A Rare Disease Just "Messed with the Wrong Mother." Now She's Fighting to Beat It Once and For All.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.

Amber Freed and Maxwell near their home in Denver, Colorado.
Amber Freed felt she was the happiest mother on earth when she gave birth to twins in March 2017. But that euphoric feeling began to fade over the next few months, as she realized her son wasn't making the same developmental milestones as his sister. "I had a perfect benchmark because they were twins, and I saw that Maxwell was floppy—he didn't have muscle tone and couldn't hold his neck up," she recalls. At first doctors placated her with statements that boys sometimes develop slower than girls, but the difference was just too drastic. At 10 month old, Maxwell had never reached to grab a toy. In fact, he had never even used his hands.
Thinking that perhaps Maxwell couldn't see well, Freed took him to an ophthalmologist who was the first to confirm her worst fears. He didn't find Maxwell to have vision problems, but he thought there was something wrong with the boy's brain. He had seen similar cases before and they always turned out to be rare disorders, and always fatal. "Start preparing yourself for your child not to live," he had said.
Getting the diagnosis took months of painful, invasive procedures, as well as fighting with the health insurance to get the genetic testing approved. Finally, in June 2018, doctors at the Children's Hospital Colorado gave the Freeds their son's diagnosis—a genetic mutation so rare it didn't even have a name, just a bunch of letters jammed together into a word SLC6A1—same as the name of the mutated gene. The mutation, with only 40 cases known worldwide at the time, caused developmental disabilities, movement and speech disorders, and a debilitating form of epilepsy.
The doctors didn't know much about the disorder, but they said that Maxwell would also regress in his development when he turned three or four. They couldn't tell how long he would live. "Hopefully you would become an expert and educate us about it," they said, as they gave Freed a five-page paper on the SLC6A1 and told her to start calling scientists if she wanted to help her son in any way. When she Googled the name, nothing came up. She felt horrified. "Our disease was too rare to care."
Freed's husband, a 6'2'' college football player broke down in sobs and she realized that if anything could be done to help Maxwell, she'd have be the one to do it. "I understood that I had to fight like a mother," she says. "And a determined mother can do a lot of things."

The Freed family.
Courtesy Amber Freed
She quit her job as an equity analyst the day of the diagnosis and became a full-time SLC6A1 citizen scientist looking for researchers studying mutations of this gene. In the wee hours of the morning, she called scientists in Europe. As the day progressed, she called researchers on the East Coast, followed by the West in the afternoon. In the evening, she switched to Asia and Australia. She asked them the same question. "Can you help explain my gene and how do we fix it?"
Scientists need money to do research, so Freed launched Milestones for Maxwell fundraising campaign, and a SLC6A1 Connect patient advocacy nonprofit, dedicated to improving the lives of children and families battling this rare condition. And then it became clear that the mutation wasn't as rare as it seemed. As other parents began to discover her nonprofit, the number of known cases rose from 40 to 100, and later to 400, Freed says. "The disease is only rare until it messes with the wrong mother."
It took one mother to find another to start looking into what's happening inside Maxwell's brain. Freed came across Jeanne Paz, a Gladstone Institutes researcher who studies epilepsy with particular interest in absence or silent seizures—those that don't manifest by convulsions, but rather make patients absently stare into space—and that's one type of seizures Maxwell has. "It's like a brief period of silence in the brain during which the person doesn't pay attention to what's happening, and as soon as they come out of the seizure they are back to life," Paz explains. "It's like a pause button on consciousness." She was working to understand the underlying biology.
To understand how seizures begin, spread and stop, Paz uses optogenetics in mice. From words "genetic" and "optikós," which means visible in Greek, the optogenetics technique involves two steps. First, scientists introduce a light-sensitive gene into a specific brain cell type—for example into excitatory neurons that release glutamate, a neurotransmitter, which activates other cells in the brain. Then they implant a very thin optical fiber into the brain area where they forged these light-sensitive neurons. As they shine the light through the optical fiber, researchers can make excitatory neurons to release glutamate—or instead tell them to stop being active and "shut up". The ability to control what these neurons of interest do, quite literally sheds light onto where seizures start, how they propagate and what cells are involved in stopping them.
"Let's say a seizure started and we shine the light that reduces the activity of specific neurons," Paz explains. "If that stops the seizure, we know that activating those cells was necessary to maintain the seizure." Likewise, shutting down their activity will make the seizure stop.
Freed reached out to Paz in 2019 and the two women had an instant connection. They were both passionate about brain and seizures research, even if for different reasons. Freed asked Paz if she would study her son's seizures and Paz agreed.
To do that, Paz needed mice that carried the SLC6A1 mutation, so Freed found a company in China that created them to specs. The company replaced a mouse SLC6A1 gene with a human mutated one and shipped them over to Paz's lab. "We call them Maxwell mice," Paz says, "and we are now implanting electrodes into them to see which brain regions generate seizures." That would help them understand what goes wrong and what brain cells are malfunctioning in the SLC6A1 mice—and help scientists better understand what might cause seizures in children.
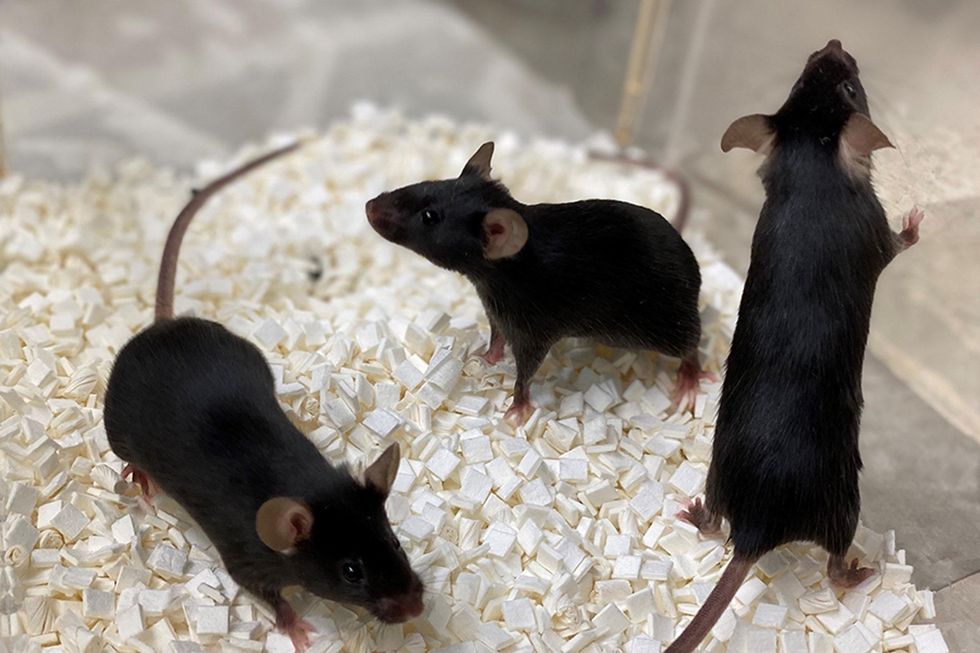
Bred to carry SLC6A1 mutation, these "Maxwell mice" will help better understand this debilitating genetic disease. (These mice are from Vanderbilt University, where researchers are also studying SLC6A1.)
Courtesy Amber Freed
This information—along with other research Amber is funding in other institutions—will inform the development of a novel genetic treatment, in which scientists would deploy a harmless virus to deliver a healthy, working copy of the SLC6A1 gene into the mice brains. They would likely deliver the therapeutic via a spinal tap infusion, and if it works and doesn't produce side effects in mice, the human trials will follow.
In the meantime, Freed is raising money to fund other research of various stop-gap measures. On April 22, 2021, she updated her Milestone for Maxwell page with a post that her nonprofit is funding yet another effort. It is a trial at Weill Cornell Medicine in New York City, in which doctors will use an already FDA-approved drug, which was recently repurposed for the SLC6A1 condition to treat epilepsy in these children. "It will buy us time," Freed says—while the gene therapy effort progresses.
Freed is determined to beat SLC6A1 before it beats down her family. She hopes to put an end to this disease—and similar genetic diseases—once and for all. Her goal is not only to have scientists create a remedy, but also to add the mutation to a newborn screening panel. That way, children born with this condition in the future would receive gene therapy before they even leave the hospital.
"I don't want there to be another Maxwell Freed," she says, "and that's why I am fighting like a mother." The gene therapy trial still might be a few years away, but the Weill Cornell one aims to launch very soon—possibly around Mother's Day. This is yet another milestone for Maxwell, another baby step forward—and the best gift a mother can get.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.
A new type of cancer therapy is shrinking deadly brain tumors with just one treatment
MRI scans after a new kind of immunotherapy for brain cancer show remarkable progress in one patient just days after the first treatment.
Few cancers are deadlier than glioblastomas—aggressive and lethal tumors that originate in the brain or spinal cord. Five years after diagnosis, less than five percent of glioblastoma patients are still alive—and more often, glioblastoma patients live just 14 months on average after receiving a diagnosis.
But an ongoing clinical trial at Mass General Cancer Center is giving new hope to glioblastoma patients and their families. The trial, called INCIPIENT, is meant to evaluate the effects of a special type of immune cell, called CAR-T cells, on patients with recurrent glioblastoma.
How CAR-T cell therapy works
CAR-T cell therapy is a type of cancer treatment called immunotherapy, where doctors modify a patient’s own immune system specifically to find and destroy cancer cells. In CAR-T cell therapy, doctors extract the patient’s T-cells, which are immune system cells that help fight off disease—particularly cancer. These T-cells are harvested from the patient and then genetically modified in a lab to produce proteins on their surface called chimeric antigen receptors (thus becoming CAR-T cells), which makes them able to bind to a specific protein on the patient’s cancer cells. Once modified, these CAR-T cells are grown in the lab for several weeks so that they can multiply into an army of millions. When enough cells have been grown, these super-charged T-cells are infused back into the patient where they can then seek out cancer cells, bind to them, and destroy them. CAR-T cell therapies have been approved by the US Food and Drug Administration (FDA) to treat certain types of lymphomas and leukemias, as well as multiple myeloma, but haven’t been approved to treat glioblastomas—yet.
CAR-T cell therapies don’t always work against solid tumors, such as glioblastomas. Because solid tumors contain different kinds of cancer cells, some cells can evade the immune system’s detection even after CAR-T cell therapy, according to a press release from Massachusetts General Hospital. For the INCIPIENT trial, researchers modified the CAR-T cells even further in hopes of making them more effective against solid tumors. These second-generation CAR-T cells (called CARv3-TEAM-E T cells) contain special antibodies that attack EFGR, a protein expressed in the majority of glioblastoma tumors. Unlike other CAR-T cell therapies, these particular CAR-T cells were designed to be directly injected into the patient’s brain.
The INCIPIENT trial results
The INCIPIENT trial involved three patients who were enrolled in the study between March and July 2023. All three patients—a 72-year-old man, a 74-year-old man, and a 57-year-old woman—were treated with chemo and radiation and enrolled in the trial with CAR-T cells after their glioblastoma tumors came back.
The results, which were published earlier this year in the New England Journal of Medicine (NEJM), were called “rapid” and “dramatic” by doctors involved in the trial. After just a single infusion of the CAR-T cells, each patient experienced a significant reduction in their tumor sizes. Just two days after receiving the infusion, the glioblastoma tumor of the 72-year-old man decreased by nearly twenty percent. Just two months later the tumor had shrunk by an astonishing 60 percent, and the change was maintained for more than six months. The most dramatic result was in the 57-year-old female patient, whose tumor shrank nearly completely after just one infusion of the CAR-T cells.
The results of the INCIPIENT trial were unexpected and astonishing—but unfortunately, they were also temporary. For all three patients, the tumors eventually began to grow back regardless of the CAR-T cell infusions. According to the press release from MGH, the medical team is now considering treating each patient with multiple infusions or prefacing each treatment with chemotherapy to prolong the response.
While there is still “more to do,” says co-author of the study neuro-oncologist Dr. Elizabeth Gerstner, the results are still promising. If nothing else, these second-generation CAR-T cell infusions may someday be able to give patients more time than traditional treatments would allow.
“These results are exciting but they are also just the beginning,” says Dr. Marcela Maus, a doctor and professor of medicine at Mass General who was involved in the clinical trial. “They tell us that we are on the right track in pursuing a therapy that has the potential to change the outlook for this intractable disease.”
A recent study in The Lancet Oncology showed that AI found 20 percent more cancers on mammogram screens than radiologists alone.
Since the early 2000s, AI systems have eliminated more than 1.7 million jobs, and that number will only increase as AI improves. Some research estimates that by 2025, AI will eliminate more than 85 million jobs.
But for all the talk about job security, AI is also proving to be a powerful tool in healthcare—specifically, cancer detection. One recently published study has shown that, remarkably, artificial intelligence was able to detect 20 percent more cancers in imaging scans than radiologists alone.
Published in The Lancet Oncology, the study analyzed the scans of 80,000 Swedish women with a moderate hereditary risk of breast cancer who had undergone a mammogram between April 2021 and July 2022. Half of these scans were read by AI and then a radiologist to double-check the findings. The second group of scans was read by two researchers without the help of AI. (Currently, the standard of care across Europe is to have two radiologists analyze a scan before diagnosing a patient with breast cancer.)
The study showed that the AI group detected cancer in 6 out of every 1,000 scans, while the radiologists detected cancer in 5 per 1,000 scans. In other words, AI found 20 percent more cancers than the highly-trained radiologists.

But even though the AI was better able to pinpoint cancer on an image, it doesn’t mean radiologists will soon be out of a job. Dr. Laura Heacock, a breast radiologist at NYU, said in an interview with CNN that radiologists do much more than simply screening mammograms, and that even well-trained technology can make errors. “These tools work best when paired with highly-trained radiologists who make the final call on your mammogram. Think of it as a tool like a stethoscope for a cardiologist.”
AI is still an emerging technology, but more and more doctors are using them to detect different cancers. For example, researchers at MIT have developed a program called MIRAI, which looks at patterns in patient mammograms across a series of scans and uses an algorithm to model a patient's risk of developing breast cancer over time. The program was "trained" with more than 200,000 breast imaging scans from Massachusetts General Hospital and has been tested on over 100,000 women in different hospitals across the world. According to MIT, MIRAI "has been shown to be more accurate in predicting the risk for developing breast cancer in the short term (over a 3-year period) compared to traditional tools." It has also been able to detect breast cancer up to five years before a patient receives a diagnosis.
The challenges for cancer-detecting AI tools now is not just accuracy. AI tools are also being challenged to perform consistently well across different ages, races, and breast density profiles, particularly given the increased risks that different women face. For example, Black women are 42 percent more likely than white women to die from breast cancer, despite having nearly the same rates of breast cancer as white women. Recently, an FDA-approved AI device for screening breast cancer has come under fire for wrongly detecting cancer in Black patients significantly more often than white patients.
As AI technology improves, radiologists will be able to accurately scan a more diverse set of patients at a larger volume than ever before, potentially saving more lives than ever.

