Blood Money: Paying for Convalescent Plasma to Treat COVID-19
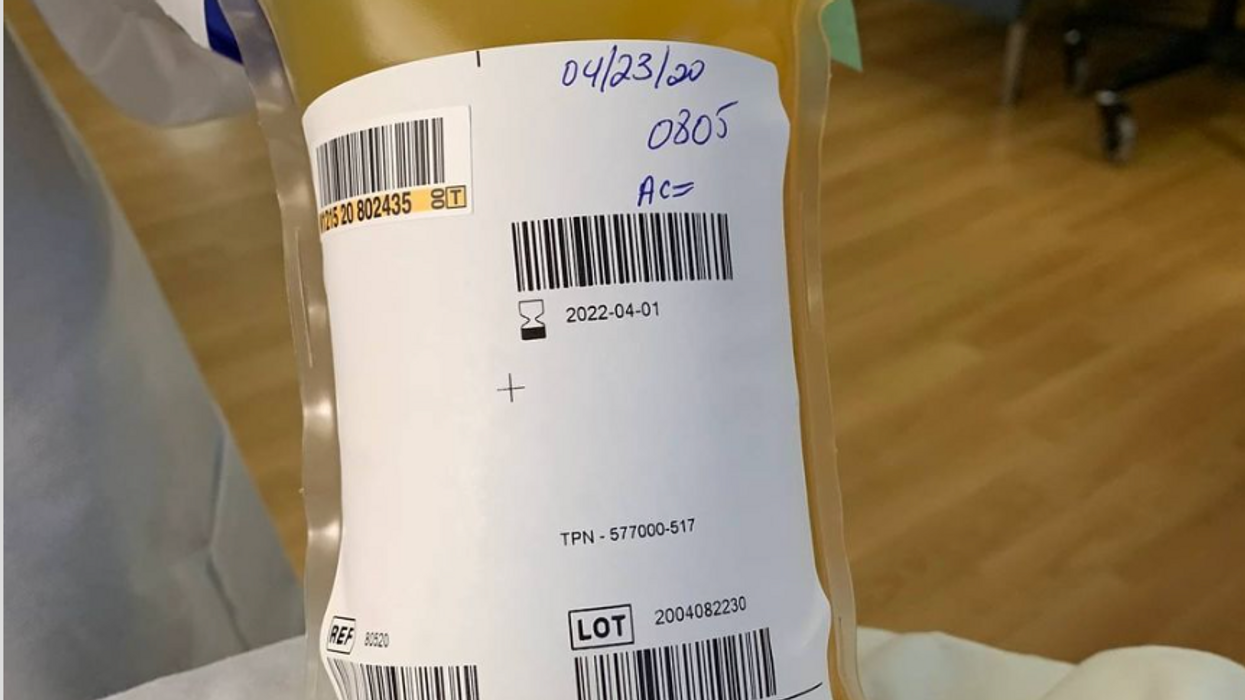
A bag of plasma that Tom Hanks donated back in April 2020 after his coronavirus infection. (He was not paid to donate.)
Convalescent plasma – first used to treat diphtheria in 1890 – has been dusted off the shelf to treat COVID-19. Does it work? Should we rely strictly on the altruism of donors or should people be paid for it?
The biologic theory is that a person who has recovered from a disease has chemicals in their blood, most likely antibodies, that contributed to their recovery, and transferring those to a person who is sick might aid their recovery. Whole blood won't work because there are too few antibodies in a single unit of blood and the body can hold only so much of it.
Plasma comprises about 55 percent of whole blood and is what's left once you take out the red blood cells that carry oxygen and the white blood cells of the immune system. Most of it is water but the rest is a complex mix of fats, salts, signaling molecules and proteins produced by the immune system, including antibodies.
A process called apheresis circulates the donors' blood through a machine that separates out the desired parts of blood and returns the rest to the donor. It takes several times the length of a regular whole blood donation to cycle through enough blood for the process. The end product is a yellowish concentration called convalescent plasma.
Recent History
It was used extensively during the great influenza epidemic off 1918 but fell out of favor with the development of antibiotics. Still, whenever a new disease emerges – SARS, MERS, Ebola, even antibiotic-resistant bacteria – doctors turn to convalescent plasma, often as a stopgap until more effective antibiotic and antiviral drugs are developed. The process is certainly safe when standard procedures for handling blood products are followed, and historically it does seem to be beneficial in at least some patients if administered early enough in the disease.
With few good treatment options for COVID-19, doctors have given convalescent plasma to more than a hundred thousand Americans and tens of thousand of people elsewhere, to mixed results. Placebo-controlled trials could give a clearer picture of plasma's value but it is difficult to enroll patients facing possible death when the flip of a coin will determine who will receive a saline solution or plasma.
And the plasma itself isn't some uniform pill stamped out in a factory, it's a natural product that is shaped by the immune history of the donor's body and its encounter not just with SARS-CoV-2 but a lifetime of exposure to different pathogens.
Researchers believe antibodies in plasma are a key factor in directly fighting the virus. But the variety and quantity of antibodies vary from donor to donor, and even over time from the same donor because once the immune system has cleared the virus from the body, it stops putting out antibodies to fight the virus. Often the quality and quantity of antibodies being given to a patient are not measured, making it somewhat hit or miss, which is why several companies have recently developed monoclonal antibodies, a single type of antibody found in blood that is effective against SARS-CoV-2 and that is multiplied in the lab for use as therapy.
Plasma may also contain other unknown factors that contribute to fighting disease, say perhaps signaling molecules that affect gene expression, which might affect the movement of immune cells, their production of antiviral molecules, or the regulation of inflammation. The complexity and lack of standardization makes it difficult to evaluate what might be working or not with a convalescent plasma treatment. Thus researchers are left with few clues about how to make it more effective.
Industrializing Plasma
Many Americans living along the border with Mexico regularly head south to purchase prescription drugs at a significant discount. Less known is the medical traffic the other way, Mexicans who regularly head north to be paid for plasma donations, which are prohibited in their country; the U.S. allows payment for plasma donations but not whole blood. A typical payment is about $35 for a donation but the sudden demand for convalescent plasma from people who have recovered from COVID-19 commands a premium price, sometimes as high as $200. These donors are part of a fast-growing plasma industry that surpassed $25 billion in 2018. The U.S. supplies about three-quarters of the world's needs for plasma.
Payment for whole blood donation in the U.S. is prohibited, and while payment for plasma is allowed, there is a stigma attached to payment and much plasma is donated for free.
The pharmaceutical industry has shied away from natural products they cannot patent but they have identified simpler components from plasma, such as clotting factors and immunoglobulins, that have been turned into useful drugs from this raw material of plasma. While some companies have retooled to provide convalescent plasma to treat COVID-19, often paying those donors who have recovered a premium of several times the normal rate, most convalescent plasma has come as donations through traditional blood centers.
In April the Mayo Clinic, in cooperation with the FDA, created an expanded access program for convalescent plasma to treat COVID-19. It was meant to reduce the paperwork associated with gaining access to a treatment not yet approved by the FDA for that disease. Initially it was supposed to be for 5000 units but it quickly grew to more than twenty times that size. Michael Joyner, the head of the program, discussed that experience in an extended interview in September.
The Centers for Medicare and Medicaid Services (CMS) also created associated reimbursement codes, which became permanent in August.
Mayo published an analysis of the first 35,000 patients as a preprint in August. It concluded, "The relationships between mortality and both time to plasma transfusion, and antibody levels provide a signature that is consistent with efficacy for the use of convalescent plasma in the treatment of hospitalized COVID-19 patients."
It seemed to work best when given early in infection and in larger doses; a similar pattern has been seen in studies of monoclonal antibodies. A revised version will soon be published in a major medical journal. Some criticized the findings as not being from a randomized clinical trial.
Convalescent plasma is not the only intervention that seems to work better when used earlier in the course of disease. Recently the pharmaceutical company Eli Lilly stopped a clinical trial of a monoclonal antibody in hospitalized COVID-19 patients when it became apparent it wasn't helping. It is continuing trials for patients who are less sick and begin treatment earlier, as well as in persons who have been exposed to the virus but not yet diagnosed as infected, to see if it might prevent infection. In November the FDA eased access to this drug outside of clinical trials, though it is not yet approved for sale.
Show Me the Money
The antibodies that seem to give plasma its curative powers are fragile proteins that the body produces to fight the virus. Production shuts down once the virus is cleared and the remaining antibodies survive only for a few weeks before the levels fade. [Vaccines are used to train immune cells to produce antibodies and other defenses to respond to exposure to future pathogens.] So they can be usefully harvested from a recovered patient for only a few short weeks or months before they decline precipitously. The question becomes, how does one mobilize this resource in that short window of opportunity?
The program run by the Mayo Clinic explains the process and criteria for donating convalescent plasma for COVID-19, as well as links to local blood centers equipped to handle those free donations. Commercial plasma centers also are advertising and paying for donations.
A majority of countries prohibit paying donors for blood or blood products, including India. But an investigation by India Today touted a black market of people willing to donate convalescent plasma for the equivalent of several hundred dollars. Officials vowed to prosecute, saying donations should be selfless.
But that enforcement threat seemed to be undercut when the health minister of the state of Assam declared "plasma donors will get preference in several government schemes including the government job interview." It appeared to be a form of compensation that far surpassed simple cash.
The small city of Rexburg, Idaho, with a population a bit over 50,000, overwhelmingly Mormon and home to a campus of Brigham Young University, at one point had one of the highest per capita rates of COVID-19 in the current wave of infection. Rumors circulated that some students were intentionally trying to become infected so they could later sell their plasma for top dollar, potentially as much as $200 a visit.
Troubled university officials investigated the allegations but could come up with nothing definitive; how does one prove intentionality with such an omnipresent yet elusive virus? They chalked it up to idle chatter, perhaps an urban legend, which might be associated with alcohol use on some other campus.
Doctors, hospitals, and drug companies are all rightly praised for their altruism in the fight against COVID-19, but they also get paid. Payment for whole blood donation in the U.S. is prohibited, and while payment for plasma is allowed, there is a stigma attached to payment and much plasma is donated for free. "Why do we expect the donors [of convalescent plasma] to be the only uncompensated people in the process? It really makes no sense," argues Mark Yarborough, an ethicist at the UC Davis School of Medicine in Sacramento.
"When I was in grad school, two of my closest friends, at least once a week they went and gave plasma. That was their weekend spending money," Yarborough recalls. He says upper and middle-income people may have the luxury of donating blood products but prohibiting people from selling their plasma is a bit paternalistic and doesn't do anything to improve the economic status of poor people.
"Asking people to dedicate two hours a week for an entire year in exchange for cookies and milk is demonstrably asking too much," says Peter Jaworski, an ethicist who teaches at Georgetown University.
He notes that companies that pay plasma donors have much lower total costs than do operations that rely solely on uncompensated donations. The companies have to spend less to recruit and retain donors because they increase payments to encourage regular repeat donations. They are able to more rationally schedule visits to maximize use of expensive apheresis equipment and medical personnel used for the collection.
It seems that COVID-19 has been with us forever, but in reality it is less than a year. We have learned much over that short time, can now better manage the disease, and have lower mortality rates to prove it. Just how much convalescent plasma may have contributed to that remains an open question. Access to vaccines is months away for many people, and even then some people will continue to get sick. Given the lack of proven treatments, it makes sense to keep plasma as part of the mix, and not close the door to any legitimate means to obtain it.
Friday Five: These boots were made for walking, even for people who can't
New boots could have you moving like Iron Man, based on research this month by Stanford scientists.
The Friday Five covers important stories in health and science research that you may have missed - usually over the previous week but, today, we're doing a lookback on breakthrough research over the month of October. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
This Friday Five episode covers the following studies published and announced over the past month:
- New boots could have you moving like Iron Man
- The problem with bedtime munching
- The perfect recipe for tiny brains
- The best sports for kids to avoid lifelong health risks
- Can virtual reality reduce pain?
Should egg and sperm donors reveal their identities? The debate pivots on genetics and medical history.
Cassandra Adams performs on stage at the Jersey City Theater Center in March 2019 to raise awareness about traumatic experiences that she and others have had with anonymous donor conception.
Until age 35, Cassandra Adams assumed her mother and father were her biological parents. Then she took saliva tests through two genealogy databases—23andMe and AncestryDNA—and discovered a discrepancy in her heritage. In bringing up the matter with her parents, she learned that fertility issues had led the couple to use a sperm donor.
“Most people my age were not told,” said Adams, now 40 and a stay-at-home mom in Jersey City, New Jersey, who is involved with donor-conception advocacy. “Even now, there’s still a lot of secrecy in the industry. There are still many parents who aren’t truthful or planning not to be truthful with their children.”
While some of those offspring may never know a significant part of their medical history, Adams is grateful that she does. Surprisingly, the DNA test revealed Jewish ancestry.
“There are a lot more genetic conditions that run in Jewish families, so it was really important that I get my medical history, because it’s very different from my dad who raised me,” said Adams, who has met her biological father and two of three known half-siblings. As a result of this experience, she converted to Judaism. “It has been a big journey,” she said.
In an era of advancing assisted reproduction technologies, genetics and medical history have become front and center of the debate as to whether or not egg and sperm donations should be anonymous – and whether secrecy is even possible in many cases.
Obstacles to staying anonymous
People looking to become parents can choose what’s called an “identity-release donor,” meaning their child can receive information about the donor when he or she turns 18. There’s no way to ensure that the donor will consent to a relationship at that time. Instead, if a relationship between the donor and child is a priority, parents may decide to use a known donor.
The majority of donors want to remain anonymous, said reproductive endocrinologist Robert Kiltz, founder and director of CNY Fertility in Syracuse, New York. “In general, egg and sperm donation is mostly anonymous, meaning the recipient doesn’t know the donor and the donor doesn’t know the recipient.”
Even if the donor isn’t disclosed, though, the mystery may become unraveled when a donor-conceived person undergoes direct-to-consumer genetic testing through ancestry databases, which are growing in number and popularity. These services offer DNA testing and links to relatives with identifiable information.
In the future, another obstacle to anonymity could be laws that prohibit anonymous sperm and egg donations, if they catch on. In June, Colorado became the first state in the nation to ban anonymous sperm and egg donations. The law, which takes effect in 2025, will give donor-conceived adults the legal authority to obtain their donor’s identity and medical history. It also requires banks that provide sperm and egg collection to keep current medical records and contact information for all donors. Meanwhile, it prohibits donations from those who won’t consent to identity disclosures.
“The tradition of anonymous sperm or egg donation has created a vast array of problems, most significantly that the people thus created want to know who their mommy and daddy are,” said Kenneth W. Goodman, professor and director of the Institute for Bioethics and Health Policy at the University of Miami Miller School of Medicine.
“There are counter arguments on both sides. But the current situation has led to great uncertainty and, in many cases, grief,” Goodman said.
Donors should bear some moral responsibility for their role in reproduction by allowing their identity to be disclosed to donor-conceived individuals when they turn 18, Goodman added, noting that “there are counter arguments on both sides. But the current situation has led to great uncertainty and, in many cases, grief.”
Adams, the Jersey City woman who learned she was Jewish, has channeled these feelings into several works of art and performances on stage at venues such as the Jersey City Theater Center. During these performances, she describes the trauma of “not knowing where we come from [or] who we look like.”
In the last five years, Kathleen “Casey” DiPaola, a lawyer in Albany, New York, who focuses her practice on adoption, assisted reproduction and surrogacy, has observed a big shift toward would-be parents looking to use known sperm donors. On the other hand, with egg donation, “I’m not seeing a whole lot of change,” she said. Compared to sperm donation, more medical screening is involved with egg donation, so donors are primarily found through fertility clinics and egg donor agencies that prefer anonymity. This leads to fewer options for prospective parents seeking an egg donor with disclosed identity, DiPaola said.
Some donors want to keep in touch
Rachel Lemmons, 32, who lives in Denver, grew interested in becoming an egg donor when, as a graduate student in environmental sciences, she saw an online advertisement. “It seemed like a good way to help pay off my student loan debt,” said Lemmons, who is married and has a daughter who will turn 2-years-old in December. She didn’t end up donating until many years later, after she’d paid off the debt. “The primary motivation at that point wasn’t financial,” she said. “Instead, it felt like a really wonderful way to help someone else have a family in a few weeks’ time.”
Lemmons originally donated anonymously because she didn’t know open donations existed. She was content with that until she became aware of donor-conceived individuals’ struggles. “It concerned me that I could potentially be contributing to this,” she said, adding that the egg donor and surrogacy agency and fertility clinic wouldn’t allow her to disclose her identity retroactively.
Since then, she has donated as an open donor, and kept in touch with the recipients through email and video calls. Knowing that they were finally able to have children is “incredibly rewarding,” Lemmons said.
When to tell the kids
Stanton Honig, professor of urology and division chief of sexual and reproductive medicine at Yale School of Medicine, said for years his team has recommended that couples using donor sperm inform children about the role of the donor and their identity. “Honesty is always the best policy, and it is likely that when they become of age, they might or will be able to find out about their biological sperm donor,” he said. “Hiding it creates more of a complicated situation for children in the long run.”
Amy Jones, a 45-year-old resident of Syracuse, N.Y., has three children, including twins, who know they were conceived with anonymous donor eggs from the same individual, so they share the same genetics. Jones, who is a registered nurse and asked for her real name not to be published, told them around age seven.
“The thought of using a known donor brought more concerns—what if she wanted my babies after they were born, or how would I feel if she treated them as her own every time I saw her?” said Jones.
“I did a lot of reading, and all psychologists said that it is best to start the conversation early,” she recalled. “They understood very little of what I was telling them, but through the years, I have brought it up in discussion and encouraged them to ask questions. To this day, they don't seem to be all that interested, but I expect that later on in life they may have more questions.”
Jones and her husband opted to use a donor because premature ovarian failure at age 27 had rendered her infertile. “The decision to use an egg donor was hard enough,” she said. “The thought of using a known donor brought more concerns—what if she wanted my babies after they were born, or how would I feel if she treated them as her own every time I saw her?”
Susan C. Klock, a clinical psychologist in the section of fertility and reproductive medicine at Northwestern University Feinberg School of Medicine, said, “Anonymity is virtually impossible in the age of direct-to-consumer genetic testing.” In addition, “selecting an identity-release donor is typically not the first thing parents are looking at when they select a donor. First and foremost, they are looking for a donor with a healthy medical background. Then they may consider donor characteristics that resemble the parents.”
The donor’s medical history can be critical
Donor agencies rely on the self-reported medical history of egg and sperm donors, which can lead to gaps in learning important information. Knowing a donor’s medical history may have led some families to make different or more well-informed choices.
After Steven Gunner, a donor-conceived adult, suffered from schizophrenia and died of a drug overdose at age 27 in 2020, his parents, who live in New York, learned of a potential genetic link to his mental illness. A website, Donor Sibling Registry, revealed that the sperm donor the couple had used, a college student at the time of donation, had been hospitalized during childhood for schizophrenia and died of a drug overdose at age 46. Gunner’s story inspired Steven’s Law, a bill that was introduced in Congress in July. If passed, it would mandate sperm banks to collect information on donors’ medical conditions, and donors would have to disclose medical information the banks weren’t able to find.
With limited exceptions, the U.S. Food and Drug Administration requires donors to be screened and tested for relevant communicable disease agents and diseases such as HIV, hepatitis viruses B and C, the Zika virus and several STDs. With current technology, it is also impossible to screen for thousands of rare genetic diseases. “If a couple is using IVF (in vitro fertilization) to conceive with the donor gamete, some may opt for pre-implantation genetic testing to assess for chromosomal abnormalities,” Klock said.
Even these precautions wouldn't cover every disease, and some would-be parents don't get the genetic screening. In a situation where one donor has a large number of offspring, it is concerning that he or she can spread a rare disease to multiple people, said Nick Isel, 37, of Yorkville, Illinois, who was conceived with donor sperm due to his parents’ fertility issues. They told him the truth when he was a teenager, and he found his biological father with a journalist’s help.
Since 2016, Isel, who owns a roofing company, has been petitioning the FDA to extend the retention of medical records, requiring the fertility establishment to maintain information on sperm and egg donors for 50 years instead of the current 10-year mandate.
“The lack of family health information,” he said, “is an ongoing, slow-motion public health crisis since donor conception began being regulated by the FDA as a practice.”

