How Smallpox Was Wiped Off the Planet By a Vaccine and Global Cooperation
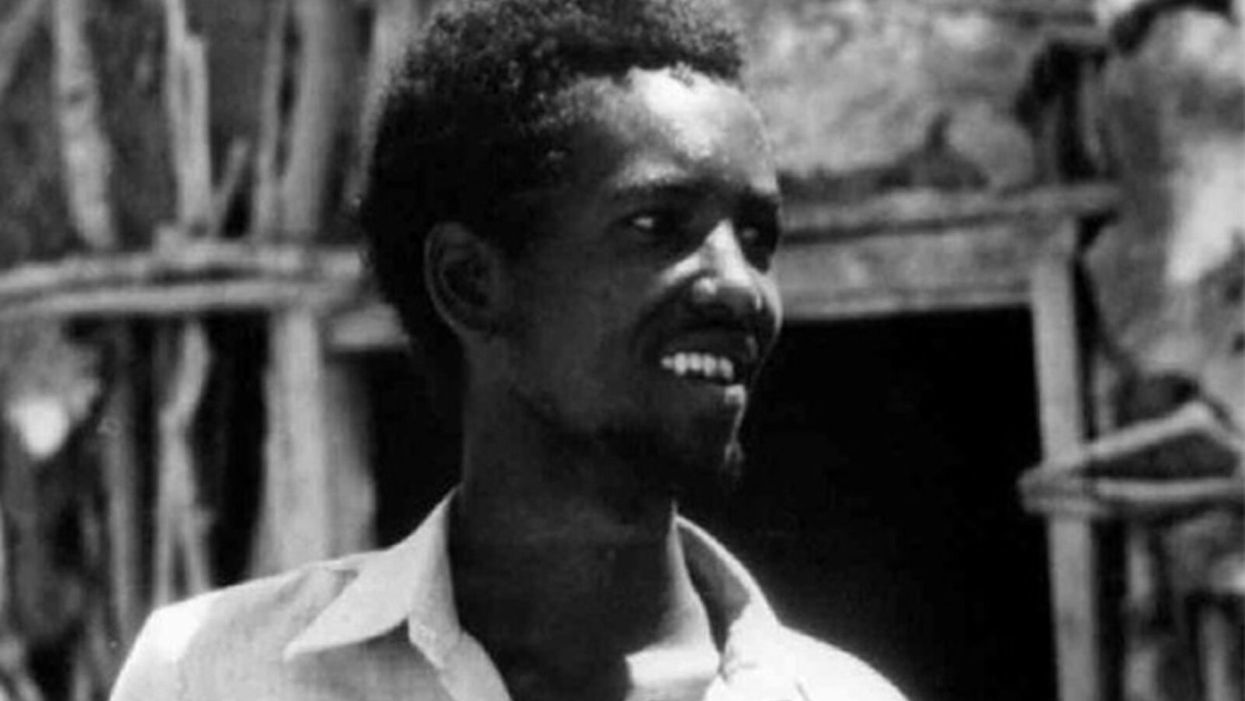
The world's last recorded case of endemic smallpox was in Ali Maow Maalin, of Merka, Somalia, in October 1977. He made a full recovery.
For 3000 years, civilizations all over the world were brutalized by smallpox, an infectious and deadly virus characterized by fever and a rash of painful, oozing sores.
Doctors had to contend with wars, floods, and language barriers to make their campaign a success.
Smallpox was merciless, killing one third of people it infected and leaving many survivors permanently pockmarked and blind. Although smallpox was more common during the 18th and 19th centuries, it was still a leading cause of death even up until the early 1950s, killing an estimated 50 million people annually.
A Primitive Cure
Sometime during the 10th century, Chinese physicians figured out that exposing people to a tiny bit of smallpox would sometimes result in a milder infection and immunity to the disease afterward (if the person survived). Desperate for a cure, people would huff powders made of smallpox scabs or insert smallpox pus into their skin, all in the hopes of getting immunity without having to get too sick. However, this method – called inoculation – didn't always work. People could still catch the full-blown disease, spread it to others, or even catch another infectious disease like syphilis in the process.
A Breakthrough Treatment
For centuries, inoculation – however imperfect – was the only protection the world had against smallpox. But in the late 18th century, an English physician named Edward Jenner created a more effective method. Jenner discovered that inoculating a person with cowpox – a much milder relative of the smallpox virus – would make that person immune to smallpox as well, but this time without the possibility of actually catching or transmitting smallpox. His breakthrough became the world's first vaccine against a contagious disease. Other researchers, like Louis Pasteur, would use these same principles to make vaccines for global killers like anthrax and rabies. Vaccination was considered a miracle, conferring all of the rewards of having gotten sick (immunity) without the risk of death or blindness.
Scaling the Cure
As vaccination became more widespread, the number of global smallpox deaths began to drop, particularly in Europe and the United States. But even as late as 1967, smallpox was still killing anywhere from 10 to 15 million people in poorer parts of the globe. The World Health Assembly (a decision-making body of the World Health Organization) decided that year to launch the first coordinated effort to eradicate smallpox from the planet completely, aiming for 80 percent vaccine coverage in every country in which the disease was endemic – a total of 33 countries.
But officials knew that eradicating smallpox would be easier said than done. Doctors had to contend with wars, floods, and language barriers to make their campaign a success. The vaccination initiative in Bangladesh proved the most challenging, due to its population density and the prevalence of the disease, writes journalist Laurie Garrett in her book, The Coming Plague.
In one instance, French physician Daniel Tarantola on assignment in Bangladesh confronted a murderous gang that was thought to be spreading smallpox throughout the countryside during their crime sprees. Without police protection, Tarantola confronted the gang and "faced down guns" in order to immunize them, protecting the villagers from repeated outbreaks.
Because not enough vaccines existed to vaccinate everyone in a given country, doctors utilized a strategy called "ring vaccination," which meant locating individual outbreaks and vaccinating all known and possible contacts to stop an outbreak at its source. Fewer than 50 percent of the population in Nigeria received a vaccine, for example, but thanks to ring vaccination, it was eradicated in that country nonetheless. Doctors worked tirelessly for the next eleven years to immunize as many people as possible.
The World Health Organization declared smallpox officially eradicated on May 8, 1980.
A Resounding Success
In November 1975, officials discovered a case of variola major — the more virulent strain of the smallpox virus — in a three-year-old Bangladeshi girl named Rahima Banu. Banu was forcibly quarantined in her family's home with armed guards until the risk of transmission had passed, while officials went door-to-door vaccinating everyone within a five-mile radius. Two years later, the last case of variola major in human history was reported in Somalia. When no new community-acquired cases appeared after that, the World Health Organization declared smallpox officially eradicated on May 8, 1980.
Because of smallpox, we now know it's possible to completely eliminate a disease. But is it likely to happen again with other diseases, like COVID-19? Some scientists aren't so sure. As dangerous as smallpox was, it had a few characteristics that made eradication possibly easier than for other diseases. Smallpox, for instance, has no animal reservoir, meaning that it could not circulate in animals and resurge in a human population at a later date. Additionally, a person who had smallpox once was guaranteed immunity from the disease thereafter — which is not the case for COVID-19.
In The Coming Plague, Japanese physician Isao Arita, who led the WHO's Smallpox Eradication Unit, admitted to routinely defying orders from the WHO, mobilizing to parts of the world without official approval and sometimes even vaccinating people against their will. "If we hadn't broken every single WHO rule many times over, we would have never defeated smallpox," Arita said. "Never."
Still, thanks to the life-saving technology of vaccines – and the tireless efforts of doctors and scientists across the globe – a once-lethal disease is now a thing of the past.
Here's how one doctor overcame extraordinary odds to help create the birth control pill
Dr. Percy Julian had so many personal and professional obstacles throughout his life, it’s amazing he was able to accomplish anything at all. But this hidden figure not only overcame these incredible obstacles, he also laid the foundation for the creation of the birth control pill.
Julian’s first obstacle was growing up in the Jim Crow-era south in the early part of the twentieth century, where racial segregation kept many African-Americans out of schools, libraries, parks, restaurants, and more. Despite limited opportunities and education, Julian was accepted to DePauw University in Indiana, where he majored in chemistry. But in college, Julian encountered another obstacle: he wasn’t allowed to stay in DePauw’s student housing because of segregation. Julian found lodging in an off-campus boarding house that refused to serve him meals. To pay for his room, board, and food, Julian waited tables and fired furnaces while he studied chemistry full-time. Incredibly, he graduated in 1920 as valedictorian of his class.
After graduation, Julian landed a fellowship at Harvard University to study chemistry—but here, Julian ran into yet another obstacle. Harvard thought that white students would resent being taught by Julian, an African-American man, so they withdrew his teaching assistantship. Julian instead decided to complete his PhD at the University of Vienna in Austria. When he did, he became one of the first African Americans to ever receive a PhD in chemistry.
Julian received offers for professorships, fellowships, and jobs throughout the 1930s, due to his impressive qualifications—but these offers were almost always revoked when schools or potential employers found out Julian was black. In one instance, Julian was offered a job at the Institute of Paper Chemistory in Appleton, Wisconsin—but Appleton, like many cities in the United States at the time, was known as a “sundown town,” which meant that black people weren’t allowed to be there after dark. As a result, Julian lost the job.
During this time, Julian became an expert at synthesis, which is the process of turning one substance into another through a series of planned chemical reactions. Julian synthesized a plant compound called physostigmine, which would later become a treatment for an eye disease called glaucoma.
In 1936, Julian was finally able to land—and keep—a job at Glidden, and there he found a way to extract soybean protein. This was used to produce a fire-retardant foam used in fire extinguishers to smother oil and gasoline fires aboard ships and aircraft carriers, and it ended up saving the lives of thousands of soldiers during World War II.
At Glidden, Julian found a way to synthesize human sex hormones such as progesterone, estrogen, and testosterone, from plants. This was a hugely profitable discovery for his company—but it also meant that clinicians now had huge quantities of these hormones, making hormone therapy cheaper and easier to come by. His work also laid the foundation for the creation of hormonal birth control: Without the ability to synthesize these hormones, hormonal birth control would not exist.
Julian left Glidden in the 1950s and formed his own company, called Julian Laboratories, outside of Chicago, where he manufactured steroids and conducted his own research. The company turned profitable within a year, but even so Julian’s obstacles weren’t over. In 1950 and 1951, Julian’s home was firebombed and attacked with dynamite, with his family inside. Julian often had to sit out on the front porch of his home with a shotgun to protect his family from violence.
But despite years of racism and violence, Julian’s story has a happy ending. Julian’s family was eventually welcomed into the neighborhood and protected from future attacks (Julian’s daughter lives there to this day). Julian then became one of the country’s first black millionaires when he sold his company in the 1960s.
When Julian passed away at the age of 76, he had more than 130 chemical patents to his name and left behind a body of work that benefits people to this day.
Therapies for Healthy Aging with Dr. Alexandra Bause
My guest today is Dr. Alexandra Bause, a biologist who has dedicated her career to advancing health, medicine and healthier human lifespans. Dr. Bause co-founded a company called Apollo Health Ventures in 2017. Currently a venture partner at Apollo, she's immersed in the discoveries underway in Apollo’s Venture Lab while the company focuses on assembling a team of investors to support progress. Dr. Bause and Apollo Health Ventures say that biotech is at “an inflection point” and is set to become a driver of important change and economic value.
Previously, Dr. Bause worked at the Boston Consulting Group in its healthcare practice specializing in biopharma strategy, among other priorities
She did her PhD studies at Harvard Medical School focusing on molecular mechanisms that contribute to cellular aging, and she’s also a trained pharmacist
In the episode, we talk about the present and future of therapeutics that could increase people’s spans of health, the benefits of certain lifestyle practice, the best use of electronic wearables for these purposes, and much more.
Dr. Bause is at the forefront of developing interventions that target the aging process with the aim of ensuring that all of us can have healthier, more productive lifespans.


