How Genetic Testing and Targeted Treatments Are Helping More Cancer Patients Survive

Scientists are studying cancer genomes to more precisely diagnose their patients' diseases - offering hope for targeted drug treatments.
Late in 2018, Chris Reiner found himself “chasing a persistent cough” to figure out a cause. He talked to doctors; he endured various tests, including an X-ray. Initially, his physician suspected bronchitis. After several months, he still felt no improvement. In May 2019, his general practitioner recommended that Reiner, a business development specialist for a Seattle-based software company, schedule a CAT scan.
Reiner knew immediately that his doctor asking him to visit his office to discuss the results wasn’t a good sign. The longtime resident of Newburyport, MA, remembers dreading “that conversation that people who learn they have cancer have.”
“The doctor handed me something to look at, and the only thing I remember after that was everything went blank all around me,” Reiner, 50, reveals. “It was the magnitude of what he was telling me, that I had a malignant mass in my lung.”
Next, he recalls, he felt ushered into “the jaws of the medical system very quickly.” He spent a couple of days meeting with a team of doctors at Beth Israel Deaconess Medical Center in nearby Boston. One of them was from a medical field he hadn’t even known existed, a pulmonary interventionist, who would perform a biopsy on the mass in his lung.
“Knowing there was a medicine for my particular type of cancer was like a weight lifted off my shoulders."
A week later he and his wife Allison returned to meet with the oncologist, radiologist, pulmonary interventionist – his medical team. They confirmed his initial diagnosis: Stage 4 metastatic lung cancer that had spread to several parts of his body. “We just sat there, stunned,” he says. “I felt like I was getting hit by a wrecking ball over and over.”
An onslaught of medical terminology about what they had identified flowed over the shocked couple, but then the medical team switched gears, he recalls. They offered hope. “They told me, ‘Hey, you’re not a smoker, so that’s good,’” Reiner says. “‘There’s a good chance that what’s driving this disease for you is actually a genetic mutation, and we have ways to understand more about what that could be through some simple testing.’”
They told him about Foundation Medicine, a company launched in neighboring Cambridge, MA, in 2009 that develops, manufactures, and sells genomic profiling assays. These are tests that, according to the company’s website, “can analyze a broad panel of genes to detect the four main classes of genomic alterations known to drive cancer growth.” With these insights, certain patients can be matched with therapies targeted specifically for the genetic driver(s) of their cancer. The company maintains one of the largest cancer genomic databases in the world, with more than 500,000 patient samples profiled, and they have more than 65 biopharma partners.
According to Foundation Medicine, they are the only company that has FDA-approved tests for both tissue- and blood-based comprehensive genomic profiling tests. One other company has an FDA-approved biopsy test, and several other companies offer tissue-based genomic profiling. Additionally, several major cancer centers like Memorial Sloan Kettering in New York and Anderson Cancer Center in Texas have their own such testing platforms.
Currently, genomic profiling is more accessible for patients with advanced cancer, due to broader insurance coverage in later stages of disease.
“Right now, the vast majority of patients either have cancers for which we don’t have treatments or they have genetic alterations that are not known,” says Jorge Garcia, MD, Division Chief, Solid Tumor Oncology, UH Cleveland Medical Center, which has its own CGP testing platform. “However, a significant proportion of patients with advanced cancer have alterations that we can tap for therapeutic purposes.”
Foundation Medicine estimates that in 2017, just over 5 percent of advanced solid cancer patients in the U.S. received CGP testing. In 2021, they estimate that number is between 25 to 30 percent of advanced solid cancer patients in the U.S., which doesn’t include patients who are tested with small (less than 50 genes) panels. Their panel tests for more than 300 cancer-related genes.

“The good news is the platforms we are developing are better and more comprehensive, and they’re going to continue to be larger data sets,” Dr. Garcia adds.
In Reiner’s case, his team ordered comprehensive genetic profiling on both his tissue and blood, from Foundation Medicine.
At this point, Reiner still wasn’t sure what genetic mutations were or how they factored into cancer or what comprehensive genomic profiling entailed. That day, though, his team ushered the Reiners into the world of precision oncology that placed him on much more sure footing to learn about and fight the specific lung cancer that had been troubling him for more than a year.
What genetic alterations were driving his cancer? Foundation Medicine’s tests were about to find out.
At the core of these tests is next generation sequencing, a DNA sequencing technology. Since 2009, this has revolutionized genomic research, according to the National Center for Biotechnology Information, because it allows an entire human genome to be sequenced within one day. Cancer genomics posits that cancer is caused by mutations and is a disease of the genome. Now, cancer genomes can be systemically studied in their entirety. For cancer patients such as Reiner, NGS can provide a more precise diagnosis and classification of the disease, more accurate prognosis, and potentially the identification of targeted drug treatments. Ultimately, the technology can provide the basis of personalized cancer management.
The detailed reports supply patients and their oncologists with extensive information about the patient’s genomic profile and potential treatment options that they can discuss together. Reiner trusted his doctors that this approach was worth the two- or three-week wait to receive the Foundation Medicine report and the specifically targeted treatment, rather than immediately jump into a round of chemotherapy. He is especially grateful now, he says, because the report delivered a great deal of relief from his previously exhausting and growing anxiety about having cancer.
Reiner and his team learned his lung cancer contained the epidermal growth factor receptor (EGFR) mutation. That biomarker enabled his oncologist to prescribe Tagrisso (osimertinib), a medication developed to directly target that genetic mutation.
“Knowing there was a medicine for my particular type of cancer was like a weight lifted off my shoulders,” he says. “It only took a week or two before my cough finally started subsiding. This pill goes right after the particular piece of genetic material in the tumor that’s causing its growth.”
Dr. Jerry Mitchell, director field medical oncology, Foundation Medicine, in Columbus, Ohio, explains that genomic profiling is generating substantial impacts today. “This is a technology that is the standard of care across many advanced malignancies that takes patients from chemotherapy-only options to very targeted options or immunotherapy options,” he says. “You can also look at complex biomarkers, and these are not specific genetic changes but different genes across the tumor to get a biomarker.”
According to Dr. Mitchell, Foundation Medicine’s technology can test more than 324 different cancer-related genes in a single test. Thus, a growing number of patients are benefitting from comprehensive genetic profiling, due to the rapidly growing number of targeted therapies. While not all of the cancers are treatable yet, the company uses that information to partner with researchers to find new potential therapies for patient groups that may have rare mutations.
Since his tumor’s diagnosis, Reiner has undergone chemotherapy and a couple surgeries to treat the metastatic cancer in other parts of his body, but the drug Tagrisso has significantly reduced his lung tumor. Now, having learned so much during the past couple of years, he is grateful for precision oncology. He still reflects on the probability that, had the Tagrisso pill not been available in May 2019, he might have only survived for another six months or a year.
“Comprehensive Genomic Profiling is not some future state, but in both the U.S. and Europe, it is a very standard, accepted, and recommended first step to knowing how to treat your cancer,” says Dr. Mitchell, adding that he feels fortunate to be an oncologist in this era. “However, we know there are still people not getting this recommended testing, so we still have opportunities to find many more patients and impact them by knowing the molecular profile of their cancer.”
A robot server, controlled remotely by a disabled worker, delivers drinks to patrons at the DAWN cafe in Tokyo.
A sleek, four-foot tall white robot glides across a cafe storefront in Tokyo’s Nihonbashi district, holding a two-tiered serving tray full of tea sandwiches and pastries. The cafe’s patrons smile and say thanks as they take the tray—but it’s not the robot they’re thanking. Instead, the patrons are talking to the person controlling the robot—a restaurant employee who operates the avatar from the comfort of their home.
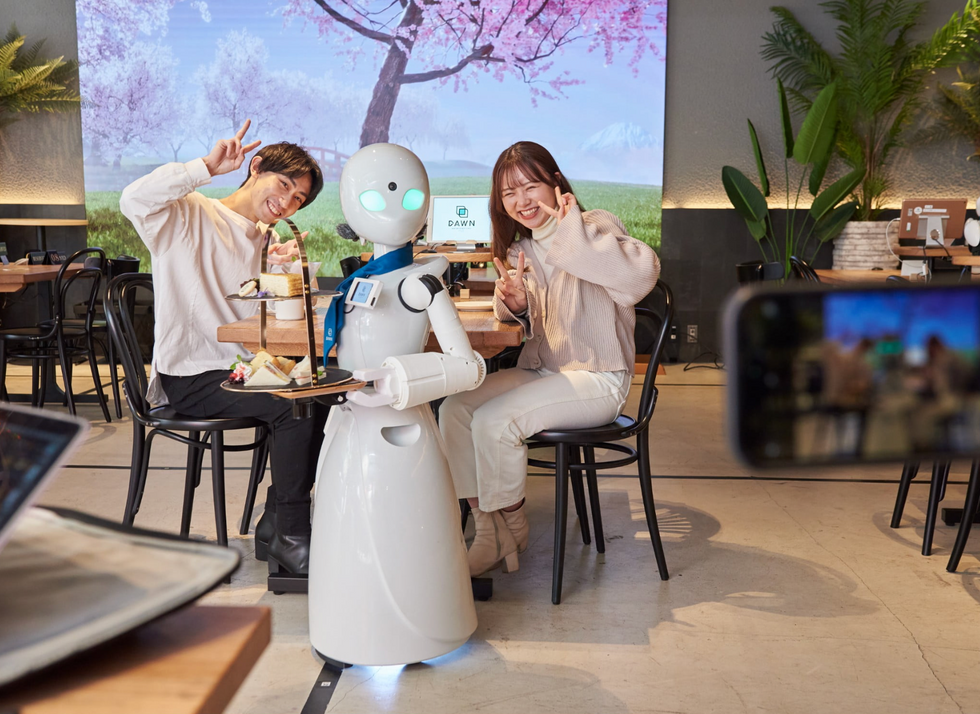
It’s a typical scene at DAWN, short for Diverse Avatar Working Network—a cafe that launched in Tokyo six years ago as an experimental pop-up and quickly became an overnight success. Today, the cafe is a permanent fixture in Nihonbashi, staffing roughly 60 remote workers who control the robots remotely and communicate to customers via a built-in microphone.
More than just a creative idea, however, DAWN is being hailed as a life-changing opportunity. The workers who control the robots remotely (known as “pilots”) all have disabilities that limit their ability to move around freely and travel outside their homes. Worldwide, an estimated 16 percent of the global population lives with a significant disability—and according to the World Health Organization, these disabilities give rise to other problems, such as exclusion from education, unemployment, and poverty.
These are all problems that Kentaro Yoshifuji, founder and CEO of Ory Laboratory, which supplies the robot servers at DAWN, is looking to correct. Yoshifuji, who was bedridden for several years in high school due to an undisclosed health problem, launched the company to help enable people who are house-bound or bedridden to more fully participate in society, as well as end the loneliness, isolation, and feelings of worthlessness that can sometimes go hand-in-hand with being disabled.
“It’s heartbreaking to think that [people with disabilities] feel they are a burden to society, or that they fear their families suffer by caring for them,” said Yoshifuji in an interview in 2020. “We are dedicating ourselves to providing workable, technology-based solutions. That is our purpose.”

Shota, Kuwahara, a DAWN employee with muscular dystrophy, agrees. "There are many difficulties in my daily life, but I believe my life has a purpose and is not being wasted," he says. "Being useful, able to help other people, even feeling needed by others, is so motivational."
A woman receives a mammogram, which can detect the presence of tumors in a patient's breast.
When a patient is diagnosed with early-stage breast cancer, having surgery to remove the tumor is considered the standard of care. But what happens when a patient can’t have surgery?
Whether it’s due to high blood pressure, advanced age, heart issues, or other reasons, some breast cancer patients don’t qualify for a lumpectomy—one of the most common treatment options for early-stage breast cancer. A lumpectomy surgically removes the tumor while keeping the patient’s breast intact, while a mastectomy removes the entire breast and nearby lymph nodes.
Fortunately, a new technique called cryoablation is now available for breast cancer patients who either aren’t candidates for surgery or don’t feel comfortable undergoing a surgical procedure. With cryoablation, doctors use an ultrasound or CT scan to locate any tumors inside the patient’s breast. They then insert small, needle-like probes into the patient's breast which create an “ice ball” that surrounds the tumor and kills the cancer cells.
Cryoablation has been used for decades to treat cancers of the kidneys and liver—but only in the past few years have doctors been able to use the procedure to treat breast cancer patients. And while clinical trials have shown that cryoablation works for tumors smaller than 1.5 centimeters, a recent clinical trial at Memorial Sloan Kettering Cancer Center in New York has shown that it can work for larger tumors, too.
In this study, doctors performed cryoablation on patients whose tumors were, on average, 2.5 centimeters. The cryoablation procedure lasted for about 30 minutes, and patients were able to go home on the same day following treatment. Doctors then followed up with the patients after 16 months. In the follow-up, doctors found the recurrence rate for tumors after using cryoablation was only 10 percent.
For patients who don’t qualify for surgery, radiation and hormonal therapy is typically used to treat tumors. However, said Yolanda Brice, M.D., an interventional radiologist at Memorial Sloan Kettering Cancer Center, “when treated with only radiation and hormonal therapy, the tumors will eventually return.” Cryotherapy, Brice said, could be a more effective way to treat cancer for patients who can’t have surgery.
“The fact that we only saw a 10 percent recurrence rate in our study is incredibly promising,” she said.

