A Rare Disease Just "Messed with the Wrong Mother." Now She's Fighting to Beat It Once and For All.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.

Amber Freed and Maxwell near their home in Denver, Colorado.
Amber Freed felt she was the happiest mother on earth when she gave birth to twins in March 2017. But that euphoric feeling began to fade over the next few months, as she realized her son wasn't making the same developmental milestones as his sister. "I had a perfect benchmark because they were twins, and I saw that Maxwell was floppy—he didn't have muscle tone and couldn't hold his neck up," she recalls. At first doctors placated her with statements that boys sometimes develop slower than girls, but the difference was just too drastic. At 10 month old, Maxwell had never reached to grab a toy. In fact, he had never even used his hands.
Thinking that perhaps Maxwell couldn't see well, Freed took him to an ophthalmologist who was the first to confirm her worst fears. He didn't find Maxwell to have vision problems, but he thought there was something wrong with the boy's brain. He had seen similar cases before and they always turned out to be rare disorders, and always fatal. "Start preparing yourself for your child not to live," he had said.
Getting the diagnosis took months of painful, invasive procedures, as well as fighting with the health insurance to get the genetic testing approved. Finally, in June 2018, doctors at the Children's Hospital Colorado gave the Freeds their son's diagnosis—a genetic mutation so rare it didn't even have a name, just a bunch of letters jammed together into a word SLC6A1—same as the name of the mutated gene. The mutation, with only 40 cases known worldwide at the time, caused developmental disabilities, movement and speech disorders, and a debilitating form of epilepsy.
The doctors didn't know much about the disorder, but they said that Maxwell would also regress in his development when he turned three or four. They couldn't tell how long he would live. "Hopefully you would become an expert and educate us about it," they said, as they gave Freed a five-page paper on the SLC6A1 and told her to start calling scientists if she wanted to help her son in any way. When she Googled the name, nothing came up. She felt horrified. "Our disease was too rare to care."
Freed's husband, a 6'2'' college football player broke down in sobs and she realized that if anything could be done to help Maxwell, she'd have be the one to do it. "I understood that I had to fight like a mother," she says. "And a determined mother can do a lot of things."

The Freed family.
Courtesy Amber Freed
She quit her job as an equity analyst the day of the diagnosis and became a full-time SLC6A1 citizen scientist looking for researchers studying mutations of this gene. In the wee hours of the morning, she called scientists in Europe. As the day progressed, she called researchers on the East Coast, followed by the West in the afternoon. In the evening, she switched to Asia and Australia. She asked them the same question. "Can you help explain my gene and how do we fix it?"
Scientists need money to do research, so Freed launched Milestones for Maxwell fundraising campaign, and a SLC6A1 Connect patient advocacy nonprofit, dedicated to improving the lives of children and families battling this rare condition. And then it became clear that the mutation wasn't as rare as it seemed. As other parents began to discover her nonprofit, the number of known cases rose from 40 to 100, and later to 400, Freed says. "The disease is only rare until it messes with the wrong mother."
It took one mother to find another to start looking into what's happening inside Maxwell's brain. Freed came across Jeanne Paz, a Gladstone Institutes researcher who studies epilepsy with particular interest in absence or silent seizures—those that don't manifest by convulsions, but rather make patients absently stare into space—and that's one type of seizures Maxwell has. "It's like a brief period of silence in the brain during which the person doesn't pay attention to what's happening, and as soon as they come out of the seizure they are back to life," Paz explains. "It's like a pause button on consciousness." She was working to understand the underlying biology.
To understand how seizures begin, spread and stop, Paz uses optogenetics in mice. From words "genetic" and "optikós," which means visible in Greek, the optogenetics technique involves two steps. First, scientists introduce a light-sensitive gene into a specific brain cell type—for example into excitatory neurons that release glutamate, a neurotransmitter, which activates other cells in the brain. Then they implant a very thin optical fiber into the brain area where they forged these light-sensitive neurons. As they shine the light through the optical fiber, researchers can make excitatory neurons to release glutamate—or instead tell them to stop being active and "shut up". The ability to control what these neurons of interest do, quite literally sheds light onto where seizures start, how they propagate and what cells are involved in stopping them.
"Let's say a seizure started and we shine the light that reduces the activity of specific neurons," Paz explains. "If that stops the seizure, we know that activating those cells was necessary to maintain the seizure." Likewise, shutting down their activity will make the seizure stop.
Freed reached out to Paz in 2019 and the two women had an instant connection. They were both passionate about brain and seizures research, even if for different reasons. Freed asked Paz if she would study her son's seizures and Paz agreed.
To do that, Paz needed mice that carried the SLC6A1 mutation, so Freed found a company in China that created them to specs. The company replaced a mouse SLC6A1 gene with a human mutated one and shipped them over to Paz's lab. "We call them Maxwell mice," Paz says, "and we are now implanting electrodes into them to see which brain regions generate seizures." That would help them understand what goes wrong and what brain cells are malfunctioning in the SLC6A1 mice—and help scientists better understand what might cause seizures in children.
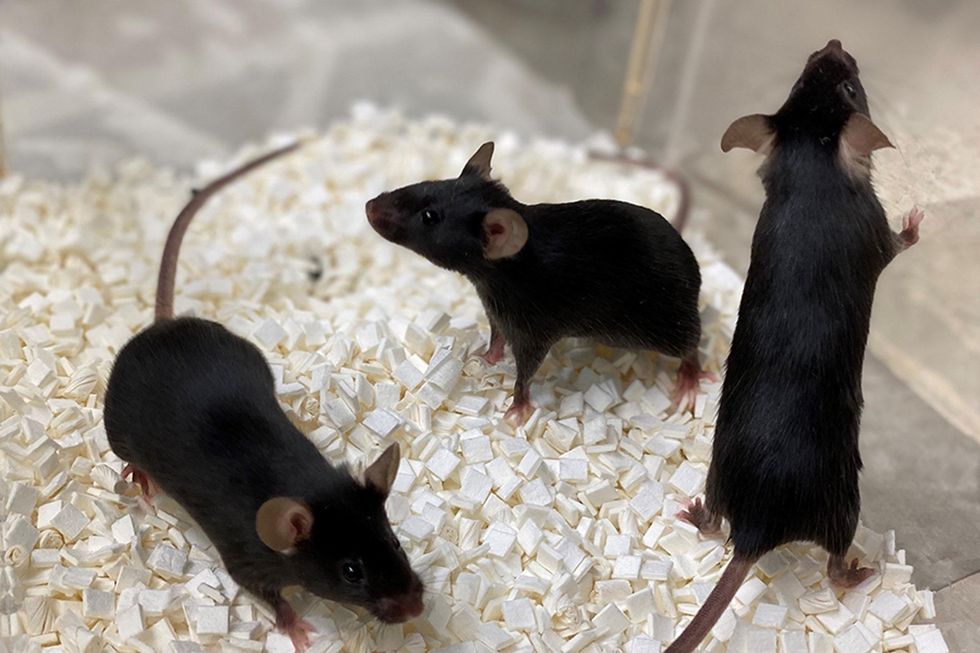
Bred to carry SLC6A1 mutation, these "Maxwell mice" will help better understand this debilitating genetic disease. (These mice are from Vanderbilt University, where researchers are also studying SLC6A1.)
Courtesy Amber Freed
This information—along with other research Amber is funding in other institutions—will inform the development of a novel genetic treatment, in which scientists would deploy a harmless virus to deliver a healthy, working copy of the SLC6A1 gene into the mice brains. They would likely deliver the therapeutic via a spinal tap infusion, and if it works and doesn't produce side effects in mice, the human trials will follow.
In the meantime, Freed is raising money to fund other research of various stop-gap measures. On April 22, 2021, she updated her Milestone for Maxwell page with a post that her nonprofit is funding yet another effort. It is a trial at Weill Cornell Medicine in New York City, in which doctors will use an already FDA-approved drug, which was recently repurposed for the SLC6A1 condition to treat epilepsy in these children. "It will buy us time," Freed says—while the gene therapy effort progresses.
Freed is determined to beat SLC6A1 before it beats down her family. She hopes to put an end to this disease—and similar genetic diseases—once and for all. Her goal is not only to have scientists create a remedy, but also to add the mutation to a newborn screening panel. That way, children born with this condition in the future would receive gene therapy before they even leave the hospital.
"I don't want there to be another Maxwell Freed," she says, "and that's why I am fighting like a mother." The gene therapy trial still might be a few years away, but the Weill Cornell one aims to launch very soon—possibly around Mother's Day. This is yet another milestone for Maxwell, another baby step forward—and the best gift a mother can get.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.
Here's how one doctor overcame extraordinary odds to help create the birth control pill
Dr. Percy Julian had so many personal and professional obstacles throughout his life, it’s amazing he was able to accomplish anything at all. But this hidden figure not only overcame these incredible obstacles, he also laid the foundation for the creation of the birth control pill.
Julian’s first obstacle was growing up in the Jim Crow-era south in the early part of the twentieth century, where racial segregation kept many African-Americans out of schools, libraries, parks, restaurants, and more. Despite limited opportunities and education, Julian was accepted to DePauw University in Indiana, where he majored in chemistry. But in college, Julian encountered another obstacle: he wasn’t allowed to stay in DePauw’s student housing because of segregation. Julian found lodging in an off-campus boarding house that refused to serve him meals. To pay for his room, board, and food, Julian waited tables and fired furnaces while he studied chemistry full-time. Incredibly, he graduated in 1920 as valedictorian of his class.
After graduation, Julian landed a fellowship at Harvard University to study chemistry—but here, Julian ran into yet another obstacle. Harvard thought that white students would resent being taught by Julian, an African-American man, so they withdrew his teaching assistantship. Julian instead decided to complete his PhD at the University of Vienna in Austria. When he did, he became one of the first African Americans to ever receive a PhD in chemistry.
Julian received offers for professorships, fellowships, and jobs throughout the 1930s, due to his impressive qualifications—but these offers were almost always revoked when schools or potential employers found out Julian was black. In one instance, Julian was offered a job at the Institute of Paper Chemistory in Appleton, Wisconsin—but Appleton, like many cities in the United States at the time, was known as a “sundown town,” which meant that black people weren’t allowed to be there after dark. As a result, Julian lost the job.
During this time, Julian became an expert at synthesis, which is the process of turning one substance into another through a series of planned chemical reactions. Julian synthesized a plant compound called physostigmine, which would later become a treatment for an eye disease called glaucoma.
In 1936, Julian was finally able to land—and keep—a job at Glidden, and there he found a way to extract soybean protein. This was used to produce a fire-retardant foam used in fire extinguishers to smother oil and gasoline fires aboard ships and aircraft carriers, and it ended up saving the lives of thousands of soldiers during World War II.
At Glidden, Julian found a way to synthesize human sex hormones such as progesterone, estrogen, and testosterone, from plants. This was a hugely profitable discovery for his company—but it also meant that clinicians now had huge quantities of these hormones, making hormone therapy cheaper and easier to come by. His work also laid the foundation for the creation of hormonal birth control: Without the ability to synthesize these hormones, hormonal birth control would not exist.
Julian left Glidden in the 1950s and formed his own company, called Julian Laboratories, outside of Chicago, where he manufactured steroids and conducted his own research. The company turned profitable within a year, but even so Julian’s obstacles weren’t over. In 1950 and 1951, Julian’s home was firebombed and attacked with dynamite, with his family inside. Julian often had to sit out on the front porch of his home with a shotgun to protect his family from violence.
But despite years of racism and violence, Julian’s story has a happy ending. Julian’s family was eventually welcomed into the neighborhood and protected from future attacks (Julian’s daughter lives there to this day). Julian then became one of the country’s first black millionaires when he sold his company in the 1960s.
When Julian passed away at the age of 76, he had more than 130 chemical patents to his name and left behind a body of work that benefits people to this day.
Therapies for Healthy Aging with Dr. Alexandra Bause
My guest today is Dr. Alexandra Bause, a biologist who has dedicated her career to advancing health, medicine and healthier human lifespans. Dr. Bause co-founded a company called Apollo Health Ventures in 2017. Currently a venture partner at Apollo, she's immersed in the discoveries underway in Apollo’s Venture Lab while the company focuses on assembling a team of investors to support progress. Dr. Bause and Apollo Health Ventures say that biotech is at “an inflection point” and is set to become a driver of important change and economic value.
Previously, Dr. Bause worked at the Boston Consulting Group in its healthcare practice specializing in biopharma strategy, among other priorities
She did her PhD studies at Harvard Medical School focusing on molecular mechanisms that contribute to cellular aging, and she’s also a trained pharmacist
In the episode, we talk about the present and future of therapeutics that could increase people’s spans of health, the benefits of certain lifestyle practice, the best use of electronic wearables for these purposes, and much more.
Dr. Bause is at the forefront of developing interventions that target the aging process with the aim of ensuring that all of us can have healthier, more productive lifespans.


