Genetic Testing Companies Are Facing a Racial Bias Problem in Disease Risk Tests

The large genetic studies underlying certain disease risk tests have primarily been done in populations of European ancestry, limiting their accuracy.
Earlier this year, California-based Ambry Genetics announced that it was discontinuing a test meant to estimate a person's risk of developing prostate or breast cancer. The test looks for variations in a person's DNA that are known to be associated with these cancers.
Known as a polygenic risk score, this type of test adds up the effects of variants in many genes — often in the dozens or hundreds — and calculates a person's risk of developing a particular health condition compared to other people. In this way, polygenic risk scores are different from traditional genetic tests that look for mutations in single genes, such as BRCA1 and BRCA2, which raise the risk of breast cancer.
Traditional genetic tests look for mutations that are relatively rare in the general population but have a large impact on a person's disease risk, like BRCA1 and BRCA2. By contrast, polygenic risk scores scan for more common genetic variants that, on their own, have a small effect on risk. Added together, however, they can raise a person's risk for developing disease.
These scores could become a part of routine healthcare in the next few years. Researchers are developing polygenic risk scores for cancer, heart, disease, diabetes and even depression. Before they can be rolled out widely, they'll have to overcome a key limitation: racial bias.
"The issue with these polygenic risk scores is that the scientific studies which they're based on have primarily been done in individuals of European ancestry," says Sara Riordan, president of the National Society of Genetics Counselors. These scores are calculated by comparing the genetic data of people with and without a particular disease. To make these scores accurate, researchers need genetic data from tens or hundreds of thousands of people.
Myriad's old test would have shown that a Black woman had twice as high of a risk for breast cancer compared to the average woman even if she was at low or average risk.
A 2018 analysis found that 78% of participants included in such large genetic studies, known as genome-wide association studies, were of European descent. That's a problem, because certain disease-associated genetic variants don't appear equally across different racial and ethnic groups. For example, a particular variant in the TTR gene, known as V1221, occurs more frequently in people of African descent. In recent years, the variant has been found in 3 to 4 percent of individuals of African ancestry in the United States. Mutations in this gene can cause protein to build up in the heart, leading to a higher risk of heart failure. A polygenic risk score for heart disease based on genetic data from mostly white people likely wouldn't give accurate risk information to African Americans.
Accuracy in genetic testing matters because such polygenic risk scores could help patients and their doctors make better decisions about their healthcare.
For instance, if a polygenic risk score determines that a woman is at higher-than-average risk of breast cancer, her doctor might recommend more frequent mammograms — X-rays that take a picture of the breast. Or, if a risk score reveals that a patient is more predisposed to heart attack, a doctor might prescribe preventive statins, a type of cholesterol-lowering drug.
"Let's be clear, these are not diagnostic tools," says Alicia Martin, a population and statistical geneticist at the Broad Institute of MIT and Harvard. "We can't use a polygenic score to say you will or will not get breast cancer or have a heart attack."
But combining a patient's polygenic risk score with other factors that affect disease risk — like age, weight, medication use or smoking status — may provide a better sense of how likely they are to develop a specific health condition than considering any one risk factor one its own. The accuracy of polygenic risk scores becomes even more important when considering that these scores may be used to guide medication prescription or help patients make decisions about preventive surgery, such as a mastectomy.
In a study published in September, researchers used results from large genetics studies of people with European ancestry and data from the UK Biobank to calculate polygenic risk scores for breast and prostate cancer for people with African, East Asian, European and South Asian ancestry. They found that they could identify individuals at higher risk of breast and prostate cancer when they scaled the risk scores within each group, but the authors say this is only a temporary solution. Recruiting more diverse participants for genetics studies will lead to better cancer detection and prevent, they conclude.
Recent efforts to do just that are expected to make these scores more accurate in the future. Until then, some genetics companies are struggling to overcome the European bias in their tests.
Acknowledging the limitations of its polygenic risk score, Ambry Genetics said in April that it would stop offering the test until it could be recalibrated. The company launched the test, known as AmbryScore, in 2018.
"After careful consideration, we have decided to discontinue AmbryScore to help reduce disparities in access to genetic testing and to stay aligned with current guidelines," the company said in an email to customers. "Due to limited data across ethnic populations, most polygenic risk scores, including AmbryScore, have not been validated for use in patients of diverse backgrounds." (The company did not make a spokesperson available for an interview for this story.)
In September 2020, the National Comprehensive Cancer Network updated its guidelines to advise against the use of polygenic risk scores in routine patient care because of "significant limitations in interpretation." The nonprofit, which represents 31 major cancer cancers across the United States, said such scores could continue to be used experimentally in clinical trials, however.
Holly Pederson, director of Medical Breast Services at the Cleveland Clinic, says the realization that polygenic risk scores may not be accurate for all races and ethnicities is relatively recent. Pederson worked with Salt Lake City-based Myriad Genetics, a leading provider of genetic tests, to improve the accuracy of its polygenic risk score for breast cancer.
The company announced in August that it had recalibrated the test, called RiskScore, for women of all ancestries. Previously, Myriad did not offer its polygenic risk score to women who self-reported any ancestry other than sole European or Ashkenazi ancestry.
"Black women, while they have a similar rate of breast cancer to white women, if not lower, had twice as high of a polygenic risk score because the development and validation of the model was done in white populations," Pederson said of the old test. In other words, Myriad's old test would have shown that a Black woman had twice as high of a risk for breast cancer compared to the average woman even if she was at low or average risk.
To develop and validate the new score, Pederson and other researchers assessed data from more than 275,000 women, including more than 31,000 African American women and nearly 50,000 women of East Asian descent. They looked at 56 different genetic variants associated with ancestry and 93 associated with breast cancer. Interestingly, they found that at least 95% of the breast cancer variants were similar amongst the different ancestries.
The company says the resulting test is now more accurate for all women across the board, but Pederson cautions that it's still slightly less accurate for Black women.
"It's not only the lack of data from Black women that leads to inaccuracies and a lack of validation in these types of risk models, it's also the pure genomic diversity of Africa," she says, noting that Africa is the most genetically diverse continent on the planet. "We just need more data, not only in American Black women but in African women to really further characterize that continent."
Martin says it's problematic that such scores are most accurate for white people because they could further exacerbate health disparities in traditionally underserved groups, such as Black Americans. "If we were to set up really representative massive genetic studies, we would do a much better job at predicting genetic risk for everybody," she says.
Earlier this year, the National Institutes of Health awarded $38 million to researchers to improve the accuracy of polygenic risk scores in diverse populations. Researchers will create new genome datasets and pool information from existing ones in an effort to diversify the data that polygenic scores rely on. They plan to make these datasets available to other scientists to use.
"By having adequate representation, we can ensure that the results of a genetic test are widely applicable," Riordan says.
Thanks to safety cautions from the COVID-19 pandemic, a strain of influenza has been completely eliminated.
If you were one of the millions who masked up, washed your hands thoroughly and socially distanced, pat yourself on the back—you may have helped change the course of human history.
Scientists say that thanks to these safety precautions, which were introduced in early 2020 as a way to stop transmission of the novel COVID-19 virus, a strain of influenza has been completely eliminated. This marks the first time in human history that a virus has been wiped out through non-pharmaceutical interventions, such as vaccines.
The flu shot, explained
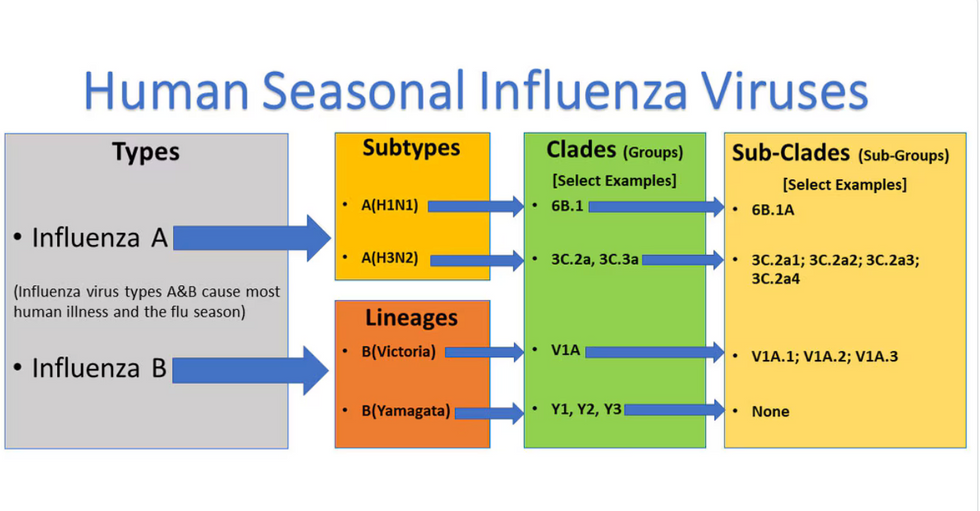
Influenza viruses type A and B are responsible for the majority of human illnesses and the flu season.
Centers for Disease Control
For more than a decade, flu shots have protected against two types of the influenza virus–type A and type B. While there are four different strains of influenza in existence (A, B, C, and D), only strains A, B, and C are capable of infecting humans, and only A and B cause pandemics. In other words, if you catch the flu during flu season, you’re most likely sick with flu type A or B.
Flu vaccines contain inactivated—or dead—influenza virus. These inactivated viruses can’t cause sickness in humans, but when administered as part of a vaccine, they teach a person’s immune system to recognize and kill those viruses when they’re encountered in the wild.
Each spring, a panel of experts gives a recommendation to the US Food and Drug Administration on which strains of each flu type to include in that year’s flu vaccine, depending on what surveillance data says is circulating and what they believe is likely to cause the most illness during the upcoming flu season. For the past decade, Americans have had access to vaccines that provide protection against two strains of influenza A and two lineages of influenza B, known as the Victoria lineage and the Yamagata lineage. But this year, the seasonal flu shot won’t include the Yamagata strain, because the Yamagata strain is no longer circulating among humans.
How Yamagata Disappeared

Flu surveillance data from the Global Initiative on Sharing All Influenza Data (GISAID) shows that the Yamagata lineage of flu type B has not been sequenced since April 2020.
Nature
Experts believe that the Yamagata lineage had already been in decline before the pandemic hit, likely because the strain was naturally less capable of infecting large numbers of people compared to the other strains. When the COVID-19 pandemic hit, the resulting safety precautions such as social distancing, isolating, hand-washing, and masking were enough to drive the virus into extinction completely.
Because the strain hasn’t been circulating since 2020, the FDA elected to remove the Yamagata strain from the seasonal flu vaccine. This will mark the first time since 2012 that the annual flu shot will be trivalent (three-component) rather than quadrivalent (four-component).
Should I still get the flu shot?
The flu shot will protect against fewer strains this year—but that doesn’t mean we should skip it. Influenza places a substantial health burden on the United States every year, responsible for hundreds of thousands of hospitalizations and tens of thousands of deaths. The flu shot has been shown to prevent millions of illnesses each year (more than six million during the 2022-2023 season). And while it’s still possible to catch the flu after getting the flu shot, studies show that people are far less likely to be hospitalized or die when they’re vaccinated.
Another unexpected benefit of dropping the Yamagata strain from the seasonal vaccine? This will possibly make production of the flu vaccine faster, and enable manufacturers to make more vaccines, helping countries who have a flu vaccine shortage and potentially saving millions more lives.
After his grandmother’s dementia diagnosis, one man invented a snack to keep her healthy and hydrated.
Founder Lewis Hornby and his grandmother Pat, sampling Jelly Drops—an edible gummy containing water and life-saving electrolytes.
On a visit to his grandmother’s nursing home in 2016, college student Lewis Hornby made a shocking discovery: Dehydration is a common (and dangerous) problem among seniors—especially those that are diagnosed with dementia.
Hornby’s grandmother, Pat, had always had difficulty keeping up her water intake as she got older, a common issue with seniors. As we age, our body composition changes, and we naturally hold less water than younger adults or children, so it’s easier to become dehydrated quickly if those fluids aren’t replenished. What’s more, our thirst signals diminish naturally as we age as well—meaning our body is not as good as it once was in letting us know that we need to rehydrate. This often creates a perfect storm that commonly leads to dehydration. In Pat’s case, her dehydration was so severe she nearly died.
When Lewis Hornby visited his grandmother at her nursing home afterward, he learned that dehydration especially affects people with dementia, as they often don’t feel thirst cues at all, or may not recognize how to use cups correctly. But while dementia patients often don’t remember to drink water, it seemed to Hornby that they had less problem remembering to eat, particularly candy.

Hornby wanted to create a solution for elderly people who struggled keeping their fluid intake up. He spent the next eighteen months researching and designing a solution and securing funding for his project. In 2019, Hornby won a sizable grant from the Alzheimer’s Society, a UK-based care and research charity for people with dementia and their caregivers. Together, through the charity’s Accelerator Program, they created a bite-sized, sugar-free, edible jelly drop that looked and tasted like candy. The candy, called Jelly Drops, contained 95% water and electrolytes—important minerals that are often lost during dehydration. The final product launched in 2020—and was an immediate success. The drops were able to provide extra hydration to the elderly, as well as help keep dementia patients safe, since dehydration commonly leads to confusion, hospitalization, and sometimes even death.
Not only did Jelly Drops quickly become a favorite snack among dementia patients in the UK, but they were able to provide an additional boost of hydration to hospital workers during the pandemic. In NHS coronavirus hospital wards, patients infected with the virus were regularly given Jelly Drops to keep their fluid levels normal—and staff members snacked on them as well, since long shifts and personal protective equipment (PPE) they were required to wear often left them feeling parched.
In April 2022, Jelly Drops launched in the United States. The company continues to donate 1% of its profits to help fund Alzheimer’s research.

