23andMe Is Using Customers’ Genetic Data to Develop Drugs. Is This Brilliant or Dubious?

A woman does a DNA test with a cotton swab at home.
Leading direct-to-consumer (DTC) genetic testing companies are continuously unveiling novel ways to leverage their vast stores of genetic data.
"23andMe will tell you what diseases you have and then sell you the drugs to treat them."
As reported last week, 23andMe's latest concept is to develop and license new drugs using the data of consumers who have opted in to let their information be used for research. To date, over 10 million people have used the service and around 80 percent have opted in, making its database one of the largest in the world.
Culture researcher Dr. Julia Creet is one of the foremost experts on the DTC genetic testing industry, and in her forthcoming book, The Genealogical Sublime, she bluntly examines whether such companies' motives and interests are in sync with those of consumers.
Leapsmag caught up with Creet about the latest news and the wider industry's implications for health and privacy.
23andMe has just announced that it plans to license a newly developed anti-inflammatory drug, the first one created using its customers' genetic data, to Almirall, a pharma company in Spain. What's your take?
I think this development is the next step in the evolution of the company and its "double-sided" marketing model. In the past, as it enticed customers to give it their DNA, it sold the results and the medical information divulged by customers to other drug companies. Now it is positioning itself to reap the profits of a new model by developing treatments itself.
Given that there are many anti-inflammatory drugs on the market already, whatever Almirall produces might not have much of an impact. We might see this canny move as a "proof of concept," that 23andMe has learned how to "leverage" its genetic data without having to sell them to a third party. In a way, the privacy provisions will be much less complicated, and the company stands to attract investment as it turns itself into [a pseudo pharmaceutical company], a "pharma-psuedocal" company.
Emily Drabant Conley, the president of business development, has said that 23andMe is pursuing other drug compounds and may conduct their own clinical trials rather than licensing them out to their existing research partners. The end goal, it seems, is to make direct-to-consumer DNA testing to drug production and sales back to that same consumer base a seamless and lucrative circle. You have to admit it's a brilliant business model. 23andMe will tell you what diseases you have and then sell you the drugs to treat them.
In your new book, you describe how DTC genetic testing companies have capitalized on our innate human desire to connect with or ancestors and each other. I quote you: "This industry has taken that potent, spiritual, all-too-human need to belong... and monetized it in a particularly exploitative way." But others argue that DTC genetic testing companies are merely providing a service in exchange for fair-market compensation. So where does exploitation come into the picture?
Yes, the industry provides a fee for service, but that's only part of the story. The rest of the story reveals a pernicious industry that hides its business model behind the larger science project of health and heredity. All of the major testing companies play on the idea of "lack," that we can't know who we are unless we buy information about ourselves. When you really think about it, "Who do you think you are?" is a pernicious question that suggests that we don't or can't know who we or to whom we are related without advanced data searches and testing. This existential question used to be a philosophical question; now the answers are provided by databases that acquire more valuable information than they provide in the exchange.
"It's a brilliant business model that exploits consumer naiveté."
As you've said before, consumers are actually paying to be the product because the companies are likely to profit more from selling their genetic data. Could you elaborate?
The largest databases, AncestryDNA and 23andMe, have signed lucrative agreements with biotech companies that pay them for the de-identified data of their customers. What's so valuable is the DNA combined with the family relationships. Consumers provide the family relationships and the companies link and extrapolate the results to larger and larger family trees. Combined with the genetic markers for certain diseases, or increased susceptibility to certain diseases, these databases are very valuable for biotech research.
None of that value will ever be returned to consumers except in the form of for-profit drugs. Ancestry, in particular, has removed all information about its "research partners" from its website, making it very difficult to see how it is profiting from its third-party sales. 23andMe is more open about its "two-sided business model," but encourages consumers to donate their information to science. It's a brilliant business model that exploits consumer naiveté.
A WIRED journalist wrote that "23andMe has been sharing insights gleaned from consented customer data with GSK and at least six other pharmaceutical and biotechnology firms for the past three and a half years." Is this a consumer privacy risk?
I don't see that 23andMe did anything to which consumers didn't consent, albeit through arguably unreadable terms and conditions. The part that worries me more is the 300 phenotype data points that the company has collected on its consumers through longitudinal surveys designed, as Anne Wojcicki, CEO and Co-founder of 23andMe, put it, "to circumvent medical records and just self-report."
Everyone is focused on the DNA, but it's the combination of genetic samples, genealogical information and health records that is the most potent dataset, and 23andMe has figured out a way to extract all three from consumers.
Thanks to safety cautions from the COVID-19 pandemic, a strain of influenza has been completely eliminated.
If you were one of the millions who masked up, washed your hands thoroughly and socially distanced, pat yourself on the back—you may have helped change the course of human history.
Scientists say that thanks to these safety precautions, which were introduced in early 2020 as a way to stop transmission of the novel COVID-19 virus, a strain of influenza has been completely eliminated. This marks the first time in human history that a virus has been wiped out through non-pharmaceutical interventions, such as vaccines.
The flu shot, explained
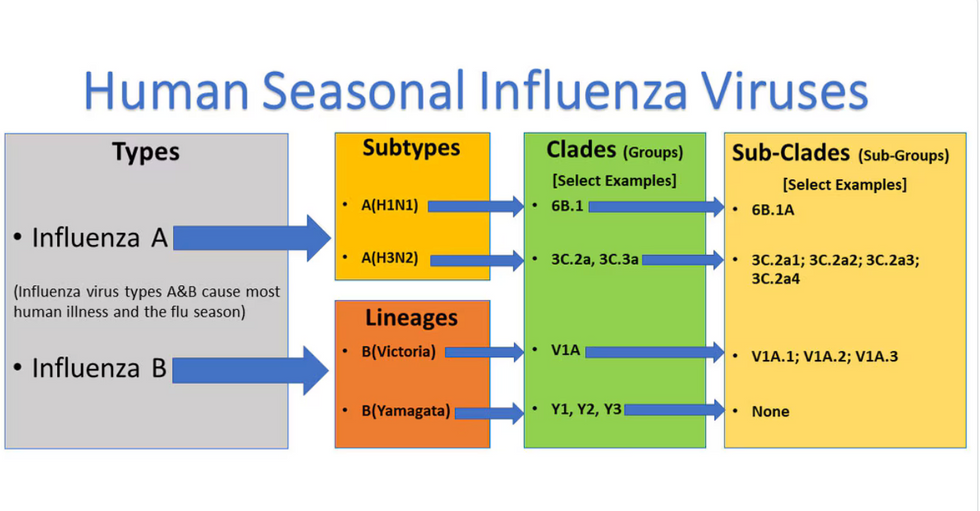
Influenza viruses type A and B are responsible for the majority of human illnesses and the flu season.
Centers for Disease Control
For more than a decade, flu shots have protected against two types of the influenza virus–type A and type B. While there are four different strains of influenza in existence (A, B, C, and D), only strains A, B, and C are capable of infecting humans, and only A and B cause pandemics. In other words, if you catch the flu during flu season, you’re most likely sick with flu type A or B.
Flu vaccines contain inactivated—or dead—influenza virus. These inactivated viruses can’t cause sickness in humans, but when administered as part of a vaccine, they teach a person’s immune system to recognize and kill those viruses when they’re encountered in the wild.
Each spring, a panel of experts gives a recommendation to the US Food and Drug Administration on which strains of each flu type to include in that year’s flu vaccine, depending on what surveillance data says is circulating and what they believe is likely to cause the most illness during the upcoming flu season. For the past decade, Americans have had access to vaccines that provide protection against two strains of influenza A and two lineages of influenza B, known as the Victoria lineage and the Yamagata lineage. But this year, the seasonal flu shot won’t include the Yamagata strain, because the Yamagata strain is no longer circulating among humans.
How Yamagata Disappeared

Flu surveillance data from the Global Initiative on Sharing All Influenza Data (GISAID) shows that the Yamagata lineage of flu type B has not been sequenced since April 2020.
Nature
Experts believe that the Yamagata lineage had already been in decline before the pandemic hit, likely because the strain was naturally less capable of infecting large numbers of people compared to the other strains. When the COVID-19 pandemic hit, the resulting safety precautions such as social distancing, isolating, hand-washing, and masking were enough to drive the virus into extinction completely.
Because the strain hasn’t been circulating since 2020, the FDA elected to remove the Yamagata strain from the seasonal flu vaccine. This will mark the first time since 2012 that the annual flu shot will be trivalent (three-component) rather than quadrivalent (four-component).
Should I still get the flu shot?
The flu shot will protect against fewer strains this year—but that doesn’t mean we should skip it. Influenza places a substantial health burden on the United States every year, responsible for hundreds of thousands of hospitalizations and tens of thousands of deaths. The flu shot has been shown to prevent millions of illnesses each year (more than six million during the 2022-2023 season). And while it’s still possible to catch the flu after getting the flu shot, studies show that people are far less likely to be hospitalized or die when they’re vaccinated.
Another unexpected benefit of dropping the Yamagata strain from the seasonal vaccine? This will possibly make production of the flu vaccine faster, and enable manufacturers to make more vaccines, helping countries who have a flu vaccine shortage and potentially saving millions more lives.
After his grandmother’s dementia diagnosis, one man invented a snack to keep her healthy and hydrated.
Founder Lewis Hornby and his grandmother Pat, sampling Jelly Drops—an edible gummy containing water and life-saving electrolytes.
On a visit to his grandmother’s nursing home in 2016, college student Lewis Hornby made a shocking discovery: Dehydration is a common (and dangerous) problem among seniors—especially those that are diagnosed with dementia.
Hornby’s grandmother, Pat, had always had difficulty keeping up her water intake as she got older, a common issue with seniors. As we age, our body composition changes, and we naturally hold less water than younger adults or children, so it’s easier to become dehydrated quickly if those fluids aren’t replenished. What’s more, our thirst signals diminish naturally as we age as well—meaning our body is not as good as it once was in letting us know that we need to rehydrate. This often creates a perfect storm that commonly leads to dehydration. In Pat’s case, her dehydration was so severe she nearly died.
When Lewis Hornby visited his grandmother at her nursing home afterward, he learned that dehydration especially affects people with dementia, as they often don’t feel thirst cues at all, or may not recognize how to use cups correctly. But while dementia patients often don’t remember to drink water, it seemed to Hornby that they had less problem remembering to eat, particularly candy.

Hornby wanted to create a solution for elderly people who struggled keeping their fluid intake up. He spent the next eighteen months researching and designing a solution and securing funding for his project. In 2019, Hornby won a sizable grant from the Alzheimer’s Society, a UK-based care and research charity for people with dementia and their caregivers. Together, through the charity’s Accelerator Program, they created a bite-sized, sugar-free, edible jelly drop that looked and tasted like candy. The candy, called Jelly Drops, contained 95% water and electrolytes—important minerals that are often lost during dehydration. The final product launched in 2020—and was an immediate success. The drops were able to provide extra hydration to the elderly, as well as help keep dementia patients safe, since dehydration commonly leads to confusion, hospitalization, and sometimes even death.
Not only did Jelly Drops quickly become a favorite snack among dementia patients in the UK, but they were able to provide an additional boost of hydration to hospital workers during the pandemic. In NHS coronavirus hospital wards, patients infected with the virus were regularly given Jelly Drops to keep their fluid levels normal—and staff members snacked on them as well, since long shifts and personal protective equipment (PPE) they were required to wear often left them feeling parched.
In April 2022, Jelly Drops launched in the United States. The company continues to donate 1% of its profits to help fund Alzheimer’s research.

