Blood Money: Paying for Convalescent Plasma to Treat COVID-19
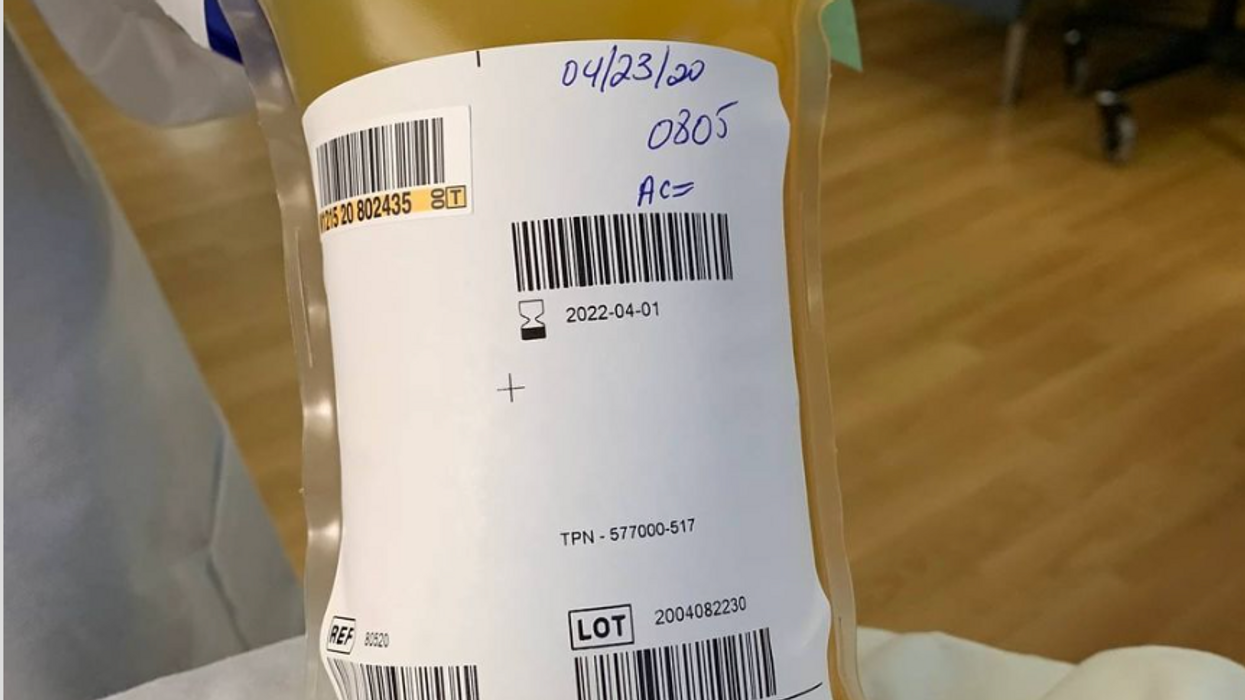
A bag of plasma that Tom Hanks donated back in April 2020 after his coronavirus infection. (He was not paid to donate.)
Convalescent plasma – first used to treat diphtheria in 1890 – has been dusted off the shelf to treat COVID-19. Does it work? Should we rely strictly on the altruism of donors or should people be paid for it?
The biologic theory is that a person who has recovered from a disease has chemicals in their blood, most likely antibodies, that contributed to their recovery, and transferring those to a person who is sick might aid their recovery. Whole blood won't work because there are too few antibodies in a single unit of blood and the body can hold only so much of it.
Plasma comprises about 55 percent of whole blood and is what's left once you take out the red blood cells that carry oxygen and the white blood cells of the immune system. Most of it is water but the rest is a complex mix of fats, salts, signaling molecules and proteins produced by the immune system, including antibodies.
A process called apheresis circulates the donors' blood through a machine that separates out the desired parts of blood and returns the rest to the donor. It takes several times the length of a regular whole blood donation to cycle through enough blood for the process. The end product is a yellowish concentration called convalescent plasma.
Recent History
It was used extensively during the great influenza epidemic off 1918 but fell out of favor with the development of antibiotics. Still, whenever a new disease emerges – SARS, MERS, Ebola, even antibiotic-resistant bacteria – doctors turn to convalescent plasma, often as a stopgap until more effective antibiotic and antiviral drugs are developed. The process is certainly safe when standard procedures for handling blood products are followed, and historically it does seem to be beneficial in at least some patients if administered early enough in the disease.
With few good treatment options for COVID-19, doctors have given convalescent plasma to more than a hundred thousand Americans and tens of thousand of people elsewhere, to mixed results. Placebo-controlled trials could give a clearer picture of plasma's value but it is difficult to enroll patients facing possible death when the flip of a coin will determine who will receive a saline solution or plasma.
And the plasma itself isn't some uniform pill stamped out in a factory, it's a natural product that is shaped by the immune history of the donor's body and its encounter not just with SARS-CoV-2 but a lifetime of exposure to different pathogens.
Researchers believe antibodies in plasma are a key factor in directly fighting the virus. But the variety and quantity of antibodies vary from donor to donor, and even over time from the same donor because once the immune system has cleared the virus from the body, it stops putting out antibodies to fight the virus. Often the quality and quantity of antibodies being given to a patient are not measured, making it somewhat hit or miss, which is why several companies have recently developed monoclonal antibodies, a single type of antibody found in blood that is effective against SARS-CoV-2 and that is multiplied in the lab for use as therapy.
Plasma may also contain other unknown factors that contribute to fighting disease, say perhaps signaling molecules that affect gene expression, which might affect the movement of immune cells, their production of antiviral molecules, or the regulation of inflammation. The complexity and lack of standardization makes it difficult to evaluate what might be working or not with a convalescent plasma treatment. Thus researchers are left with few clues about how to make it more effective.
Industrializing Plasma
Many Americans living along the border with Mexico regularly head south to purchase prescription drugs at a significant discount. Less known is the medical traffic the other way, Mexicans who regularly head north to be paid for plasma donations, which are prohibited in their country; the U.S. allows payment for plasma donations but not whole blood. A typical payment is about $35 for a donation but the sudden demand for convalescent plasma from people who have recovered from COVID-19 commands a premium price, sometimes as high as $200. These donors are part of a fast-growing plasma industry that surpassed $25 billion in 2018. The U.S. supplies about three-quarters of the world's needs for plasma.
Payment for whole blood donation in the U.S. is prohibited, and while payment for plasma is allowed, there is a stigma attached to payment and much plasma is donated for free.
The pharmaceutical industry has shied away from natural products they cannot patent but they have identified simpler components from plasma, such as clotting factors and immunoglobulins, that have been turned into useful drugs from this raw material of plasma. While some companies have retooled to provide convalescent plasma to treat COVID-19, often paying those donors who have recovered a premium of several times the normal rate, most convalescent plasma has come as donations through traditional blood centers.
In April the Mayo Clinic, in cooperation with the FDA, created an expanded access program for convalescent plasma to treat COVID-19. It was meant to reduce the paperwork associated with gaining access to a treatment not yet approved by the FDA for that disease. Initially it was supposed to be for 5000 units but it quickly grew to more than twenty times that size. Michael Joyner, the head of the program, discussed that experience in an extended interview in September.
The Centers for Medicare and Medicaid Services (CMS) also created associated reimbursement codes, which became permanent in August.
Mayo published an analysis of the first 35,000 patients as a preprint in August. It concluded, "The relationships between mortality and both time to plasma transfusion, and antibody levels provide a signature that is consistent with efficacy for the use of convalescent plasma in the treatment of hospitalized COVID-19 patients."
It seemed to work best when given early in infection and in larger doses; a similar pattern has been seen in studies of monoclonal antibodies. A revised version will soon be published in a major medical journal. Some criticized the findings as not being from a randomized clinical trial.
Convalescent plasma is not the only intervention that seems to work better when used earlier in the course of disease. Recently the pharmaceutical company Eli Lilly stopped a clinical trial of a monoclonal antibody in hospitalized COVID-19 patients when it became apparent it wasn't helping. It is continuing trials for patients who are less sick and begin treatment earlier, as well as in persons who have been exposed to the virus but not yet diagnosed as infected, to see if it might prevent infection. In November the FDA eased access to this drug outside of clinical trials, though it is not yet approved for sale.
Show Me the Money
The antibodies that seem to give plasma its curative powers are fragile proteins that the body produces to fight the virus. Production shuts down once the virus is cleared and the remaining antibodies survive only for a few weeks before the levels fade. [Vaccines are used to train immune cells to produce antibodies and other defenses to respond to exposure to future pathogens.] So they can be usefully harvested from a recovered patient for only a few short weeks or months before they decline precipitously. The question becomes, how does one mobilize this resource in that short window of opportunity?
The program run by the Mayo Clinic explains the process and criteria for donating convalescent plasma for COVID-19, as well as links to local blood centers equipped to handle those free donations. Commercial plasma centers also are advertising and paying for donations.
A majority of countries prohibit paying donors for blood or blood products, including India. But an investigation by India Today touted a black market of people willing to donate convalescent plasma for the equivalent of several hundred dollars. Officials vowed to prosecute, saying donations should be selfless.
But that enforcement threat seemed to be undercut when the health minister of the state of Assam declared "plasma donors will get preference in several government schemes including the government job interview." It appeared to be a form of compensation that far surpassed simple cash.
The small city of Rexburg, Idaho, with a population a bit over 50,000, overwhelmingly Mormon and home to a campus of Brigham Young University, at one point had one of the highest per capita rates of COVID-19 in the current wave of infection. Rumors circulated that some students were intentionally trying to become infected so they could later sell their plasma for top dollar, potentially as much as $200 a visit.
Troubled university officials investigated the allegations but could come up with nothing definitive; how does one prove intentionality with such an omnipresent yet elusive virus? They chalked it up to idle chatter, perhaps an urban legend, which might be associated with alcohol use on some other campus.
Doctors, hospitals, and drug companies are all rightly praised for their altruism in the fight against COVID-19, but they also get paid. Payment for whole blood donation in the U.S. is prohibited, and while payment for plasma is allowed, there is a stigma attached to payment and much plasma is donated for free. "Why do we expect the donors [of convalescent plasma] to be the only uncompensated people in the process? It really makes no sense," argues Mark Yarborough, an ethicist at the UC Davis School of Medicine in Sacramento.
"When I was in grad school, two of my closest friends, at least once a week they went and gave plasma. That was their weekend spending money," Yarborough recalls. He says upper and middle-income people may have the luxury of donating blood products but prohibiting people from selling their plasma is a bit paternalistic and doesn't do anything to improve the economic status of poor people.
"Asking people to dedicate two hours a week for an entire year in exchange for cookies and milk is demonstrably asking too much," says Peter Jaworski, an ethicist who teaches at Georgetown University.
He notes that companies that pay plasma donors have much lower total costs than do operations that rely solely on uncompensated donations. The companies have to spend less to recruit and retain donors because they increase payments to encourage regular repeat donations. They are able to more rationally schedule visits to maximize use of expensive apheresis equipment and medical personnel used for the collection.
It seems that COVID-19 has been with us forever, but in reality it is less than a year. We have learned much over that short time, can now better manage the disease, and have lower mortality rates to prove it. Just how much convalescent plasma may have contributed to that remains an open question. Access to vaccines is months away for many people, and even then some people will continue to get sick. Given the lack of proven treatments, it makes sense to keep plasma as part of the mix, and not close the door to any legitimate means to obtain it.
Will religious people reject organ transplants from pigs?
Scientists are getting better at transplanting pig organs into humans. But religious followers of prohibitions on consuming pork may reject these organs, even if their bodies could accept them.
The first successful recipient of a human heart transplant lived 18 days. The first artificial heart recipient lived just over 100.
Their brief post-transplant lives paved the way toward vastly greater successes. Former Vice President Dick Cheney relied on an artificial heart for nearly two years before receiving a human heart transplant. It still beats in his chest more than a decade later.
Organ transplantation recently reached its next phase with David Bennett. He survived for two months after becoming the first recipient of a pig’s heart genetically modified to function in a human body in February. Known as a xenotransplant, the procedure could pave the way for greatly expanding the use of transplanted vital organs to extend human lives.
Clinical trials would have to be held in the U.S. before xenotransplants become widespread; Bennett’s surgery was authorized under a special Food and Drug Administration program that addresses patients with life-threatening medical conditions.
German researchers plan to perform eight pig-to-human heart transplants as part of a clinical trial beginning in 2024. According to an email sent to Leaps.org by three scholars working on the German project, these procedures will focus on one of the reasons David Bennett did not survive longer: A porcine infection from his new heart.
The transplant team will conduct more sensitive testing of the donor organs, “which in all likelihood will be able to detect even low levels of virus in the xenograft,” note the scientists, Katharina Ebner, Jochen Ostheimer and Jochen Sautermeister. They are confident that the risk of infection with a porcine virus in the future will be significantly lower.
Moreover, hearts are not the only genetically modified organs that are being xenotransplanted. A team of surgeons at the University of Alabama at Birmingham successfully transplanted genetically modified pig kidneys into a brain-dead human recipient in September. The kidneys functioned normally for more than three days before the experiment ended. The UAB team is now moving forward with clinical trials focusing on transplanting pig kidneys into human patients.
Some experts believe the momentum for xenotransplantation is building, particularly given the recent successes. “I think there is a strong likelihood this will go mainstream,” says Brendan Parent of NYU Langone Health.
Douglas Anderson, a surgeon who is part of that kidney xenotransplant team, observes that, “organ shortages have been the major issue facing transplantation since its inception” and that xenotransplantation is a potential solution to that quandary. “It can’t be understated the number of people waiting for a kidney on dialysis, which has a significant mortality rate,” he says. According to the advocacy group Donate Life America, more than 100,000 people in the U.S. alone are waiting for a donated organ, and 85 percent of them need a kidney.
Other experts believe the momentum for xenotransplantation is building, particularly given the recent successes. “I think there is a strong likelihood this will go mainstream,” says Brendan Parent, director of transplant ethics and policy at NYU Langone Health, a New York City-based hospital system. Like the UAB team, surgeons at NYU Langone have had success coaxing modified pig kidneys to work in deceased humans.
“There is a genuinely good chance that within a generation, (xenotransplantation) might become very common in reasonably wealthy countries,” says Michael Reiss, professor of science education at University College in London. In addition to his academic position, Reiss sits on the Nuffield Council on Bioethics, a nonprofit that is one of Britain’s most prominent watchdogs regarding medical and scientific issues. Reiss is also an Anglican priest and has studied xenotransplantation from both a scientific and religious point of view.
Moreover, genetic modifications could one day lead to organs being specifically optimized for their recipients. That could ensure issues like donor rejection and the calculated risk of artificially suppressing recipient immune systems become concerns of the past.
Major bioethical, religious concerns
Despite the promise of xenotransplantation, numerous bioethical issues swirl around the procedure. They could be magnified if xenotransplantation evolves from one-off experiments to a routine medical procedure.
One of the biggest is the millennia-long prohibitions Islam and Judaism have had regarding the consumption of pork. Will followers of these religions assume such rules extend to those taboo materials being inserted into a human body?
“Initially, one’s instinctual reaction is that, oh, crumbs! – how are Jews and Muslims going to react to that?” Reiss says. But in a world where science and secularism are accepted on an everyday basis, he notes it is not a significant issue. Reiss points out that valves from pig hearts have been used in human patients for decades without any issues. He adds that both Islam and Judaism waive religious dietary restrictions if a human life is at risk.
“While nobody's saying an individual patient is to be forced to have these, the very high proportion of people who identify as Jews or Muslims when given this option are content with it,” he says.
Concurring with Reiss is Michael Gusamano, professor of health policy at Lehigh University and director of its Center for Ethics. He is currently performing research on the ethics of xenotransplantation for the National Institutes of Health.
“Leaders from all major religions have commented on this and have indicated that this is not inconsistent with religious doctrine,” Gusamano says in written remarks to Leaps.org. “Having said that, it is plausible to believe that some people will assume that this is inconsistent with the teaching of their religion and may object to…receiving a xenotransplant as part of routine medical care.”
A history of clashes
Despite those assurances, science has long clashed with theology. Although Galileo proved the planets revolved around the sun, the Catholic Church found him guilty of heresy and rewarded his discovery with house arrest for the last decade of his life. A revolt occurred in mid-19th century India after native-born soldiers believed the ammunition supplied by their British occupiers had been lubricated with pork and beef tallow. Given they had to use their mouths to tear open ammunition pouches, this violated both the tenets of Islam and Hinduism. And one of the conspiracy theories hatched as a result of COVID-19 was that the vaccines developed to fight the disease were the “mark of the beast” – a sign of impending Armageddon under evangelical Christian theology.
The German xenotransplant research team has encountered such potential concerns when the procedure is regarded through a religious lens. “The pastors in our research suspected that many recipients might feel disgust and revulsion,” they write. “Even beyond these special religious reservations, cultural scripts about pigs as inferior living beings are also generally widespread and effective in the western world, so that here too possible disgust reactions cannot be ruled out.”
The German researchers add that “Jewish and Muslim hospital pastoral workers believe possible considerable problems in this respect, which must be dealt with psychosocially, religiously, and pastorally prior to a possible transplantation in order to strengthen the acceptance of the received organ by the patients and their relatives.”
Parent, the director at NYU Langone, shares a concern that xenotransplantation could move “too fast,” although much of his worry is focused on zoonotic disease transmission – pig viruses jumping into humans as a result of such procedures.
Another ethical issue
Moreover, the way pigs and other animals are raised for transplants could pose future ethical dilemmas.
Reiss notes that pigs raised for medical procedures have to be grown and kept in what are known as a designated pathogen-free facility, or DPF. Such facilities are kept painstakingly antiseptic so as to minimize the risk of zoonotic transmissions. But given pigs are fond of outdoor activities such as wallowing in mud and sleeping on hay, they lead “stunningly boring lives” that they probably do not enjoy, Reiss observes.
Ethical concerns with using pigs may push transplantation medicine into its next logical phase: Growing functional organs for transplant in a laboratory setting.
“There’s no doubt that these research pigs have gotten much better veterinary care, et cetera, (compared to farmed pigs). But it’s not a great life,” Reiss says. “And although it hasn’t so far dominated the discussion, I think as the years go by, rather as we’ve seen with the use of apes and now monkeys in medical research, more and more theologians will get uncomfortable about us just assuming we can do this with…pigs.”
The German research team raises the same concerns, but has taken a fairly sanguine view on the topic. “The impairments of the species-typical behavior will certainly provoke criticism and perhaps also public protest. But the number of animals affected is very small in relation to slaughter cattle,” the German researchers note. “Moreover, the conditions there and also in several animal experiments are far worse.”
Observers say that may push transplantation medicine into its next logical phase: Growing functional organs for transplant in a laboratory setting. Anderson, the UAB transplant surgeon, believes such an accomplishment remains decades away.
But other experts believe there is a moral imperative that xenotransplantation remain a temporary solution. “I think we have a duty to go in that direction,” Parent says. “We have to go that way, with the xenotransplantation process (as) a steppingstone and research path that will be useful for bioengineered organs.”
The Friday Five: Scientists treated this girl's disease before she was born
In this week's Friday Five, scientists treated this girl's rare diseases in utero. Plus, how to lift weights in half the time, electric shocks help people regain the ability to walk, meditation is found to work as well as medication, and much more.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Here are the promising studies covered in this week's Friday Five:
- Kids treated for diseases before they're born
- How to lift weights in half the time
- Electric shocks help people regain the ability to walk
- Meditation just as good as medication?
- These foods could pump up your motivation

