Editor's Note: A team of researchers in Italy recently used artificial intelligence and machine learning to diagnose Alzheimer's disease on a brain scan an entire decade before symptoms show up in the patient. While some people argue that early detection is critical, others believe the knowledge would do more harm than good. LeapsMag invited contributors with opposite opinions to share their perspectives.
Alzheimer's doesn't run in my family. When my father was diagnosed at the age of 58, we looked at his familial history. Both his parents lived into their late 80's. All of their surviving siblings were similarly long-lived and none had had Alzheimer's or any related dementias. My dad had spent 20 years working for the United Nations in the 60's and 70's in Africa. He was convinced that the Alzheimer's had come from his time spent in dodgy mines where he was exposed without the proper protections to all kinds of chemical processes.
Maybe that was true. Maybe it wasn't. The theory that metals, particularly aluminum, is an environmental factor leading to Alzheimer's has been around for a while. It's mostly been debunked, but clearly something is causing this epidemic as the vast majority of the cases in the world today are age-related. But no one knows what the trigger is, nor are we close to knowing.
If my father had had the Alzheimer's gene, I would go get myself checked for it. If some new MRI were commercially available to scan my brain and let me know if I was developing Alzheimer's, I would also take that test. There are four reasons why.
First, studies have shown that lifestyle has a major impact on the disease. I already run three miles a day. I eat relatively healthily. But like anyone, I don't live strictly on boiled chicken and broccoli. And I definitely enjoy a glass of wine or two. If I knew I had a propensity for the disease, or was developing it, I would be more diligent. I would eat my broccoli and cut out my wine. Life would be less fun, but I'd get more life and that's what's important.
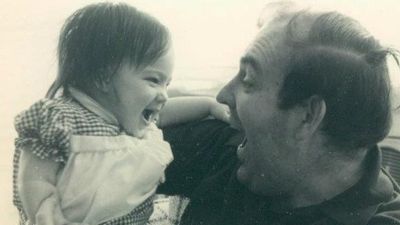
The last picture taken of the author with her father before his death, in 2015.
Secondly, I would also have time to create an end-of-life plan the way my father did not. He told me repeatedly early on in his diagnosis that he did not want to live when he no longer knew me, when he became a burden, when he couldn't feed or bathe himself. I did my best in his final years to help him die quicker: I know that was what he wanted. But, given U.S. laws, all that meant was taking him off his heart and stroke medications and letting him eat anything he wanted, no matter how unhealthy. Knowing what's to come, having seen him go through it, I might consider moving to Belgium, which has begun to allow assisted suicide of those living with Alzheimer's and dementia if they can clearly state their intentions early on in the disease when they still have clarity of mind.
Next, I could help. Right now, there are dozens of Alzheimer's and dementia studies in the works. They are short thousands of willing test subjects. One of the top barriers to learning what's triggering the disease, and finding a cure, is populating these studies. So, knowing would make me a stronger candidate and would potentially help others down the road.
Finally, it would change my priorities. My father died the longest death possible: he succumbed last year more than 15 years after his diagnosis. My mother died the quickest possible way: she had a stress-related brain aneurysm 10 years after my father's diagnosis. Caring for him was too much for her and aneurysms ran in her family; her mother died of one as well. I already get a scan once every five years to see if I'm developing a brain aneurysm. If I am, odds are only 66% that they can operate on it—some aneurysms develop much too deep in the brain to operate, like my mother's.
Would she have wanted to know? Even though the aneurysm in her case was inoperable? I'm not sure. But I imagine if she had known, she would've lived her final years differently. She might have taken that trip to Alaska that she debated but thought was too expensive. She might have gotten organized earlier to make out a will so I wasn't left with chaos in the wake of her death; we'd planned for my father's death, knowing he was ill, but not my mother's. And she might have finally gotten around to dictating her story to me, as she'd always promised me she would when she found the time.
Telling my father's story at the end of his life helped his care.
With my startup MemoryWell, I spend my life now collecting senior stories before they are lost, in part because telling my father's story at the end of his life helped his care. But it's also in part for the story I lost with my mother.
If I knew that my time was limited, I'd not worry so much about saving for retirement. I'd make progress on my bucket list: hike Machu Picchu, scuba dive the Maldives, or raft the Grand Canyon. I'd tell my loved ones as much as I can in my time remaining how much they mean to me. And I would spend more time writing my own story to pass it down—finally finishing the book I've been working on. Maybe it's the writer in me, or maybe it's that I don't have kids of my own yet to carry on a legacy, but I'd want my story to be known, to have others learn from my experiences. And that's the biggest gift knowing would give me.
Editor's Note: Consider the other side of the argument here.