A Million Patients Have Innovated Their Own Medical Solutions, And Doctors Are Terrified

Diabetes patient advocate Renza Scibilia with her continuous glucose monitor, used in innovative DIY health technology.
In the fall of 2017, patient advocate Renza Scibilia told a conference of endocrinologists in Australia about new, patient-developed artificial pancreas technology that helped her manage her Type 1 diabetes.
"Because it's not a regulated product, some [doctors] were worried and said 'What if it goes wrong?'"
"They were in equal measure really interested and really scared," recalled Scibilia. "Because it's not a regulated product, some were worried and said 'What if it goes wrong? What is my liability going to be?'"
That was two years ago. Asked if physicians have been more receptive to the same "looping" technology now that its benefits have been supported by considerable data (as Leapsmag pointed out in May), Scibilia said, "No. Clinicians are still really insecure. They're always going to be reluctant to accept consumer-driven technology."
This exemplifies a major challenge to the growing Do-It-Yourself (DIY) biohealth movement: physicians are unnerved and worried about innovations developed by patients and other consumers that haven't been tested in elaborate clinical trials or sanctioned by regulatory authorities.
"It's difficult for patients who develop new health technology to demonstrate the advantage in a way that physicians would accept." said Howard DeMonaco, visiting scientist at MIT's Sloan School of Management. "New approaches to the treatment of diseases are by definition suspect to clinicians. Most are risk averse unless there is a substantial advantage to the new approach and the risks in doing so appear to be minimized."
Nevertheless, the DIY biohealth movement is booming. About a million people reported that they created medical innovations to address their own medical needs in surveys conducted from 2010-2015 in the U.S., U.K., Finland, Canada and South Korea.
Add in other DIY health innovations created in homes, community biolabs and "Maker" health fairs, and it's clear that health care providers are increasingly confronted with medical devices, information technology, and even medications that were developed in unconventional settings and lack the blessing of regulatory authorities.
Researchers in Portugal have tried to spread the word about many of these solutions on the Patent Innovations website, which has more than 500 examples, ranging from a 3-D printed arm and hand to a sensor device that warns someone when an osteomy bag is full.
When Reddit asked medical professionals, "What is the craziest DIY health treatment you've seen a patient attempt?" thousands shared horror stories.
But even in this era of patient empowerment, more widespread use of DIY health solutions still depends upon the approval and cooperation of physicians, nurses and other caregivers. And health care providers still lack awareness of promising patient-developed innovations, according to Dr. Joyce Lee, a pediatric endocrinologist at the University of Michigan who advocates involving patients in the design of healthcare technology. "Most physicians are scared of what they don't know," she said.
They're also understandably worried about patients who don't know what they're doing and make irresponsible decisions. When Reddit asked medical professionals, "What is the craziest DIY health treatment you've seen a patient attempt?" thousands shared horror stories, including a man who poked a hole in his belly button with a knitting needle to relieve gas.
Yet DeMonaco and Lee think it's possible to start bridging the gaps between responsible patient innovators and skeptical doctors as well as unprepared regulatory systems.
One obstacle to consumer-driven health innovations is that clinical trials to prove their safety and effectiveness are expensive and time-consuming, as De Monaco points out in a recent article. He and his colleagues suggested that low-cost clinical trials by and for patients could help address this challenge. They urged patients to publish their own research and detail the impact of innovations on their own health, and create databases that incorporate the findings of other patients.
For example, Adam Brown, who has Type 1 diabetes, compared the effects of low and high carbohydrate diets on his blood sugar management, and conveyed the results in an online journal. "Sharing the information allowed others to copy the experiment," the article noted, suggesting that this could be a model to create multi-patient trials that could be "analyzed by expert patients and/or by professionals."
Asked how to convince health care providers to consider such research, DeMonaco cited the example of doctors prescribing "off label" drugs for purposes that aren't approved by the FDA. "The secret to off label use, like any other user innovation, is dissemination," he said. Sharing case reports and other low-cost research serves to disseminate the information "in a way that is comfortable for physicians," he said, and urged patient innovators to take the same approach.
The FDA regulates commercial products and has no authority if consumers want to use medical devices, medications, or information systems that they find on their own.
Physicians should also be encouraged to engage in patient-driven research, said Dr. Lee. She suggests forming "maker spaces in which patients and physicians are involved in designing personalized technology for chronic diseases. In my vision, patient peers would build, iterate, and learn from each other and the doctor would be part of the team, constantly assessing and evaluating the technology and facilitating the process."
Some kind of regulatory oversight of DIY health technology is also necessary, said Todd Kuiken, senior research scholar at NC State and former principal investigator at the Woodrow Wilson Center's Synthetic Biology Project.
The FDA regulates commercial products and has no authority if consumers want to use medical devices, medications, or information systems that they find on their own. But that doesn't stop regulators from worrying about patients who use them. For example, the FDA issued a warning about diabetes looping technology earlier this year after one diabetic was hospitalized with hypoglycemia.
Kuiken, for one, believes that citizen-driven innovation requires oversight "to move forward." He suggested that Internal Review Boards, with experts on medical technology, safety and ethics, could play a helpful role in validating the work of patient innovators and others engaged in DIY health research. "As people are developing health products, there would be experts available to take a look and check in," he said.
Kuiken pointed out that in native American territories, tribally based IRBs working with the national Indian Health Services help to oversee new health science research. The model could be applied more broadly.
He also offered hope to those who want to integrate the current health regulatory structure into the ecosystem of DIY health innovations. "I didn't expect people from the FDA or NIH to show up" he said about a workshop on citizen-driven biomedical research that he helped organize at the Wilson Center last year. But senior officials from both agencies attended.
He indicated they "were open to new ideas." While he wouldn't disclose contributions made by individual participants in the workshop, he said the government staffers were "very interested in figuring out how to engage with citizen health innovators, to build bridges with the DIY community."
"Why should we wait for regulatory bodies? Why wait for trials that take too long?"
Time will tell whether those bridges will be built quickly enough to increase the comfort of physicians with health innovations developed by patients and other consumers. In the meantime, DIY health innovators like patient advocate Scibilia are undeterred.
"Why should we wait for regulatory bodies?" she asked. "Why wait for trials that take too long? There are plenty of data out there indicating the [diabetes looping] technology works. So we're just going to do it. We're not waiting."
A robot server, controlled remotely by a disabled worker, delivers drinks to patrons at the DAWN cafe in Tokyo.
A sleek, four-foot tall white robot glides across a cafe storefront in Tokyo’s Nihonbashi district, holding a two-tiered serving tray full of tea sandwiches and pastries. The cafe’s patrons smile and say thanks as they take the tray—but it’s not the robot they’re thanking. Instead, the patrons are talking to the person controlling the robot—a restaurant employee who operates the avatar from the comfort of their home.
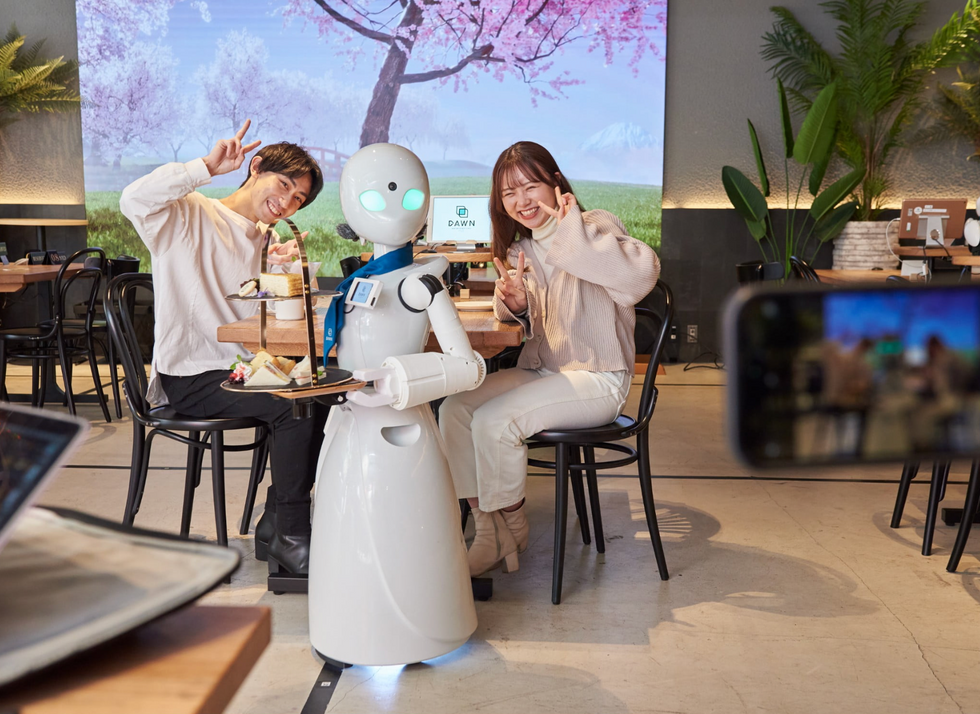
It’s a typical scene at DAWN, short for Diverse Avatar Working Network—a cafe that launched in Tokyo six years ago as an experimental pop-up and quickly became an overnight success. Today, the cafe is a permanent fixture in Nihonbashi, staffing roughly 60 remote workers who control the robots remotely and communicate to customers via a built-in microphone.
More than just a creative idea, however, DAWN is being hailed as a life-changing opportunity. The workers who control the robots remotely (known as “pilots”) all have disabilities that limit their ability to move around freely and travel outside their homes. Worldwide, an estimated 16 percent of the global population lives with a significant disability—and according to the World Health Organization, these disabilities give rise to other problems, such as exclusion from education, unemployment, and poverty.
These are all problems that Kentaro Yoshifuji, founder and CEO of Ory Laboratory, which supplies the robot servers at DAWN, is looking to correct. Yoshifuji, who was bedridden for several years in high school due to an undisclosed health problem, launched the company to help enable people who are house-bound or bedridden to more fully participate in society, as well as end the loneliness, isolation, and feelings of worthlessness that can sometimes go hand-in-hand with being disabled.
“It’s heartbreaking to think that [people with disabilities] feel they are a burden to society, or that they fear their families suffer by caring for them,” said Yoshifuji in an interview in 2020. “We are dedicating ourselves to providing workable, technology-based solutions. That is our purpose.”

Shota, Kuwahara, a DAWN employee with muscular dystrophy, agrees. "There are many difficulties in my daily life, but I believe my life has a purpose and is not being wasted," he says. "Being useful, able to help other people, even feeling needed by others, is so motivational."
A woman receives a mammogram, which can detect the presence of tumors in a patient's breast.
When a patient is diagnosed with early-stage breast cancer, having surgery to remove the tumor is considered the standard of care. But what happens when a patient can’t have surgery?
Whether it’s due to high blood pressure, advanced age, heart issues, or other reasons, some breast cancer patients don’t qualify for a lumpectomy—one of the most common treatment options for early-stage breast cancer. A lumpectomy surgically removes the tumor while keeping the patient’s breast intact, while a mastectomy removes the entire breast and nearby lymph nodes.
Fortunately, a new technique called cryoablation is now available for breast cancer patients who either aren’t candidates for surgery or don’t feel comfortable undergoing a surgical procedure. With cryoablation, doctors use an ultrasound or CT scan to locate any tumors inside the patient’s breast. They then insert small, needle-like probes into the patient's breast which create an “ice ball” that surrounds the tumor and kills the cancer cells.
Cryoablation has been used for decades to treat cancers of the kidneys and liver—but only in the past few years have doctors been able to use the procedure to treat breast cancer patients. And while clinical trials have shown that cryoablation works for tumors smaller than 1.5 centimeters, a recent clinical trial at Memorial Sloan Kettering Cancer Center in New York has shown that it can work for larger tumors, too.
In this study, doctors performed cryoablation on patients whose tumors were, on average, 2.5 centimeters. The cryoablation procedure lasted for about 30 minutes, and patients were able to go home on the same day following treatment. Doctors then followed up with the patients after 16 months. In the follow-up, doctors found the recurrence rate for tumors after using cryoablation was only 10 percent.
For patients who don’t qualify for surgery, radiation and hormonal therapy is typically used to treat tumors. However, said Yolanda Brice, M.D., an interventional radiologist at Memorial Sloan Kettering Cancer Center, “when treated with only radiation and hormonal therapy, the tumors will eventually return.” Cryotherapy, Brice said, could be a more effective way to treat cancer for patients who can’t have surgery.
“The fact that we only saw a 10 percent recurrence rate in our study is incredibly promising,” she said.

