Interview with Jamie Metzl: We need a global OS upgrade

Jamie Metzl, author of Hacking Darwin, shares his views with Leaps.org on the future of genetics, tech, healthcare and more.
In this Q&A, leading technology and healthcare futurist Jamie Metzl discusses a range of topics and trend lines that will unfold over the next several decades: whether a version of Moore's Law applies to genetic technologies, the ethics of genetic engineering, the dangers of gene hacking, the end of sex, and much more.
Metzl is a member of the WHO expert advisory committee on human genome editing and the bestselling author of Hacking Darwin.
The conversation was lightly edited by Leaps.org for style and length.
In Hacking Darwin, you describe how we may modify the human body with CRISPR technologies, initially to obtain unsurpassed sports performance and then to enhance other human characteristics. What would such power over human biology mean for the future of our civilization?
After nearly four billion years of evolution, our one species suddenly has the increasing ability to read, write, and hack the code of life. This will have massive implications across the board, including in human health and reproduction, plant and animal agriculture, energy and advanced materials, and data storage and computing, just to name a few. My book Hacking Darwin: Genetic Engineering and the Future of Humanity primarly explored how we are currently deploying and will increasingly use our capabilities to transform human life in novel ways. My next book, The Great Biohack: Recasting Life in an Age of Revolutionary Technology, coming out in May 2024, will examine the broader implications for all of life on Earth.
We humans will, over time, use these technologies on ourselves to solve problems and eventually to enhance our capabilities. We need to be extremely conservative, cautious, and careful in doing so, but doing so will almost certainly be part of our future as a species.
In electronics, Moore's law is an established theory that computing power doubles every 18 months. Is there any parallel to be drawn with genetic technologies?
The increase in speed and decrease in costs of genome sequencing have progressed far faster than Moore’s law. It took thirteen years and cost about a billion dollars to sequence the first human genome. Today it takes just a few hours and can cost as little as a hundred dollars to do a far better job. In 2012, Jennifer Doudna and Emmanuel Charpentier published the basic science paper outlining the CRISPR-cas9 genome editing tool that would eventually win them the Nobel prize. Only six years later, the first CRISPR babies were born in China. If it feels like technology is moving ever-faster, that’s because it is.
Let's turn to the topic of aging. Do you think that the field of genetics will advance fast enough to eventually increase maximal lifespan for a child born this year? How about for a person who is currently age 50?
The science of aging is definitely real, but that doesn’t mean we will live forever. Aging is a biological process subject to human manipulation. Decades of animal research shows that. This does not mean we will live forever, but it does me we will be able to do more to expand our healthspans, the period of our lives where we are able to live most vigorously.
The first thing we need to do is make sure everyone on earth has access to the resources necessary to live up to their potential. I live in New York City, and I can take a ten minute subway ride to a neighborhood where the average lifespan is over a decade shorter than in mine. This is true within societies and between countries as well. Secondly, we all can live more like people in the Blue Zones, parts of the world where people live longer, on average, than the rest of us. They get regular exercise, eat healthy foods, have strong social connections, etc. Finally, we will all benefit, over time, from more scientific interventions to extend our healthspan. This may include small molecule drugs like metformin, rapamycin, and NAD+ boosters, blood serum infusions, and many other things.
Science fiction has depicted a future where we will never get sick again, stay young longer or become immortal. Assuming that any of this is remotely possible, should we be afraid of such changes, even if they seem positive in some regards, because we can’t understand the full implications at this point?
Not all of these promises will be realized in full, but we will use these technologies to help us live healthier, longer lives. We will never become immortal becasue nothing lasts forever. We will always get sick, even if the balance of diseases we face shifts over time, as it has always done. It is healthy, and absolutely necessary, that we feel both hope and fear about this future. If we only feel hope, we will blind ourselves to the very real potential downsides. If we only feel fear, we will deny ourselves the very meaningful benefits these technologies have the potential to provide.
A fascinating chapter in Hacking Darwin is entitled The End of Sex. And you see that as a good thing?
We humans will always be a sexually reproducing species, it’s just that we’ll reproduce increasingly less through the physical act of sex. We’re already seeing this with IVF. As the benefits of technology assisted reproduction increase relative to reproduction through the act of sex, many people will come to see assisted reproduction as a better way to reduce risk and, over time, possibly increase benefits. We’ll still have sex for all the other wonderful reasons we have it today, just less for reproduction. There will always be a critical place in our world for Italian romantics!
What are dangers of genetic hackers, perhaps especially if everyone’s DNA is eventually transcribed for medical purposes and available on the internet and in the cloud?
The sky is really the limit for how we can use gentic technologies to do things we may want, and the sky is also the limit for potential harms. It’s quite easy to imagine scenarios in which malevolent actors create synthetic pathogens designed to wreak havoc, or where people steal and abuse other people’s genetic information. It wouldn’t even need to be malevolent actors. Even well-intentioned researchers making unintended mistakes could cause real harm, as we may have seen with COVID-19 if, as appears likely to me, the pandemic stems for a research related incident]. That’s why we need strong governance and regulatory systems to optimize benefits and minimize potential harms. I was honored to have served on the World Health Organization Expert Advisory Committee on Human Genome Editing, were we developed a proposed framework for how this might best be achieved.
You foresee the equivalent of a genetic arms race between the world's most powerful countries. In what sense are genetic technologies similar to weapons?
Genetic technologies could be used to create incredibly powerful bioweapons or to build gene drives with the potential to crash entire ecosystems. That’s why thoughtful regulation is in order. Because the benefits of mastering and deploying these technologies are so great, there’s also a real danger of a genetics arms race. This could be extremely dangerous and will need to be prevented.
In your book, you express concern that states lacking Western conceptions of human rights are especially prone to misusing the science of genetics. Does this same concern apply to private companies? How much can we trust them to control and wield these technologies?
This is a conversation about science and technology but it’s really a conversation about values. If we don’t agree on what core values should be promoted, it will be nearly impossible to agree on what actions do and do not make sense. We need norms, laws, and values frameworks that apply to everyone, including governments, corporations, researchers, healthcare providers, DiY bio hobbyists, and everyone else.
We have co-evolved with our technology for a very long time. Many of our deepest beliefs have formed in that context and will continue to do so. But as we take for ourselves the powers we have attributed to our various gods, many of these beliefs will be challenged. We can not and must not jettison our beliefs in the face of technology, and must instead make sure our most cherished values guide the application of our most powerful technologies.
A conversation on international norms is in full swing in the field of AI, prompted by the release of ChatGPT4 earlier this year. Are there ways in which it’s inefficient, shortsighted or otherwise problematic for these discussions on gene technologies, AI and other advances to be occurring in silos? In addition to more specific guidelines, is there something to be gained from developing a universal set of norms and values that applies more broadly to all innovation?
AI is yet another technology where the potential to do great good is tied to the potential to inflict signifcant harm. It makes no sense that we tend to treat each technology on its own rather than looking at the entire category of challenges. For sure, we need to very rapidly ramp up our efforts with regard to AI norm-setting, regulations, and governance at all levels. But just doing that will be kind of like generating a flu vaccine for each individual flu strain. Far better to build a universal flu vaccine addressing common elements of all flu viruses of concern.
That’s why we also need to be far more deliberate in both building a global operating systems based around the mutual responsibilities of our global interdependence and, under that umbrella, a broader system for helping us govern and regulate revolutionary technologies. Such a process might begin with a large international conference, the equivalent of Rio 1992 for climate change, but then quickly work to establish and share best practices, help build parallel institutions in all countries so people and governamts can talk with each other, and do everything possible to maximize benefits and minimize risks at all levels in an ongoing and dynamic way.
At what point might genetic enhancements lead to a reclassfication of modified humans as another species?
We’ll still all be fellow humans for a very, very long time. We already have lots of variation between us. That is the essence of biology. Will some humans, at some point in the future, leave Earth and spend generations elsewhere? I believe so. In those new environments, humans will evolve, over time, differently than those if us who remain on this planet? This may sound like science fiction, but the sci-fi future is coming at us faster than most people realize.
Is the concept of human being changing?
Yes. It always has and always will.
Another big question raised in your book: what limits should we impose on the freedom to manipulate genetics?
Different societies will come to different conclusion on this critical question. I am sympathetic to the argument that people should have lots of say over their own bodies, which why I support abortion rights even though I recognize that an abortion can be a violent procedure. But it would be insane and self-defeating to say that individuals have an unlimited right to manipulate their own or their future children’s heritable genetics. The future of human life is all of our concern and must be regulated, albeit wisely.
In some cases, such as when we have the ability to prevent a deadly genetic disroder, it might be highly ethical to manipulate other human beings. In other circumstances, the genetic engineering of humans might be highly unethical. The key point is to avoid asking this question in a binary manner. We need to weigh the costs and benefits of each type of intervention. We need societal and global infrastrucutres to do that well. We don’t yet have those but we need them badly.
Can you tell us more about your next book?
The Great Biohack: Recasting Lifee in an Age of Revolutionary Technology, will come out in May 2024. It explores what the intersecting AI, genetics, and biotechnology revolutions will mean for the future of life on earth, including our healthcare, agriculture, industry, computing, and everything else. We are at a transitional moment for life on earth, equivalent to the dawn of agriculture, electricity, and industrialization. The key differentiator between better and worse outcomes is what we do today, at this early stage of this new transformation. The book describes what’s happening, what’s at stake, and what we each and all can and, frankly, must do to build the type of future we’d like to inhabit.
You’ve been a leader of international efforts calling for a full investigation into COVID-19 origins and are the founder of the global movement OneShared.World. What problem are you trying to solve through OneShared.World?
The biggest challenge we face today is the mismatch between the nature of our biggest problems, global and common, and the absence of a sufficient framework for addressing that entire category of challenges. The totally avoidable COVID-19 pandemic is one example of the extremet costs of the status quo. OneShared.World is our effort to fight for an upgrade in our world’s global operating system, based around the mutual responsibilities of interdependence. We’ve had global OS upgrades before after the Thirty Years War and after World War II, but wouldn’t it be better to make the necessary changes now to prevent a crisis of that level stemming from a nuclear war, ecosystem collapse, or deadlier synthetic biology pandemic rather than waiting until after? Revolutionary science is a global issue that must be wisely managed at every level if it is to be wisely managed at all.
How do we ensure that revolutionary technologies benefit humanity instead of undermining it?
That is the essential question. It’s why I’ve written Hacking Darwin, am writing The Great Biohack, and doing the rest of my work. If we want scietific revolutions to help, rather than hurt, us, we must all play a role building that future. This isn’t just a conversation about science, it’s about how we can draw on our most cherished values to guide the optimal development of science and technology for the common good. That must be everyone’s business.
Portions of this interview were first published in Grassia (Italy) and Zen Portugal.
Jamie Metzl is one of the world’s leading technology and healthcare futurists and author of the bestselling book, Hacking Darwin: Genetic Engineering and the Future of Humanity, which has been translated into 15 languages. In 2019, he was appointed to the World Health Organization expert advisory committee on human genome editing. Jamie is a faculty member of Singularity University and NextMed Health, a Senior Fellow of the Atlantic Council, and Founder and Chair of the global social movement, OneShared.World.
Called “the original COVID-19 whistleblower,” his pioneering role advocating for a full investigation into the origins of the COVID-19 pandemic has been featured in 60 Minutes, the New York Times, and most major media across the globe, and he was the lead witness in the first congressional hearings on this topic. Jamie previously served in the U.S. National Security Council, State Department, and Senate Foreign Relations Committee and with the United Nations in Cambodia. Jamie appears regularly on national and international media and his syndicated columns and other writing in science, technology, and global affairs are featured in publications around the world.
Jamie sits on advisory boards for multiple biotechnology and other companies and is Special Strategist to the WisdomTree BioRevolution Exchange Traded Fund. In addition to Hacking Darwin, he is author of a history of the Cambodian genocide, the historical novel The Depths of the Sea, and the genetics sci-fi thrillers Genesis Code and Eternal Sonata. His next book, The Great Biohack: Recasting Life in an age of Revolutionary Technology, will be published by Hachette in May 2024. Jamie holds a Ph.D. from Oxford, a law degree from Harvard, and an undergraduate degree from Brown and is an avid ironman triathlete and ultramarathon runner.
Tiny, tough “water bears” may help bring new vaccines and medicines to sub-Saharan Africa
Tardigrades can completely dehydrate and later rehydrate themselves, a survival trick that scientists are harnessing to preserve medicines in hot temperatures.
Microscopic tardigrades, widely considered to be some of the toughest animals on earth, can survive for decades without oxygen or water and are thought to have lived through a crash-landing on the moon. Also known as water bears, they survive by fully dehydrating and later rehydrating themselves – a feat only a few animals can accomplish. Now scientists are harnessing tardigrades’ talents to make medicines that can be dried and stored at ambient temperatures and later rehydrated for use—instead of being kept refrigerated or frozen.
Many biologics—pharmaceutical products made by using living cells or synthesized from biological sources—require refrigeration, which isn’t always available in many remote locales or places with unreliable electricity. These products include mRNA and other vaccines, monoclonal antibodies and immuno-therapies for cancer, rheumatoid arthritis and other conditions. Cooling is also needed for medicines for blood clotting disorders like hemophilia and for trauma patients.
Formulating biologics to withstand drying and hot temperatures has been the holy grail for pharmaceutical researchers for decades. It’s a hard feat to manage. “Biologic pharmaceuticals are highly efficacious, but many are inherently unstable,” says Thomas Boothby, assistant professor of molecular biology at University of Wyoming. Therefore, during storage and shipping, they must be refrigerated at 2 to 8 degrees Celsius (35 to 46 degrees Fahrenheit). Some must be frozen, typically at -20 degrees Celsius, but sometimes as low -90 degrees Celsius as was the case with the Pfizer Covid vaccine.
For Covid, fewer than 73 percent of the global population received even one dose. The need for refrigerated or frozen handling was partially to blame.
The costly cold chain
The logistics network that ensures those temperature requirements are met from production to administration is called the cold chain. This cold chain network is often unreliable or entirely lacking in remote, rural areas in developing nations that have malfunctioning electrical grids. “Almost all routine vaccines require a cold chain,” says Christopher Fox, senior vice president of formulations at the Access to Advanced Health Institute. But when the power goes out, so does refrigeration, putting refrigerated or frozen medical products at risk. Consequently, the mRNA vaccines developed for Covid-19 and other conditions, as well as more traditional vaccines for cholera, tetanus and other diseases, often can’t be delivered to the most remote parts of the world.
To understand the scope of the challenge, consider this: In the U.S., more than 984 million doses of Covid-19 vaccine have been distributed so far. Each one needed refrigeration that, even in the U.S., proved challenging. Now extrapolate to all vaccines and the entire world. For Covid, fewer than 73 percent of the global population received even one dose. The need for refrigerated or frozen handling was partially to blame.

Globally, the cold chain packaging market is valued at over $15 billion and is expected to exceed $60 billion by 2033.
Adobe Stock
Freeze-drying, also called lyophilization, which is common for many vaccines, isn’t always an option. Many freeze-dried vaccines still need refrigeration, and even medicines approved for storage at ambient temperatures break down in the heat of sub-Saharan Africa. “Even in a freeze-dried state, biologics often will undergo partial rehydration and dehydration, which can be extremely damaging,” Boothby explains.
The cold chain is also very expensive to maintain. The global pharmaceutical cold chain packaging market is valued at more than $15 billion, and is expected to exceed $60 billion by 2033, according to a report by Future Market Insights. This cost is only expected to grow. According to the consulting company Accenture, the number of medicines that require the cold chain are expected to grow by 48 percent, compared to only 21 percent for non-cold-chain therapies.
Tardigrades to the rescue
Tardigrades are only about a millimeter long – with four legs and claws, and they lumber around like bears, thus their nickname – but could provide a big solution. “Tardigrades are unique in the animal kingdom, in that they’re able to survive a vast array of environmental insults,” says Boothby, the Wyoming professor. “They can be dried out, frozen, heated past the boiling point of water and irradiated at levels that are thousands of times more than you or I could survive.” So, his team is gradually unlocking tardigrades’ survival secrets and applying them to biologic pharmaceuticals to make them withstand both extreme heat and desiccation without losing efficacy.
Boothby’s team is focusing on blood clotting factor VIII, which, as the name implies, causes blood to clot. Currently, Boothby is concentrating on the so-called cytoplasmic abundant heat soluble (CAHS) protein family, which is found only in tardigrades, protecting them when they dry out. “We showed we can desiccate a biologic (blood clotting factor VIII, a key clotting component) in the presence of tardigrade proteins,” he says—without losing any of its effectiveness.
The researchers mixed the tardigrade protein with the blood clotting factor and then dried and rehydrated that substance six times without damaging the latter. This suggests that biologics protected with tardigrade proteins can withstand real-world fluctuations in humidity.
Furthermore, Boothby’s team found that when the blood clotting factor was dried and stabilized with tardigrade proteins, it retained its efficacy at temperatures as high as 95 degrees Celsius. That’s over 200 degrees Fahrenheit, much hotter than the 58 degrees Celsius that the World Meteorological Organization lists as the hottest recorded air temperature on earth. In contrast, without the protein, the blood clotting factor degraded significantly. The team published their findings in the journal Nature in March.
Although tardigrades rarely live more than 2.5 years, they have survived in a desiccated state for up to two decades, according to Animal Diversity Web. This suggests that tardigrades’ CAHS protein can protect biologic pharmaceuticals nearly indefinitely without refrigeration or freezing, which makes it significantly easier to deliver them in locations where refrigeration is unreliable or doesn’t exist.
The tricks of the tardigrades
Besides the CAHS proteins, tardigrades rely on a type of sugar called trehalose and some other protectants. So, rather than drying up, their cells solidify into rigid, glass-like structures. As that happens, viscosity between cells increases, thereby slowing their biological functions so much that they all but stop.
Now Boothby is combining CAHS D, one of the proteins in the CAHS family, with trehalose. He found that CAHS D and trehalose each protected proteins through repeated drying and rehydrating cycles. They also work synergistically, which means that together they might stabilize biologics under a variety of dry storage conditions.
“We’re finding the protective effect is not just additive but actually is synergistic,” he says. “We’re keen to see if something like that also holds true with different protein combinations.” If so, combinations could possibly protect against a variety of conditions.
Commercialization outlook
Before any stabilization technology for biologics can be commercialized, it first must be approved by the appropriate regulators. In the U.S., that’s the U.S. Food and Drug Administration. Developing a new formulation would require clinical testing and vast numbers of participants. So existing vaccines and biologics likely won’t be re-formulated for dry storage. “Many were developed decades ago,” says Fox. “They‘re not going to be reformulated into thermo-stable vaccines overnight,” if ever, he predicts.
Extending stability outside the cold chain, even for a few days, can have profound health, environmental and economic benefits.
Instead, this technology is most likely to be used for the new products and formulations that are just being created. New and improved vaccines will be the first to benefit. Good candidates include the plethora of mRNA vaccines, as well as biologic pharmaceuticals for neglected diseases that affect parts of the world where reliable cold chain is difficult to maintain, Boothby says. Some examples include new, more effective vaccines for malaria and for pathogenic Escherichia coli, which causes diarrhea.
Tallying up the benefits
Extending stability outside the cold chain, even for a few days, can have profound health, environmental and economic benefits. For instance, MenAfriVac, a meningitis vaccine (without tardigrade proteins) developed for sub-Saharan Africa, can be stored at up to 40 degrees Celsius for four days before administration. “If you have a few days where you don’t need to maintain the cold chain, it’s easier to transport vaccines to remote areas,” Fox says, where refrigeration does not exist or is not reliable.
Better health is an obvious benefit. MenAfriVac reduced suspected meningitis cases by 57 percent in the overall population and more than 99 percent among vaccinated individuals.
Lower healthcare costs are another benefit. One study done in Togo found that the cold chain-related costs increased the per dose vaccine price up to 11-fold. The ability to ship the vaccines using the usual cold chain, but transporting them at ambient temperatures for the final few days cut the cost in half.
There are environmental benefits, too, such as reducing fuel consumption and greenhouse gas emissions. Cold chain transports consume 20 percent more fuel than non-cold chain shipping, due to refrigeration equipment, according to the International Trade Administration.
A study by researchers at Johns Hopkins University compared the greenhouse gas emissions of the new, oral Vaxart COVID-19 vaccine (which doesn’t require refrigeration) with four intramuscular vaccines (which require refrigeration or freezing). While the Vaxart vaccine is still in clinical trials, the study found that “up to 82.25 million kilograms of CO2 could be averted by using oral vaccines in the U.S. alone.” That is akin to taking 17,700 vehicles out of service for one year.
Although tardigrades’ protective proteins won’t be a component of biologic pharmaceutics for several years, scientists are proving that this approach is viable. They are hopeful that a day will come when vaccines and biologics can be delivered anywhere in the world without needing refrigerators or freezers en route.
Jamie Rettinger with his now fiance Amie Purnel-Davis, who helped him through the clinical trial.
Jamie Rettinger was still in his thirties when he first noticed a tiny streak of brown running through the thumbnail of his right hand. It slowly grew wider and the skin underneath began to deteriorate before he went to a local dermatologist in 2013. The doctor thought it was a wart and tried scooping it out, treating the affected area for three years before finally removing the nail bed and sending it off to a pathology lab for analysis.
"I have some bad news for you; what we removed was a five-millimeter melanoma, a cancerous tumor that often spreads," Jamie recalls being told on his return visit. "I'd never heard of cancer coming through a thumbnail," he says. None of his doctors had ever mentioned it either. "I just thought I was being treated for a wart." But nothing was healing and it continued to bleed.
A few months later a surgeon amputated the top half of his thumb. Lymph node biopsy tested negative for spread of the cancer and when the bandages finally came off, Jamie thought his medical issues were resolved.
Melanoma is the deadliest form of skin cancer. About 85,000 people are diagnosed with it each year in the U.S. and more than 8,000 die of the cancer when it spreads to other parts of the body, according to the Centers for Disease Control and Prevention (CDC).
There are two peaks in diagnosis of melanoma; one is in younger women ages 30-40 and often is tied to past use of tanning beds; the second is older men 60+ and is related to outdoor activity from farming to sports. Light-skinned people have a twenty-times greater risk of melanoma than do people with dark skin.
"When I graduated from medical school, in 2005, melanoma was a death sentence" --Diwakar Davar.
Jamie had a follow up PET scan about six months after his surgery. A suspicious spot on his lung led to a biopsy that came back positive for melanoma. The cancer had spread. Treatment with a monoclonal antibody (nivolumab/Opdivo®) didn't prove effective and he was referred to the UPMC Hillman Cancer Center in Pittsburgh, a four-hour drive from his home in western Ohio.
An alternative monoclonal antibody treatment brought on such bad side effects, diarrhea as often as 15 times a day, that it took more than a week of hospitalization to stabilize his condition. The only options left were experimental approaches in clinical trials.
Early research
"When I graduated from medical school, in 2005, melanoma was a death sentence" with a cure rate in the single digits, says Diwakar Davar, 39, an oncologist at UPMC Hillman Cancer Center who specializes in skin cancer. That began to change in 2010 with introduction of the first immunotherapies, monoclonal antibodies, to treat cancer. The antibodies attach to PD-1, a receptor on the surface of T cells of the immune system and on cancer cells. Antibody treatment boosted the melanoma cure rate to about 30 percent. The search was on to understand why some people responded to these drugs and others did not.
At the same time, there was a growing understanding of the role that bacteria in the gut, the gut microbiome, plays in helping to train and maintain the function of the body's various immune cells. Perhaps the bacteria also plays a role in shaping the immune response to cancer therapy.
One clue came from genetically identical mice. Animals ordered from different suppliers sometimes responded differently to the experiments being performed. That difference was traced to different compositions of their gut microbiome; transferring the microbiome from one animal to another in a process known as fecal transplant (FMT) could change their responses to disease or treatment.
When researchers looked at humans, they found that the patients who responded well to immunotherapies had a gut microbiome that looked like healthy normal folks, but patients who didn't respond had missing or reduced strains of bacteria.
Davar and his team knew that FMT had a very successful cure rate in treating the gut dysbiosis of Clostridioides difficile, a persistant intestinal infection, and they wondered if a fecal transplant from a patient who had responded well to cancer immunotherapy treatment might improve the cure rate of patients who did not originally respond to immunotherapies for melanoma.
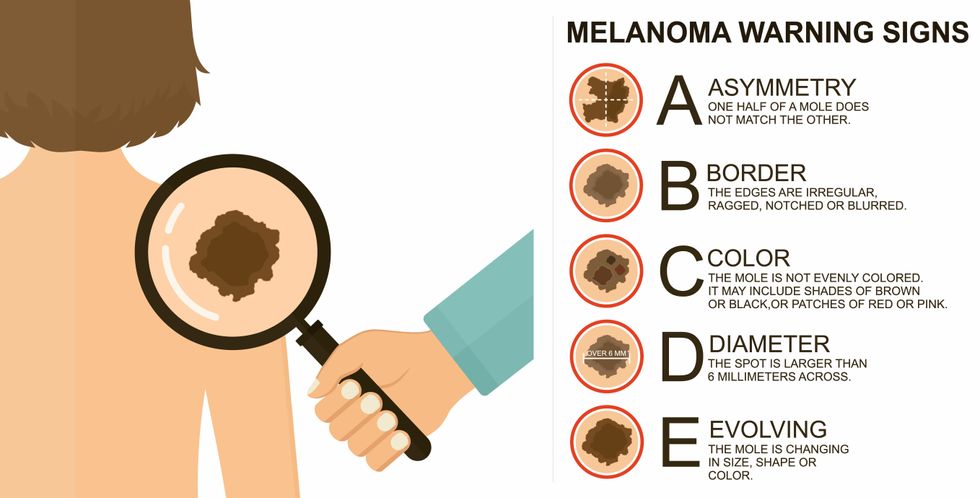
The ABCDE of melanoma detection
Adobe Stock
Clinical trial
"It was pretty weird, I was totally blasted away. Who had thought of this?" Jamie first thought when the hypothesis was explained to him. But Davar's explanation that the procedure might restore some of the beneficial bacterial his gut was lacking, convinced him to try. He quickly signed on in October 2018 to be the first person in the clinical trial.
Fecal donations go through the same safety procedures of screening for and inactivating diseases that are used in processing blood donations to make them safe for transfusion. The procedure itself uses a standard hollow colonoscope designed to screen for colon cancer and remove polyps. The transplant is inserted through the center of the flexible tube.
Most patients are sedated for procedures that use a colonoscope but Jamie doesn't respond to those drugs: "You can't knock me out. I was watching them on the TV going up my own butt. It was kind of unreal at that point," he says. "There were about twelve people in there watching because no one had seen this done before."
A test two weeks after the procedure showed that the FMT had engrafted and the once-missing bacteria were thriving in his gut. More importantly, his body was responding to another monoclonal antibody (pembrolizumab/Keytruda®) and signs of melanoma began to shrink. Every three months he made the four-hour drive from home to Pittsburgh for six rounds of treatment with the antibody drug.
"We were very, very lucky that the first patient had a great response," says Davar. "It allowed us to believe that even though we failed with the next six, we were on the right track. We just needed to tweak the [fecal] cocktail a little better" and enroll patients in the study who had less aggressive tumor growth and were likely to live long enough to complete the extensive rounds of therapy. Six of 15 patients responded positively in the pilot clinical trial that was published in the journal Science.
Davar believes they are beginning to understand the biological mechanisms of why some patients initially do not respond to immunotherapy but later can with a FMT. It is tied to the background level of inflammation produced by the interaction between the microbiome and the immune system. That paper is not yet published.
Surviving cancer
It has been almost a year since the last in his series of cancer treatments and Jamie has no measurable disease. He is cautiously optimistic that his cancer is not simply in remission but is gone for good. "I'm still scared every time I get my scans, because you don't know whether it is going to come back or not. And to realize that it is something that is totally out of my control."
"It was hard for me to regain trust" after being misdiagnosed and mistreated by several doctors he says. But his experience at Hillman helped to restore that trust "because they were interested in me, not just fixing the problem."
He is grateful for the support provided by family and friends over the last eight years. After a pause and a sigh, the ruggedly built 47-year-old says, "If everyone else was dead in my family, I probably wouldn't have been able to do it."
"I never hesitated to ask a question and I never hesitated to get a second opinion." But Jamie acknowledges the experience has made him more aware of the need for regular preventive medical care and a primary care physician. That person might have caught his melanoma at an earlier stage when it was easier to treat.
Davar continues to work on clinical studies to optimize this treatment approach. Perhaps down the road, screening the microbiome will be standard for melanoma and other cancers prior to using immunotherapies, and the FMT will be as simple as swallowing a handful of freeze-dried capsules off the shelf rather than through a colonoscopy. Earlier this year, the Food and Drug Administration approved the first oral fecal microbiota product for C. difficile, hopefully paving the way for more.
An older version of this hit article was first published on May 18, 2021

