Blood Money: Paying for Convalescent Plasma to Treat COVID-19
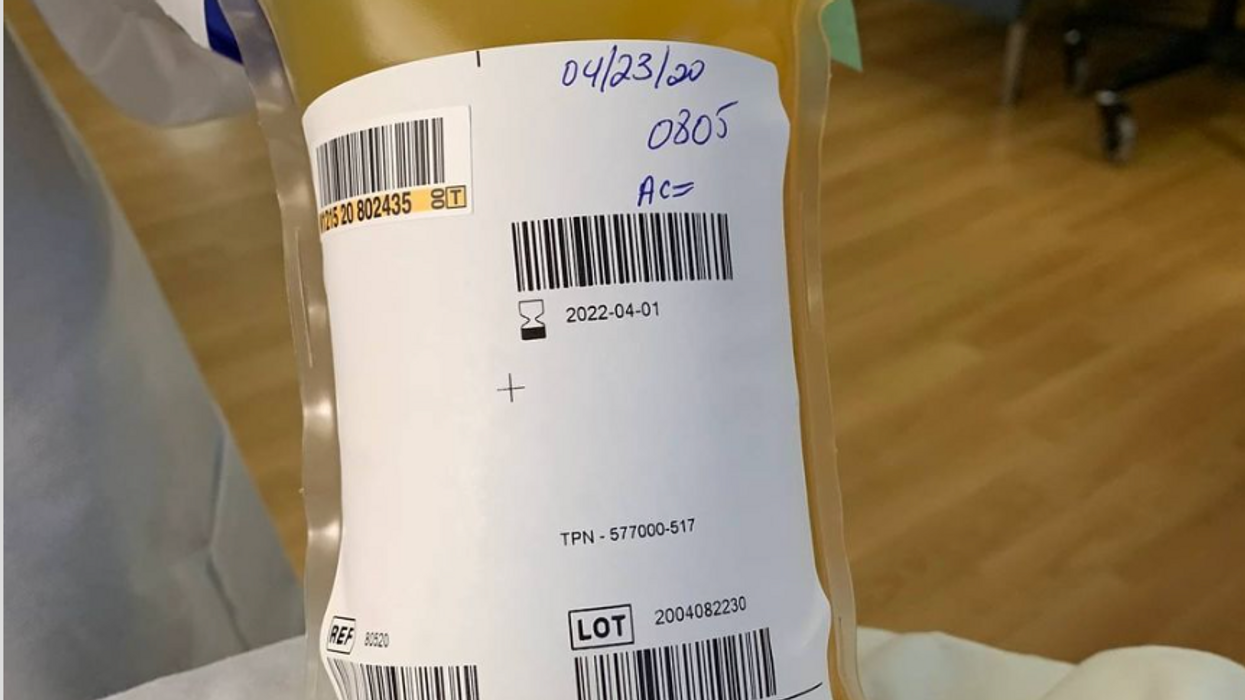
A bag of plasma that Tom Hanks donated back in April 2020 after his coronavirus infection. (He was not paid to donate.)
Convalescent plasma – first used to treat diphtheria in 1890 – has been dusted off the shelf to treat COVID-19. Does it work? Should we rely strictly on the altruism of donors or should people be paid for it?
The biologic theory is that a person who has recovered from a disease has chemicals in their blood, most likely antibodies, that contributed to their recovery, and transferring those to a person who is sick might aid their recovery. Whole blood won't work because there are too few antibodies in a single unit of blood and the body can hold only so much of it.
Plasma comprises about 55 percent of whole blood and is what's left once you take out the red blood cells that carry oxygen and the white blood cells of the immune system. Most of it is water but the rest is a complex mix of fats, salts, signaling molecules and proteins produced by the immune system, including antibodies.
A process called apheresis circulates the donors' blood through a machine that separates out the desired parts of blood and returns the rest to the donor. It takes several times the length of a regular whole blood donation to cycle through enough blood for the process. The end product is a yellowish concentration called convalescent plasma.
Recent History
It was used extensively during the great influenza epidemic off 1918 but fell out of favor with the development of antibiotics. Still, whenever a new disease emerges – SARS, MERS, Ebola, even antibiotic-resistant bacteria – doctors turn to convalescent plasma, often as a stopgap until more effective antibiotic and antiviral drugs are developed. The process is certainly safe when standard procedures for handling blood products are followed, and historically it does seem to be beneficial in at least some patients if administered early enough in the disease.
With few good treatment options for COVID-19, doctors have given convalescent plasma to more than a hundred thousand Americans and tens of thousand of people elsewhere, to mixed results. Placebo-controlled trials could give a clearer picture of plasma's value but it is difficult to enroll patients facing possible death when the flip of a coin will determine who will receive a saline solution or plasma.
And the plasma itself isn't some uniform pill stamped out in a factory, it's a natural product that is shaped by the immune history of the donor's body and its encounter not just with SARS-CoV-2 but a lifetime of exposure to different pathogens.
Researchers believe antibodies in plasma are a key factor in directly fighting the virus. But the variety and quantity of antibodies vary from donor to donor, and even over time from the same donor because once the immune system has cleared the virus from the body, it stops putting out antibodies to fight the virus. Often the quality and quantity of antibodies being given to a patient are not measured, making it somewhat hit or miss, which is why several companies have recently developed monoclonal antibodies, a single type of antibody found in blood that is effective against SARS-CoV-2 and that is multiplied in the lab for use as therapy.
Plasma may also contain other unknown factors that contribute to fighting disease, say perhaps signaling molecules that affect gene expression, which might affect the movement of immune cells, their production of antiviral molecules, or the regulation of inflammation. The complexity and lack of standardization makes it difficult to evaluate what might be working or not with a convalescent plasma treatment. Thus researchers are left with few clues about how to make it more effective.
Industrializing Plasma
Many Americans living along the border with Mexico regularly head south to purchase prescription drugs at a significant discount. Less known is the medical traffic the other way, Mexicans who regularly head north to be paid for plasma donations, which are prohibited in their country; the U.S. allows payment for plasma donations but not whole blood. A typical payment is about $35 for a donation but the sudden demand for convalescent plasma from people who have recovered from COVID-19 commands a premium price, sometimes as high as $200. These donors are part of a fast-growing plasma industry that surpassed $25 billion in 2018. The U.S. supplies about three-quarters of the world's needs for plasma.
Payment for whole blood donation in the U.S. is prohibited, and while payment for plasma is allowed, there is a stigma attached to payment and much plasma is donated for free.
The pharmaceutical industry has shied away from natural products they cannot patent but they have identified simpler components from plasma, such as clotting factors and immunoglobulins, that have been turned into useful drugs from this raw material of plasma. While some companies have retooled to provide convalescent plasma to treat COVID-19, often paying those donors who have recovered a premium of several times the normal rate, most convalescent plasma has come as donations through traditional blood centers.
In April the Mayo Clinic, in cooperation with the FDA, created an expanded access program for convalescent plasma to treat COVID-19. It was meant to reduce the paperwork associated with gaining access to a treatment not yet approved by the FDA for that disease. Initially it was supposed to be for 5000 units but it quickly grew to more than twenty times that size. Michael Joyner, the head of the program, discussed that experience in an extended interview in September.
The Centers for Medicare and Medicaid Services (CMS) also created associated reimbursement codes, which became permanent in August.
Mayo published an analysis of the first 35,000 patients as a preprint in August. It concluded, "The relationships between mortality and both time to plasma transfusion, and antibody levels provide a signature that is consistent with efficacy for the use of convalescent plasma in the treatment of hospitalized COVID-19 patients."
It seemed to work best when given early in infection and in larger doses; a similar pattern has been seen in studies of monoclonal antibodies. A revised version will soon be published in a major medical journal. Some criticized the findings as not being from a randomized clinical trial.
Convalescent plasma is not the only intervention that seems to work better when used earlier in the course of disease. Recently the pharmaceutical company Eli Lilly stopped a clinical trial of a monoclonal antibody in hospitalized COVID-19 patients when it became apparent it wasn't helping. It is continuing trials for patients who are less sick and begin treatment earlier, as well as in persons who have been exposed to the virus but not yet diagnosed as infected, to see if it might prevent infection. In November the FDA eased access to this drug outside of clinical trials, though it is not yet approved for sale.
Show Me the Money
The antibodies that seem to give plasma its curative powers are fragile proteins that the body produces to fight the virus. Production shuts down once the virus is cleared and the remaining antibodies survive only for a few weeks before the levels fade. [Vaccines are used to train immune cells to produce antibodies and other defenses to respond to exposure to future pathogens.] So they can be usefully harvested from a recovered patient for only a few short weeks or months before they decline precipitously. The question becomes, how does one mobilize this resource in that short window of opportunity?
The program run by the Mayo Clinic explains the process and criteria for donating convalescent plasma for COVID-19, as well as links to local blood centers equipped to handle those free donations. Commercial plasma centers also are advertising and paying for donations.
A majority of countries prohibit paying donors for blood or blood products, including India. But an investigation by India Today touted a black market of people willing to donate convalescent plasma for the equivalent of several hundred dollars. Officials vowed to prosecute, saying donations should be selfless.
But that enforcement threat seemed to be undercut when the health minister of the state of Assam declared "plasma donors will get preference in several government schemes including the government job interview." It appeared to be a form of compensation that far surpassed simple cash.
The small city of Rexburg, Idaho, with a population a bit over 50,000, overwhelmingly Mormon and home to a campus of Brigham Young University, at one point had one of the highest per capita rates of COVID-19 in the current wave of infection. Rumors circulated that some students were intentionally trying to become infected so they could later sell their plasma for top dollar, potentially as much as $200 a visit.
Troubled university officials investigated the allegations but could come up with nothing definitive; how does one prove intentionality with such an omnipresent yet elusive virus? They chalked it up to idle chatter, perhaps an urban legend, which might be associated with alcohol use on some other campus.
Doctors, hospitals, and drug companies are all rightly praised for their altruism in the fight against COVID-19, but they also get paid. Payment for whole blood donation in the U.S. is prohibited, and while payment for plasma is allowed, there is a stigma attached to payment and much plasma is donated for free. "Why do we expect the donors [of convalescent plasma] to be the only uncompensated people in the process? It really makes no sense," argues Mark Yarborough, an ethicist at the UC Davis School of Medicine in Sacramento.
"When I was in grad school, two of my closest friends, at least once a week they went and gave plasma. That was their weekend spending money," Yarborough recalls. He says upper and middle-income people may have the luxury of donating blood products but prohibiting people from selling their plasma is a bit paternalistic and doesn't do anything to improve the economic status of poor people.
"Asking people to dedicate two hours a week for an entire year in exchange for cookies and milk is demonstrably asking too much," says Peter Jaworski, an ethicist who teaches at Georgetown University.
He notes that companies that pay plasma donors have much lower total costs than do operations that rely solely on uncompensated donations. The companies have to spend less to recruit and retain donors because they increase payments to encourage regular repeat donations. They are able to more rationally schedule visits to maximize use of expensive apheresis equipment and medical personnel used for the collection.
It seems that COVID-19 has been with us forever, but in reality it is less than a year. We have learned much over that short time, can now better manage the disease, and have lower mortality rates to prove it. Just how much convalescent plasma may have contributed to that remains an open question. Access to vaccines is months away for many people, and even then some people will continue to get sick. Given the lack of proven treatments, it makes sense to keep plasma as part of the mix, and not close the door to any legitimate means to obtain it.
Is there a robot nanny in your child's future?
Some researchers argue that active, playful engagement with a "robot nanny" for a few hours a day is better than several hours in front of a TV or with an iPad.
From ROBOTS AND THE PEOPLE WHO LOVE THEM: Holding on to Our Humanity in an Age of Social Robots by Eve Herold. Copyright © 2024 by the author and reprinted by permission of St. Martin’s Publishing Group.
Could the use of robots take some of the workload off teachers, add engagement among students, and ultimately invigorate learning by taking it to a new level that is more consonant with the everyday experiences of young people? Do robots have the potential to become full-fledged educators and further push human teachers out of the profession? The preponderance of opinion on this subject is that, just as AI and medical technology are not going to eliminate doctors, robot teachers will never replace human teachers. Rather, they will change the job of teaching.
A 2017 study led by Google executive James Manyika suggested that skills like creativity, emotional intelligence, and communication will always be needed in the classroom and that robots aren’t likely to provide them at the same level that humans naturally do. But robot teachers do bring advantages, such as a depth of subject knowledge that teachers can’t match, and they’re great for student engagement.
The teacher and robot can complement each other in new ways, with the teacher facilitating interactions between robots and students. So far, this is the case with teaching “assistants” being adopted now in China, Japan, the U.S., and Europe. In this scenario, the robot (usually the SoftBank child-size robot NAO) is a tool for teaching mainly science, technology, engineering, and math (the STEM subjects), but the teacher is very involved in planning, overseeing, and evaluating progress. The students get an entertaining and enriched learning experience, and some of the teaching load is taken off the teacher. At least, that’s what researchers have been able to observe so far.
To be sure, there are some powerful arguments for having robots in the classroom. A not-to-be-underestimated one is that robots “speak the language” of today’s children, who have been steeped in technology since birth. These children are adept at navigating a media-rich environment that is highly visual and interactive. They are plugged into the Internet 24-7. They consume music, games, and huge numbers of videos on a weekly basis. They expect to be dazzled because they are used to being dazzled by more and more spectacular displays of digital artistry. Education has to compete with social media and the entertainment vehicles of students’ everyday lives.
Another compelling argument for teaching robots is that they help prepare students for the technological realities they will encounter in the real world when robots will be ubiquitous. From childhood on, they will be interacting and collaborating with robots in every sphere of their lives from the jobs they do to dealing with retail robots and helper robots in the home. Including robots in the classroom is one way of making sure that children of all socioeconomic backgrounds will be better prepared for a highly automated age, when successfully using robots will be as essential as reading and writing. We’ve already crossed this threshold with computers and smartphones.
Students need multimedia entertainment with their teaching. This is something robots can provide through their ability to connect to the Internet and act as a centralized host to videos, music, and games. Children also need interaction, something robots can deliver up to a point, but which humans can surpass. The education of a child is not just intended to make them technologically functional in a wired world, it’s to help them grow in intellectual, creative, social, and emotional ways. When considered through this perspective, it opens the door to questions concerning just how far robots should go. Robots don’t just teach and engage children; they’re designed to tug at their heartstrings.
It’s no coincidence that many toy makers and manufacturers are designing cute robots that look and behave like real children or animals, says Turkle. “When they make eye contact and gesture toward us, they predispose us to view them as thinking and caring,” she has written in The Washington Post. “They are designed to be cute, to provide a nurturing response” from the child. As mentioned previously, this nurturing experience is a powerful vehicle for drawing children in and promoting strong attachment. But should children really love their robots?
ROBOTS AND THE PEOPLE WHO LOVE THEM: Holding on to Our Humanity in an Age of Social Robots by Eve Herold (January 9, 2024).
St. Martin’s Publishing Group
The problem, once again, is that a child can be lulled into thinking that she’s in an actual relationship, when a robot can’t possibly love her back. If adults have these vulnerabilities, what might such asymmetrical relationships do to the emotional development of a small child? Turkle notes that while we tend to ascribe a mind and emotions to a socially interactive robot, “simulated thinking may be thinking, but simulated feeling is never feeling, and simulated love is never love.”
Always a consideration is the fact that in the first few years of life, a child’s brain is undergoing rapid growth and development that will form the foundation of their lifelong emotional health. These formative experiences are literally shaping the child’s brain, their expectations, and their view of the world and their place in it. In Alone Together, Turkle asks: What are we saying to children about their importance to us when we’re willing to outsource their care to a robot? A child might be superficially entertained by the robot while his self-esteem is systematically undermined.
Research has emerged showing that there are clear downsides to child-robot relationships.
Still, in the case of robot nannies in the home, is active, playful engagement with a robot for a few hours a day any more harmful than several hours in front of a TV or with an iPad? Some, like Xiong, regard interacting with a robot as better than mere passive entertainment. iPal’s manufacturers say that their robot can’t replace parents or teachers and is best used by three- to eight-year-olds after school, while they wait for their parents to get off work. But as robots become ever-more sophisticated, they’re expected to perform more of the tasks of day-to-day care and to be much more emotionally advanced. There is no question children will form deep attachments to some of them. And research has emerged showing that there are clear downsides to child-robot relationships.
Some studies, performed by Turkle and fellow MIT colleague Cynthia Breazeal, have revealed a darker side to the child-robot bond. Turkle has reported extensively on these studies in The Washington Post and in her book Alone Together. Most children love robots, but some act out their inner bully on the hapless machines, hitting and kicking them and otherwise trying to hurt them. The trouble is that the robot can’t fight back, teaching children that they can bully and abuse without consequences. As in any other robot relationship, such harmful behavior could carry over into the child’s human relationships.
And, ironically, it turns out that communicative machines don’t actually teach kids good communication skills. It’s well known that parent-child communication in the first three years of life sets the stage for a very young child’s intellectual and academic success. Verbal back-and-forth with parents and care-givers is like fuel for a child’s growing brain. One article that examined several types of play and their effect on children’s communication skills, published in JAMA Pediatrics in 2015, showed that babies who played with electronic toys—like the popular robot dog Aibo—show a decrease in both the quantity and quality of their language skills.
Anna V. Sosa of the Child Speech and Language Lab at Northern Arizona University studied twenty-six ten- to sixteen- month-old infants to compare the growth of their language skills after they played with three types of toys: electronic toys like a baby laptop and talking farm; traditional toys like wooden puzzles and building blocks; and books read aloud by their parents. The play that produced the most growth in verbal ability was having books read to them by a caregiver, followed by play with traditional toys. Language gains after playing with electronic toys came dead last. This form of play involved the least use of adult words, the least conversational turntaking, and the least verbalizations from the children. While the study sample was small, it’s not hard to extrapolate that no electronic toy or even more abled robot could supply the intimate responsiveness of a parent reading stories to a child, explaining new words, answering the child’s questions, and modeling the kind of back- and-forth interaction that promotes empathy and reciprocity in relationships.
***
Most experts acknowledge that robots can be valuable educational tools. But they can’t make a child feel truly loved, validated, and valued. That’s the job of parents, and when parents abdicate this responsibility, it’s not only the child who misses out on one of life’s most profound experiences.
We really don’t know how the tech-savvy children of today will ultimately process their attachments to robots and whether they will be excessively predisposed to choosing robot companionship over that of humans. It’s possible their techno literacy will draw for them a bold line between real life and a quasi-imaginary history with a robot. But it will be decades before we see long-term studies culminating in sufficient data to help scientists, and the rest of us, to parse out the effects of a lifetime spent with robots.
This is an excerpt from ROBOTS AND THE PEOPLE WHO LOVE THEM: Holding on to Our Humanity in an Age of Social Robots by Eve Herold. The book will be published on January 9, 2024.
Stem cells from a fetus can travel to the heart and regenerate the muscle, essentially saving a mother’s life.
Story by Big Think
In rare cases, a woman’s heart can start to fail in the months before or after giving birth. The all-important muscle weakens as its chambers enlarge, reducing the amount of blood pumped with each beat. Peripartum cardiomyopathy can threaten the lives of both mother and child. Viral illness, nutritional deficiency, the bodily stress of pregnancy, or an abnormal immune response could all play a role, but the causes aren’t concretely known.
If there is a silver lining to peripartum cardiomyopathy, it’s that it is perhaps the most survivable form of heart failure. A remarkable 50% of women recover spontaneously. And there’s an even more remarkable explanation for that glowing statistic: The fetus‘ stem cells migrate to the heart and regenerate the beleaguered muscle. In essence, the developing or recently born child saves its mother’s life.
Saving mama
While this process has not been observed directly in humans, it has been witnessed in mice. In a 2015 study, researchers tracked stem cells from fetal mice as they traveled to mothers’ damaged cardiac cells and integrated themselves into hearts.
Evolutionarily, this function makes sense: It is in the fetus’ best interest that its mother remains healthy.
Scientists also have spotted cells from the fetus within the hearts of human mothers, as well as countless other places inside the body, including the skin, spleen, liver, brain, lung, kidney, thyroid, lymph nodes, salivary glands, gallbladder, and intestine. These cells essentially get everywhere. While most are eliminated by the immune system during pregnancy, some can persist for an incredibly long time — up to three decades after childbirth.
This integration of the fetus’ cells into the mother’s body has been given a name: fetal microchimerism. The process appears to start between the fourth and sixth week of gestation in humans. Scientists are actively trying to suss out its purpose. Fetal stem cells, which can differentiate into all sorts of specialized cells, appear to target areas of injury. So their role in healing seems apparent. Evolutionarily, this function makes sense: It is in the fetus’ best interest that its mother remains healthy.
Sending cells into the mother’s body may also prime her immune system to grow more tolerant of the developing fetus. Successful pregnancy requires that the immune system not see the fetus as an interloper and thus dispatch cells to attack it.
Fetal microchimerism
But fetal microchimerism might not be entirely beneficial. Greater concentrations of the cells have been associated with various autoimmune diseases such as lupus, Sjogren’s syndrome, and even multiple sclerosis. After all, they are foreign cells living in the mother’s body, so it’s possible that they might trigger subtle, yet constant inflammation. Fetal cells also have been linked to cancer, although it isn’t clear whether they abet or hinder the disease.
A team of Spanish scientists summarized the apparent give and take of fetal microchimerism in a 2022 review article. “On the one hand, fetal microchimerism could be a source of progenitor cells with a beneficial effect on the mother’s health by intervening in tissue repair, angiogenesis, or neurogenesis. On the other hand, fetal microchimerism might have a detrimental function by activating the immune response and contributing to autoimmune diseases,” they wrote.
Regardless of a fetus’ cells net effect, their existence alone is intriguing. In a paper published earlier this year, University of London biologist Francisco Úbeda and University of Western Ontario mathematical biologist Geoff Wild noted that these cells might very well persist within mothers for life.
“Therefore, throughout their reproductive lives, mothers accumulate fetal cells from each of their past pregnancies including those resulting in miscarriages. Furthermore, mothers inherit, from their own mothers, a pool of cells contributed by all fetuses carried by their mothers, often referred to as grandmaternal microchimerism.”
So every mother may carry within her literal pieces of her ancestors.