A Surprising Breakthrough Will Allow Tiny Implants to Fix—and Even Upgrade—Your Body

The medical implants of the future will prompt lively discussion around the boundaries between treatment and enhancement.
Imagine it's the year 2040 and you're due for your regular health checkup. Time to schedule your next colonoscopy, Pap smear if you're a woman, and prostate screen if you're a man.
"The evolution of the biological ion transistor technology is a game changer."
But wait, you no longer need any of those, since you recently got one of the new biomed implants – a device that integrates seamlessly with body tissues, because of a watershed breakthrough that happened in the early 2020s. It's an improved biological transistor driven by electrically charged particles that move in and out of your own cells. Like insulin pumps and cardiac pacemakers, the medical implants of the future will go where they are needed, on or inside the body.
But unlike current implants, biological transistors will have a remarkable range of applications. Currently small enough to fit between a patient's hair follicles, the devices could one day enable correction of problems ranging from damaged heart muscle to failing retinas to deficiencies of hormones and enzymes.
Their usefulness raises the prospect of overcorrection to the point of human enhancement, as in the bionic parts that were imagined on the ABC television series The Six Million Dollar Man, which aired in the 1970s.
"The evolution of the biological ion transistor technology is a game changer," says Zoltan Istvan, who ran as a U.S. Presidential candidate in 2016 for the Transhumanist Party and later ran for California governor. Istvan envisions humans becoming faster, stronger, and increasingly more capable by way of technological innovations, especially in the biotechnology realm. "It's a big step forward on how we can improve and upgrade the human body."
How It Works
The new transistors are more like the soft, organic machines that biology has evolved than like traditional transistors built of semiconductors and metal, according to electric engineering expert Dion Khodagholy, one of the leaders of the team at Columbia University that developed the technology.
The key to the advance, notes Khodagholy, is that the transistors will interface seamlessly with tissue, because the electricity will be of the biological type -- transmitted via the flow of ions through liquid, rather than electrons through metal. This will boost the sensitivity of detection and decoding of biological change.
Naturally, such a paradigm change in the world of medical devices raises potential societal and ethical dilemmas.
Known as an ion-gated transistor (IGT), the new class of technology effectively melds electronics with molecules of human skin. That's the current prototype, but ultimately, biological devices will be able to go anywhere in the body. "IGT-based devices hold great promise for development of fully implantable bioelectronic devices that can address key clinical issues for patients with neuropsychiatric disease," says Khodagholy, based on the expectation that future devices could fuse with, measure, and modulate cells of the human nervous system.
Ethical Implications
Naturally, such a paradigm change in the world of medical devices raises potential societal and ethical dilemmas, starting with who receives the new technology and who pays for it. But, according clinical ethicist and health care attorney David Hoffman, we can gain insight from past experience, such as how society reacted to the invention of kidney dialysis in the mid 20th century.
"Kidney dialysis has been federally funded for all these decades, largely because the who-gets-the-technology question was an issue when the technology entered clinical medicine," says Hoffman, who teaches bioethics at Columbia's College of Physicians and Surgeons as well as at the law school and medical school of Yeshiva University. Just as dialysis became a necessity for many patients, he suggests that the emerging bio-transistors may also become critical life-sustaining devices, prompting discussions about federal coverage.
But unlike dialysis, biological transistors could allow some users to become "better than well," making it more similar to medication for ADHD (attention deficit hyperactivity disorder): People who don't require it can still use it to improve their baseline normal functioning. This raises the classic question: Should society draw a line between treatment and enhancement? And who gets to decide the answer?
If it's strictly a medical use of the technology, should everyone who needs it get to use it, regardless of ability to pay, relying on federal or private insurance coverage? On the other hand, if it's used voluntarily for enhancement, should that option also be available to everyone -- but at an upfront cost?
From a transhumanist viewpoint, getting wrapped up with concerns about the evolution of devices from therapy to enhancement is not worth the trouble.
It seems safe to say that some lively debates and growing pains are on the horizon.
"Even if [the biological ion transistor] is developed only for medical devices that compensate for losses and deficiencies similar to that of a cardiac pacemaker, it will be hard to stop its eventual evolution from compensation to enhancement," says Istvan. "If you use it in a bionic eye to restore vision to the blind, how do you draw the line between replacement of normal function and provision of enhanced function? Do you pass a law placing limits on visual capabilities of a synthetic eye? Transhumanists would oppose such laws, and any restrictions in one country or another would allow another country to gain an advantage by creating their own real-life super human cyborg citizens."
In the same breath though, Istvan admits that biotechnology on a bionic scale is bound to complicate a range of international phenomena, from economic growth and military confrontations to sporting events like the Olympic Games.
The technology is already here, and it's just a matter of time before we see clinically viable, implantable devices. As for how society will react, it seems safe to say that some lively debates and growing pains are on the horizon.
A robot server, controlled remotely by a disabled worker, delivers drinks to patrons at the DAWN cafe in Tokyo.
A sleek, four-foot tall white robot glides across a cafe storefront in Tokyo’s Nihonbashi district, holding a two-tiered serving tray full of tea sandwiches and pastries. The cafe’s patrons smile and say thanks as they take the tray—but it’s not the robot they’re thanking. Instead, the patrons are talking to the person controlling the robot—a restaurant employee who operates the avatar from the comfort of their home.
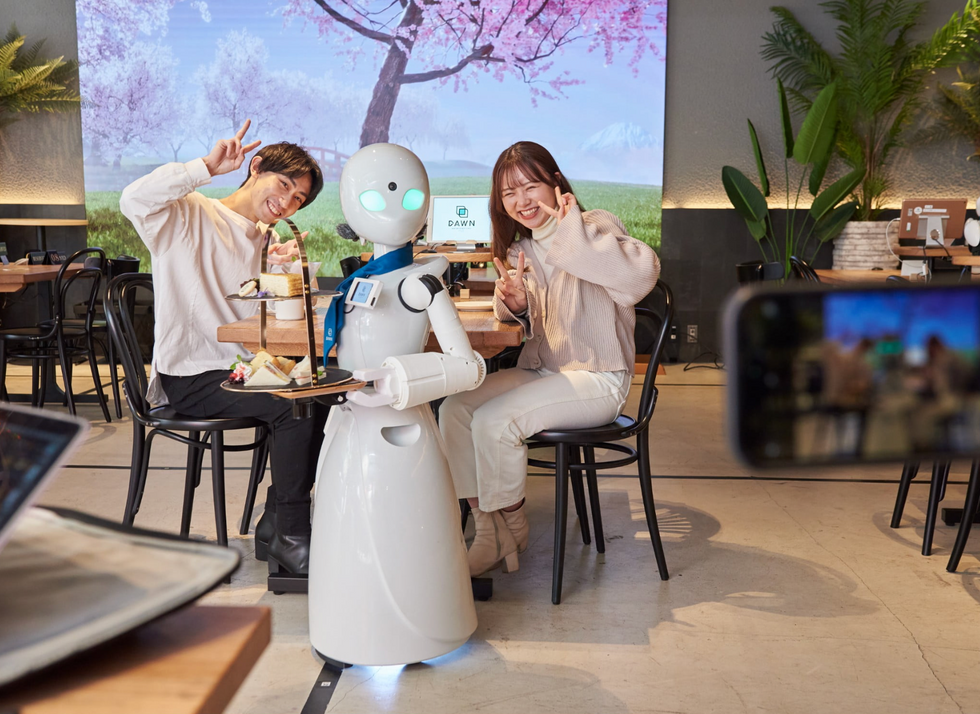
It’s a typical scene at DAWN, short for Diverse Avatar Working Network—a cafe that launched in Tokyo six years ago as an experimental pop-up and quickly became an overnight success. Today, the cafe is a permanent fixture in Nihonbashi, staffing roughly 60 remote workers who control the robots remotely and communicate to customers via a built-in microphone.
More than just a creative idea, however, DAWN is being hailed as a life-changing opportunity. The workers who control the robots remotely (known as “pilots”) all have disabilities that limit their ability to move around freely and travel outside their homes. Worldwide, an estimated 16 percent of the global population lives with a significant disability—and according to the World Health Organization, these disabilities give rise to other problems, such as exclusion from education, unemployment, and poverty.
These are all problems that Kentaro Yoshifuji, founder and CEO of Ory Laboratory, which supplies the robot servers at DAWN, is looking to correct. Yoshifuji, who was bedridden for several years in high school due to an undisclosed health problem, launched the company to help enable people who are house-bound or bedridden to more fully participate in society, as well as end the loneliness, isolation, and feelings of worthlessness that can sometimes go hand-in-hand with being disabled.
“It’s heartbreaking to think that [people with disabilities] feel they are a burden to society, or that they fear their families suffer by caring for them,” said Yoshifuji in an interview in 2020. “We are dedicating ourselves to providing workable, technology-based solutions. That is our purpose.”

Shota, Kuwahara, a DAWN employee with muscular dystrophy, agrees. "There are many difficulties in my daily life, but I believe my life has a purpose and is not being wasted," he says. "Being useful, able to help other people, even feeling needed by others, is so motivational."
A woman receives a mammogram, which can detect the presence of tumors in a patient's breast.
When a patient is diagnosed with early-stage breast cancer, having surgery to remove the tumor is considered the standard of care. But what happens when a patient can’t have surgery?
Whether it’s due to high blood pressure, advanced age, heart issues, or other reasons, some breast cancer patients don’t qualify for a lumpectomy—one of the most common treatment options for early-stage breast cancer. A lumpectomy surgically removes the tumor while keeping the patient’s breast intact, while a mastectomy removes the entire breast and nearby lymph nodes.
Fortunately, a new technique called cryoablation is now available for breast cancer patients who either aren’t candidates for surgery or don’t feel comfortable undergoing a surgical procedure. With cryoablation, doctors use an ultrasound or CT scan to locate any tumors inside the patient’s breast. They then insert small, needle-like probes into the patient's breast which create an “ice ball” that surrounds the tumor and kills the cancer cells.
Cryoablation has been used for decades to treat cancers of the kidneys and liver—but only in the past few years have doctors been able to use the procedure to treat breast cancer patients. And while clinical trials have shown that cryoablation works for tumors smaller than 1.5 centimeters, a recent clinical trial at Memorial Sloan Kettering Cancer Center in New York has shown that it can work for larger tumors, too.
In this study, doctors performed cryoablation on patients whose tumors were, on average, 2.5 centimeters. The cryoablation procedure lasted for about 30 minutes, and patients were able to go home on the same day following treatment. Doctors then followed up with the patients after 16 months. In the follow-up, doctors found the recurrence rate for tumors after using cryoablation was only 10 percent.
For patients who don’t qualify for surgery, radiation and hormonal therapy is typically used to treat tumors. However, said Yolanda Brice, M.D., an interventional radiologist at Memorial Sloan Kettering Cancer Center, “when treated with only radiation and hormonal therapy, the tumors will eventually return.” Cryotherapy, Brice said, could be a more effective way to treat cancer for patients who can’t have surgery.
“The fact that we only saw a 10 percent recurrence rate in our study is incredibly promising,” she said.

