Genital Transplants: Is Science Going Too Far, Too Fast?

Medical staff rushing organs to a surgery for transplantation.
Thanks to the remarkable evolution of organ transplantation, it's now possible to replace genitals that don't work properly or have been injured. Surgeons have been transplanting ovarian tissue for more than a decade, and they're now successfully transplanting penises and wombs too.
Rules and regulations aren't keeping up with the rapid rise of genital transplants.
Earlier this year, an American soldier whose genitals were injured by a bomb in Afghanistan received the first-ever transplant of a penis and scrotum at Johns Hopkins Medicine.
Rules and regulations aren't keeping up with the rapid rise of genital transplants, however, and there's no consensus about how society should handle a long list of difficult and delicate questions.
Are these expensive transplants worth the risk when other alternatives exist? Should men, famously obsessed with their penises, be able to ask for a better model simply because they want one? And what happens when transplant technology further muddles the concept of biological parenthood?
"We need to remember that the human body is not a machine with interchangeable parts," says bioethicist Craig M. Klugman of DePaul University. "These are complicated, difficult and potentially dangerous surgeries. And they require deep consideration on a physical, psychological, spiritual, and financial level."
From Extra Testicles to Replacement Penises
Tinkering with human genitalia -- especially the male variety -- is hardly a new phenomenon. A French surgeon created artificial penises for injured soldiers in the 16th century. And a bizarre implant craze swept the U.S. in the 1930s when a quack physician convinced men that, quite literally, the more testicles the merrier – and if the human variety wasn't available, then ones from goats would have to do.
Now we're more sophisticated. Modern genital transplants are designed to do two things: Treat infertility (in women) and restore the appearance and function of genitals (in men).
In women, surgeons have successfully transplanted ovarian tissue from one woman to another since the mid-2000s, when an Alabama woman gave birth after getting a transplant from her identical twin sister. Last year, for the first time in the U.S., a young woman gave birth after getting a uterus transplant from a living donor.
"Where do you draw the line? Is pregnancy a privilege? Is it a right?"
As for men, surgeons in the U.S. and South Africa have successfully transplanted penises from dead men into four men whose genitals were injured by a botched circumcision, penile cancer or a wartime injury. One man reportedly fathered a child after the procedure.
The Johns Hopkins procedure was the first to include a scrotum. Testicles, however, were not transplanted due to ethical concerns. Surgeons have successfully transplanted testicles from man-to-man in the past, but this procedure isn't performed because the testes would produce sperm with the donor's DNA. As a result, the recipient could father a baby who is genetically related to the donor.
Are Transplants Worth the Expense and Risk?
Genital transplants are not simple procedures. They're extremely expensive, with a uterus transplant estimated to cost as much as $250,000. They're dangerous, since patients typically must take powerful drugs to keep their immune systems from rejecting their new organs. And they're not medically necessary. All have alternatives that are much less risky and costly.
Dr. Hiten D. Patel, a urologist at Johns Hopkins University, believes these types of factors make penis transplants unnecessary. As he wrote in a 2018 commentary in the journal European Urology, "What in the world are we doing?"
There are similar questions about female genital transplants, which allow infertile women to become pregnant instead of turning to alternatives like adoption or surrogacy. "This is not a life-saving transplant. A woman can very well live without a uterus," says McGill University's Dr. Jacques Balayla, who studies uterine transplantation. "Where do you draw the line? Is pregnancy a privilege? Is it a right? You don't want to cause harm to an individual unless there's an absolute need for the procedure."
But Johns Hopkins urologist Dr. Arthur L. Burnett II, who served on the surgical team that performed the penis-and-scrotum procedure, says penis transplants can be appropriate when other alternatives – like a "neophallus" created from forearm skin and tissue – aren't feasible.
It's also important to "restore normalcy," he says. "We want someone to be able to have sense of male adequacy and a normal sense of bodily well-being on both physical and psychological levels."

Surgical team members who performed the penis transplant, including W. P. Andrew Lee, director of the department of plastic and reconstructive surgery, center.
As for the anonymous recipient, he's reportedly doing "very well" five months after the transplant. An update on Johns Hopkins' website states that "he has normal urinary functions and is beginning to regain sensation in the transplanted tissues."
When the Organ Donors Do It Live
Some peculiar messages reached Burnett's desk after his institution announced it would begin performing penis transplants. Several men wanted to donate their own organs. But for now, transplanted penises are only coming from dead donors whose next of kin have approved the donation.
Burnett doesn't expect live donors to enter the penis transplant picture. But there are no guidelines or policies to stop surgeons from transplanting a penis from a live donor or, for that matter, a testicle.
Live women have already donated wombs and ovarian tissue, forcing them to face their own risks from transplant surgery. "You're putting the donor at risk because she has to undergo pretty expensive surgery for a procedure that is not technically lifesaving," McGill University's Balayla says.
When it comes to uterus transplants, the risk spreads even beyond donor and recipient. Balayla notes there's a third person in the equation: The fetus. "Immunosuppressant medication may harm the baby, and you're feeding the baby with a [uterine] blood vessel that's not natural, held together by stitches," he says.
It's up to each medical institution that performs the procedures to set its own policies.
Bioethicists are talking about other issues raised by genital transplants: How should operations for transgender people fit in? Should men be able to get penis transplants for purely cosmetic reasons? And then there's the looming question of genetic parenthood.
It's up to each medical institution that performs the procedures to set its own policies.
Let's say a woman gets a transplant of ovarian tissue, a man gets a testicle transplant, and they have a baby the old-fashioned way.* The child would be genetically linked to the donors, not the parents who conceived him or her.
Call this a full-employment act not just for bioethicists but theologians too. "Catholicism is generally against reproductive technologies because it removes God from the nature of the procreative act. This technology, though, could result in conception through the natural act. Would their concern remain?" DePaul University's Klugman asked. "Judaism is concerned with knowing a child's parentage, would a child from transplanted testes be the child of the donor or the recipient? Would an act of coitus with a transplanted penis be adultery?"
Yikes. Maybe it's time for the medical field or the law to step in to determine what genital transplants surgeons can and can't -- or shouldn't -- do.
So far, however, only uterus transplants have guidelines in place. Otherwise, it's up to each medical institution that performs the procedures to set its own policies.
"I don't know if the medical establishment is in the position to do the best job of self-regulation," says Lisa Campo-Engelstein, a bioethicist with Albany Medical College. "Reproductive medicine in this country is a huge for-profit industry. There's a possibility of exploitation if we leave this to for-profit fertility companies."
And, as bioethicist Klugman notes, guidelines "aren't laws, and people can and do violate them with no effect."
He doesn't think laws are the solution to the ethical issues raised by genital transplants either. Still, he says, "we do need a national conversation on these topics to help provide guidance for doctors and patients."
[Correction: The following sentence has been updated: "Let's say a woman gets a transplant of ovarian tissue, a man gets a testicle transplant, and they have a baby the old-fashioned way." The original sentence mistakenly read "uterus transplant" instead of "ovarian tissue."]
A robot server, controlled remotely by a disabled worker, delivers drinks to patrons at the DAWN cafe in Tokyo.
A sleek, four-foot tall white robot glides across a cafe storefront in Tokyo’s Nihonbashi district, holding a two-tiered serving tray full of tea sandwiches and pastries. The cafe’s patrons smile and say thanks as they take the tray—but it’s not the robot they’re thanking. Instead, the patrons are talking to the person controlling the robot—a restaurant employee who operates the avatar from the comfort of their home.
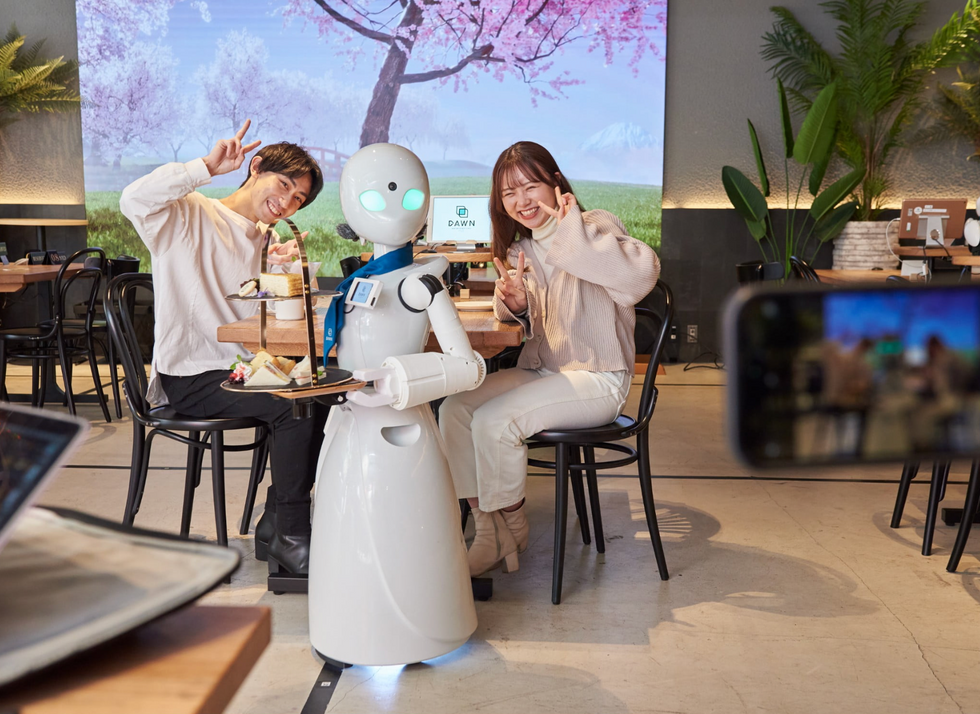
It’s a typical scene at DAWN, short for Diverse Avatar Working Network—a cafe that launched in Tokyo six years ago as an experimental pop-up and quickly became an overnight success. Today, the cafe is a permanent fixture in Nihonbashi, staffing roughly 60 remote workers who control the robots remotely and communicate to customers via a built-in microphone.
More than just a creative idea, however, DAWN is being hailed as a life-changing opportunity. The workers who control the robots remotely (known as “pilots”) all have disabilities that limit their ability to move around freely and travel outside their homes. Worldwide, an estimated 16 percent of the global population lives with a significant disability—and according to the World Health Organization, these disabilities give rise to other problems, such as exclusion from education, unemployment, and poverty.
These are all problems that Kentaro Yoshifuji, founder and CEO of Ory Laboratory, which supplies the robot servers at DAWN, is looking to correct. Yoshifuji, who was bedridden for several years in high school due to an undisclosed health problem, launched the company to help enable people who are house-bound or bedridden to more fully participate in society, as well as end the loneliness, isolation, and feelings of worthlessness that can sometimes go hand-in-hand with being disabled.
“It’s heartbreaking to think that [people with disabilities] feel they are a burden to society, or that they fear their families suffer by caring for them,” said Yoshifuji in an interview in 2020. “We are dedicating ourselves to providing workable, technology-based solutions. That is our purpose.”

Shota, Kuwahara, a DAWN employee with muscular dystrophy, agrees. "There are many difficulties in my daily life, but I believe my life has a purpose and is not being wasted," he says. "Being useful, able to help other people, even feeling needed by others, is so motivational."
A woman receives a mammogram, which can detect the presence of tumors in a patient's breast.
When a patient is diagnosed with early-stage breast cancer, having surgery to remove the tumor is considered the standard of care. But what happens when a patient can’t have surgery?
Whether it’s due to high blood pressure, advanced age, heart issues, or other reasons, some breast cancer patients don’t qualify for a lumpectomy—one of the most common treatment options for early-stage breast cancer. A lumpectomy surgically removes the tumor while keeping the patient’s breast intact, while a mastectomy removes the entire breast and nearby lymph nodes.
Fortunately, a new technique called cryoablation is now available for breast cancer patients who either aren’t candidates for surgery or don’t feel comfortable undergoing a surgical procedure. With cryoablation, doctors use an ultrasound or CT scan to locate any tumors inside the patient’s breast. They then insert small, needle-like probes into the patient's breast which create an “ice ball” that surrounds the tumor and kills the cancer cells.
Cryoablation has been used for decades to treat cancers of the kidneys and liver—but only in the past few years have doctors been able to use the procedure to treat breast cancer patients. And while clinical trials have shown that cryoablation works for tumors smaller than 1.5 centimeters, a recent clinical trial at Memorial Sloan Kettering Cancer Center in New York has shown that it can work for larger tumors, too.
In this study, doctors performed cryoablation on patients whose tumors were, on average, 2.5 centimeters. The cryoablation procedure lasted for about 30 minutes, and patients were able to go home on the same day following treatment. Doctors then followed up with the patients after 16 months. In the follow-up, doctors found the recurrence rate for tumors after using cryoablation was only 10 percent.
For patients who don’t qualify for surgery, radiation and hormonal therapy is typically used to treat tumors. However, said Yolanda Brice, M.D., an interventional radiologist at Memorial Sloan Kettering Cancer Center, “when treated with only radiation and hormonal therapy, the tumors will eventually return.” Cryotherapy, Brice said, could be a more effective way to treat cancer for patients who can’t have surgery.
“The fact that we only saw a 10 percent recurrence rate in our study is incredibly promising,” she said.

