Antibody Testing Alone is Not the Key to Re-Opening Society
Immunity tests have too many unknowns right now to make them very useful in determining protective antibody status.
[Editor's Note: We asked experts from different specialties to weigh in on a timely Big Question: "How should immunity testing play a role in re-opening society?" Below, a virologist offers her perspective.]
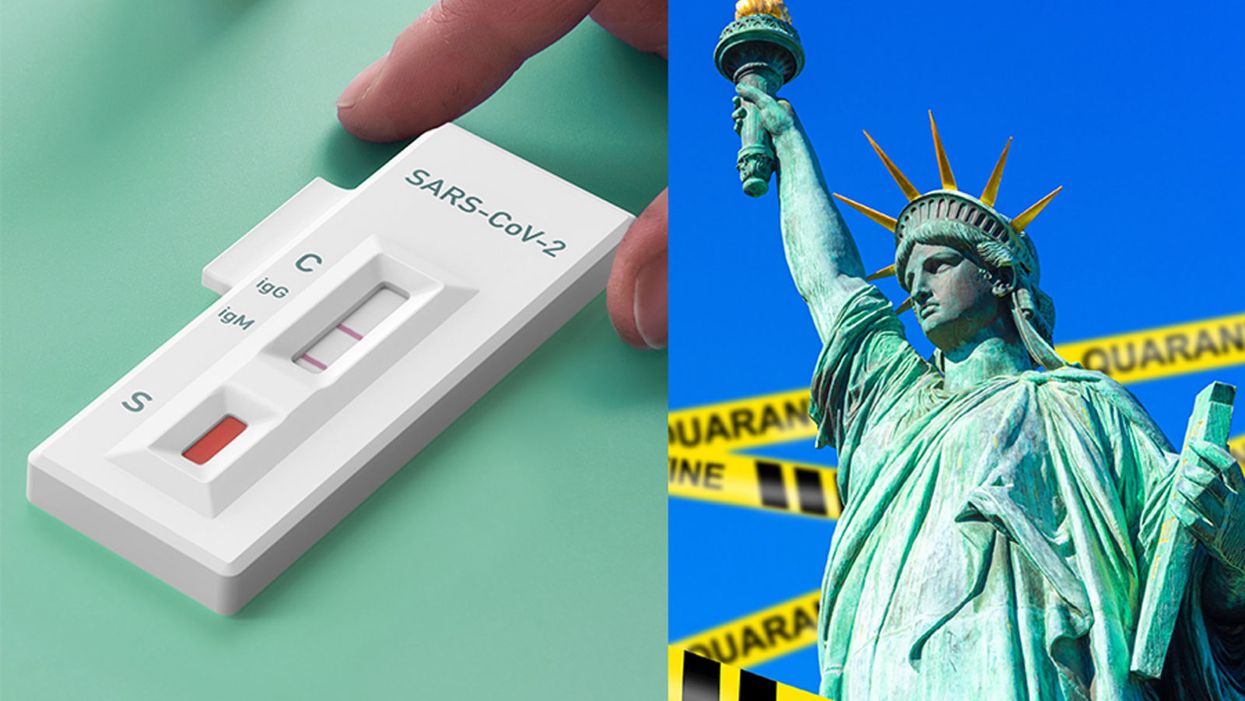
With the advent of serology testing and increased emphasis on "re-opening" America, public health officials have begun considering whether or not people who have recovered from COVID-19 can safely re-enter the workplace.
"Immunity certificates cannot certify what is not known."
Conventional wisdom holds that people who have developed antibodies in response to infection with SARS-CoV-2, the coronavirus that causes COVID-19, are likely to be immune to reinfection.
For most acute viral infections, this is generally true. However, SARS-CoV-2 is a new pathogen, and there are currently many unanswered questions about immunity. Can recovered patients be reinfected or transmit the virus? Does symptom severity determine how protective responses will be after recovery? How long will protection last? Understanding these basic features is essential to phased re-opening of the government and economy for people who have recovered from COVID-19.
One mechanism that has been considered is issuing "immunity certificates" to individuals with antibodies against SARS-CoV-2. These certificates would verify that individuals have already recovered from COVID-19, and thus have antibodies in their blood that will protect them against reinfection, enabling them to safely return to work and participate in society. Although this sounds reasonable in theory, there are many practical reasons why this is not a wise policy decision to ease off restrictive stay-home orders and distancing practices.
Too Many Scientific Unknowns
Serology tests measure antibodies in the serum—the liquid component of blood, which is where the antibodies are located. In this case, serology tests measure antibodies that specifically bind to SARS-CoV-2 virus particles. Usually when a person is infected with a virus, they develop antibodies that can "recognize" that virus, so the presence of SARS-CoV-2 antibodies indicates that a person has been previously exposed to the virus. Broad serology testing is critical to knowing how many people have been infected with SARS-CoV-2, since testing capacity for the virus itself has been so low.
Tests for the virus measure amounts of SARS-CoV-2 RNA—the virus's genetic material—directly, and thus will not detect the virus once a person has recovered. Thus, the majority of people who were not severely ill and did not require hospitalization, or did not have direct contact with a confirmed case, will not test positive for the virus weeks after they have recovered and can only determine if they had COVID-19 by testing for antibodies.
In most cases, for most pathogens, antibodies are also neutralizing, meaning they bind to the virus and render it incapable of infecting cells, and this protects against future infections. Immunity certificates are based on the assumption that people with antibodies specific for SARS-CoV-2 will be protected against reinfection. The problem is that we've only known that SARS-CoV-2 existed for a little over four months. Although studies so far indicate that most (but not all) patients with confirmed COVID-19 cases develop antibodies, we don't know the extent to which antibodies are protective against reinfection, or how long that protection will last. Immunity certificates cannot certify what is not known.
The limited data so far is encouraging with regard to protective immunity. Most of the patient sera tested for antibodies show reasonable titers of IgG, the type of antibodies most likely to be neutralizing. Furthermore, studies have shown that these IgG antibodies are capable of neutralizing surrogate viruses as well as infectious SARS-CoV-2 in laboratory tests. In addition, rhesus monkeys that were experimentally infected with SARS-CoV-2 and allowed to recover were protected from reinfection after a subsequent experimental challenge. These data tentatively suggest that most people are likely to develop neutralizing IgG, and protective immunity, after being infected by SARS-CoV-2.
However, not all COVID-19 patients do produce high levels of antibodies specific for SARS-CoV-2. A small number of patients in one study had no detectable neutralizing IgG. There have also been reports of patients in South Korea testing PCR positive after a prior negative test, indicating reinfection or reactivation. These cases may be explained by the sensitivity of the PCR test, and no data have been produced to indicate that these cases are genuine reinfection or recurrence of viral infection.
Complicating matters further, not all serology tests measure antibody titers. Some rapid serology tests are designed to be binary—the test can either detect antibodies or not, but does not give information about the amount of antibodies circulating. Based on our current knowledge, we cannot be certain that merely having any level of detectable antibodies alone guarantees protection from reinfection, or from a subclinical reinfection that might not cause a second case of COVID-19, but could still result in transmission to others. These unknowns remain problematic even with tests that accurately detect the presence of antibodies—which is not a given today, as many of the newly available tests are reportedly unreliable.
A Logistical and Ethical Quagmire
While most people are eager to cast off the isolation of physical distancing and resume their normal lives, mere desire to return to normality is not an indicator of whether those antibodies actually work, and no certificate can confer immune protection. Furthermore, immunity certificates could lead to some complicated logistical and ethical issues. If antibodies do not guarantee protective immunity, certifying that they do could give antibody-positive people a false sense of security, causing them to relax infection control practices such as distancing and hand hygiene.
"We should not, however, place our faith in assumptions and make return to normality contingent on an arbitrary and uninformative piece of paper."
Certificates could be forged, putting susceptible people at higher exposure risk. It's not clear who would issue them, what they would entitle the bearer to do or not do, or how certification would be verified or enforced. There are many ways in which such certificates could be used as a pretext to discriminate against people based on health status, in addition to disability, race, and socioeconomic status. Tracking people based on immune status raises further concerns about privacy and civil rights.
Rather than issuing documents confirming immune status, we should instead "re-open" society cautiously, with widespread virus and serology testing to accurately identify and isolate infected cases rapidly, with immediate contact tracing to safely quarantine and monitor those at exposure risk. Broad serosurveillance must be coupled with functional assays for neutralization activity to begin assessing how protective antibodies might actually be against SARS-CoV-2 infection. To understand how long immunity lasts, we should study antibodies, as well as the functional capabilities of other components of the larger immune system, such as T cells, in recovered COVID-19 patients over time.
We should not, however, place our faith in assumptions and make return to normality contingent on an arbitrary and uninformative piece of paper. Re-opening society, the government, and the economy depends not only on accurately determining how many people have antibodies to SARS-CoV-2, but on a deeper understanding of how those antibodies work to provide protection.
Recent leaps in technology represent an important step forward in unlocking artificial photosynthesis.
Since the beginning of life on Earth, plants have been naturally converting sunlight into energy. This photosynthesis process that's effortless for them has been anything but for scientists who have been trying to achieve artificial photosynthesis for the last half a century with the goal of creating a carbon-neutral fuel. Such a fuel could be a gamechanger — rather than putting CO2 back into the atmosphere like traditional fuels do, it would take CO2 out of the atmosphere and convert it into usable energy.
If given the option between a carbon-neutral fuel at the gas station and a fuel that produces carbon dioxide in spades -- and if costs and effectiveness were equal --who wouldn't choose the one best for the planet? That's the endgame scientists are after. A consumer switch to clean fuel could have a huge impact on our global CO2 emissions.
Up until this point, the methods used to make liquid fuel from atmospheric CO2 have been expensive, not efficient enough to really get off the ground, and often resulted in unwanted byproducts. But now, a new technology may be the key to unlocking the full potential of artificial photosynthesis. At the very least, it's a step forward and could help make a dent in atmospheric CO2 reduction.
"It's an important breakthrough in artificial photosynthesis," says Qian Wang, a researcher in the Department of Chemistry at Cambridge University and lead author on a recent study published in Nature about an innovation she calls "photosheets."
The latest version of the artificial leaf directly produces liquid fuel, which is easier to transport and use commercially.
These photosheets convert CO2, sunlight, and water into a carbon-neutral liquid fuel called formic acid without the aid of electricity. They're made of semiconductor powders that absorb sunlight. When in the presence of water and CO2, the electrons in the powders become excited and join with the CO2 and protons from the water molecules, reducing the CO2 in the process. The chemical reaction results in the production of formic acid, which can be used directly or converted to hydrogen, another clean energy fuel.
In the past, it's been difficult to reduce CO2 without creating a lot of unwanted byproducts. According to Wang, this new conversion process achieves the reduction and fuel creation with almost no byproducts.
The Cambridge team's new technology is a first and certainly momentous, but they're far from the only team to have produced fuel from CO2 using some form of artificial photosynthesis. More and more scientists are aiming to perfect the method in hopes of producing a truly sustainable, photosynthetic fuel capable of lowering carbon emissions.
Thanks to advancements in nanoscience, which has led to better control of materials, more successes are emerging. A team at the University of Illinois at Urbana-Champaign, for example, used gold nanoparticles as the photocatalysts in their process.
"My group demonstrated that you could actually use gold nanoparticles both as a light absorber and a catalyst in the process of converting carbon dioxide to hydrocarbons such as methane, ethane and propane fuels," says professor Prashant Jain, co-author of the study. Not only are gold nanoparticles great at absorbing light, they don't degrade as quickly as other metals, which makes them more sustainable.
That said, Jain's team, like every other research team working on artificial photosynthesis including the Cambridge team, is grappling with efficiency issues. Jain says that all parts of the process need to be optimized so the reaction can happen as quickly as possible.
"You can't just improve one [aspect], because that can lead to a decrease in performance in some other aspects," Jain explains.
The Cambridge team is currently experimenting with a range of catalysts to improve their device's stability and efficiency. Virgil Andrei, who is working on an artificial leaf design that was developed at Cambridge in 2019, was recently able to improve the performance and selectivity of the device. Now the leaf's solar-to-CO2 energy conversion efficiency is 0.2%, twice its previous efficiency.
The latest version also directly produces liquid fuel, which is easier to transport and use commercially.
In determining a method of fuel production's efficiency, one must consider how sustainable it is at every stage. That involves calculating whenever excess energy is needed to complete a step. According to Jain, in order to use CO2 for fuel production, you have to condense the CO2, which takes energy. And on the fuel production side, once the chemical reaction has created your byproducts, they need to be separated, which also takes energy.
To be truly sustainable, each part of the conversion system also needs to be durable. If parts need to be replaced often, or regularly maintained, that counts against it. Then you have to account for the system's reuse cycle. If you extract CO2 from the environment and convert it into fuel that's then put into a fuel cell, it's going to release CO2 at the other end. In order to create a fully green, carbon-neutral fuel source, that same amount of CO2 needs to be trapped and reintroduced back into the fuel conversion system.
"The cycle continues, and at each point, you will see a loss in efficiency, and depending on how much you [may also] see a loss in yield," says Jain. "And depending on what those efficiencies are at each one of those points will determine whether or not this process can be sustainable."
The science is at least a decade away from offering a competitive sustainable fuel option at scale. Streamlining a process to mimic what plants have perfected over billions of years is no small feat, but an ever-growing community of researchers using rapidly advancing technology is driving progress forward.
Genetic data sets skew too European, threatening to narrow who will benefit from future advances.
Genomics has begun its golden age. Just 20 years ago, sequencing a single genome cost nearly $3 billion and took over a decade. Today, the same feat can be achieved for a few hundred dollars and the better part of a day . Suddenly, the prospect of sequencing not just individuals, but whole populations, has become feasible.
The genetic differences between humans may seem meager, only around 0.1 percent of the genome on average, but this variation can have profound effects on an individual's risk of disease, responsiveness to medication, and even the dosage level that would work best.
Already, initiatives like the U.K.'s 100,000 Genomes Project - now expanding to 1 million genomes - and other similarly massive sequencing projects in Iceland and the U.S., have begun collecting population-scale data in order to capture and study this variation.
The resulting data sets are immensely valuable to researchers and drug developers working to design new 'precision' medicines and diagnostics, and to gain insights that may benefit patients. Yet, because the majority of this data comes from developed countries with well-established scientific and medical infrastructure, the data collected so far is heavily biased towards Western populations with largely European ancestry.
This presents a startling and fast-emerging problem: groups that are under-represented in these datasets are likely to benefit less from the new wave of therapeutics, diagnostics, and insights, simply because they were tailored for the genetic profiles of people with European ancestry.
We may indeed be approaching a golden age of genomics-enabled precision medicine. But if the data bias persists then there is a risk, as with most golden ages throughout history, that the benefits will not be equally accessible to all, and existing inequalities will only be exacerbated.
To remedy the situation, a number of initiatives have sprung up to sequence genomes of under-represented groups, adding them to the datasets and ensuring that they too will benefit from the rapidly unfolding genomic revolution.
Global Gene Corp
The idea behind Global Gene Corp was born eight years ago in Harvard when Sumit Jamuar, co-founder and CEO, met up with his two other co-founders, both experienced geneticists, for a coffee.
"They were discussing the limitless applications of understanding your genetic code," said Jamuar, a business executive from New Delhi.
"And so, being a technology enthusiast type, I was excited and I turned to them and said hey, this is incredible! Could you sequence me and give me some insights? And they actually just turned around and said no, because it's not going to be useful for you - there's not enough reference for what a good Sumit looks like."
What started as a curiosity-driven conversation on the power of genomics ended with a commitment to tackle one of the field's biggest roadblocks - its lack of global representation.
Jamuar set out to begin with India, which has about 20 percent of the world's population, including over 4000 different ethnicities, but contributes less than 2 percent of genomic data, he told Leaps.org.
Eight years later, Global Gene Corp's sequencing initiative is well underway, and is the largest in the history of the Indian subcontinent. The program is being carried out in collaboration with biotech giant Regeneron, with support from the Indian government, local communities, and the Indian healthcare ecosystem. In August 2020, Global Gene Corp's work was recognized through the $1 million 2020 Roddenberry award for organizations that advance the vision of 'Star Trek' creator Gene Roddenberry to better humanity.
This problem has already begun to manifest itself in, for example, much higher levels of genetic misdiagnosis among non-Europeans tested for their risk of certain diseases, such as hypertrophic cardiomyopathy - an inherited disease of the heart muscle.
Global Gene Corp also focuses on developing and implementing AI and machine learning tools to make sense of the deluge of genomic data. These tools are increasingly used by both industry and academia to guide future research by identifying particularly promising or clinically interesting genetic variants. But if the underlying data is skewed European, then the effectiveness of the computational analysis - along with the future advances and avenues of research that emerge from it - will be skewed towards Europeans too.
This problem has already begun to manifest itself in, for example, much higher levels of genetic misdiagnosis among non-Europeans tested for their risk of certain diseases, such as hypertrophic cardiomyopathy - an inherited disease of the heart muscle. Most of the genetic variants used in these tests were identified as being causal for the disease from studies of European genomes. However, many of these variants differ both in their distribution and clinical significance across populations, leading to many patients of non-European ancestry receiving false-positive test results - as their benign genetic variants were misclassified as pathogenic. Had even a small number of genomes from other ethnicities been included in the initial studies, these misdiagnoses could have been avoided.
"Unless we have a data set which is unbiased and representative, we're never going to achieve the success that we want," Jamuar says.
"When Siri was first launched, she could hardly recognize an accent which was not of a certain type, so if I was trying to speak to Siri, I would have to repeat myself multiple times and try to mimic an accent which wasn't my accent so that she could understand it.
"But over time the voice recognition technology improved tremendously because the training data was expanded to include people of very diverse backgrounds and their accents, so the algorithms were trained to be able to pick that up and it dramatically improved the technology. That's the way we have to think about it - without that good-quality diverse data, we will never be able to achieve the full potential of the computational tools."
While mapping India's rich genetic diversity has been the organization's primary focus so far, they plan, in time, to expand their work to other under-represented groups in Asia, the Middle East, Africa, and Latin America.
"As other like-minded people and partners join the mission, it just accelerates the achievement of what we have set out to do, which is to map out and organize the world's genomic diversity so that we can enable high-quality life and longevity benefits for everyone, everywhere," Jamuar says.
Empowering African Genomics
Africa is the birthplace of our species, and today still retains an inordinate amount of total human genetic diversity. Groups that left Africa and went on to populate the rest of the world, some 50 to 100,000 years ago, were likely small in number and only took a fraction of the total genetic diversity with them. This ancient bottleneck means that no other group in the world can match the level of genetic diversity seen in modern African populations.
Despite Africa's central importance in understanding the history and extent of human genetic diversity, the genomics of African populations remains wildly understudied. Addressing this disparity has become a central focus of the H3Africa Consortium, an initiative formally launched in 2012 with support from the African Academy of Sciences, the U.S. National Institutes of Health, and the UK's Wellcome Trust. Today, H3Africa supports over 50 projects across the continent, on an array of different research areas in genetics relevant to the health and heredity of Africans.
"Africa is the cradle of Humankind. So what that really means is that the populations that are currently living in Africa are among some of the oldest populations on the globe, and we know that the longer populations have had to go through evolutionary phases, the more variation there is in the genomes of people who live presently," says Zane Lombard, a principal investigator at H3Africa and Associate Professor of Human Genetics at the University of the Witwatersrand in Johannesburg, South Africa.
"So for that reason, African populations carry a huge amount of genetic variation and diversity, which is pretty much uncaptured. There's still a lot to learn as far as novel variation is concerned by looking at and studying African genomes."
A recent landmark H3Africa study, led by Lombard and published in Nature in October, sequenced the genomes of over 400 African individuals from 50 ethno-linguistic groups - many of which had never been sampled before.
Despite the relatively modest number of individuals sequenced in the study, over three million previously undescribed genetic variants were found, and complex patterns of ancestral migration were uncovered.
"In some of these ethno-linguistic groups they don't have a word for DNA, so we've had to really think about how to make sure that we communicate the purposes of different studies to participants so that you have true informed consent," says Lombard.
"The objective," she explained, "was to try and fill some of the gaps for many of these populations for which we didn't have any whole genome sequences or any genetic variation data...because if we're thinking about the future of precision medicine, if the patient is a member of a specific group where we don't know a lot about the genomic variation that exists in that group, it makes it really difficult to start thinking about clinical interpretation of their data."
From H3Africa's conception, the consortium's goal has not only been to better represent Africa's staggering genetic diversity in genomic data sets, but also to build Africa's domestic genomics capabilities and empower a new generation of African researchers. By doing so, the hope is that Africans will be able to set their own genomics agenda, and leapfrog to new and better ways of doing the work.
"The training that has happened on the continent and the number of new scientists, new students, and fellows that have come through the process and are now enabled to start their own research groups, to grow their own research in their countries, to be a spokesperson for genomics research in their countries, and to build that political will to do these larger types of sequencing initiatives - that is really a significant outcome from H3Africa as well. Over and above all the science that's coming out," Lombard says.
"What has been created through H3Africa is just this locus of researchers and scientists and bioethicists who have the same goal at heart - to work towards adjusting the data bias and making sure that all global populations are represented in genomics."

