I’m a Black, Genderqueer Medical Student: Here’s My Hard-Won Wisdom for Students and Educational Institutions

Advice follows for how to improve higher education for marginalized communities.
This article is part of the magazine, "The Future of Science In America: The Election Issue," co-published by LeapsMag, the Aspen Institute Science & Society Program, and GOOD.
In the last 12 years, I have earned degrees from Harvard College and Duke University and trained in an M.D.-Ph.D. program at the University of Pennsylvania. Through this process, I have assembled much educational privilege and can now speak with the authority that is conferred in these ivory towers. Along the way, as a Black, genderqueer, first-generation, low-income trainee, the systems of oppression that permeate American society—racism, transphobia, and classism, among others—coalesced in the microcosm of academia into a unique set of challenges that I had to navigate. I would like to share some of the lessons I have learned over the years in the format of advice for both Black, Indigenous, and other People of Color (BIPOC) and LGBTQ+ trainees as well as members of the education institutions that seek to serve them.
To BIPOC and LGBTQ+ Trainees: Who you are is an asset, not an obstacle. Throughout my undergraduate years, I viewed my background as something to overcome. I had to overcome the instances of implicit bias and overt discrimination I experienced in my classes and among my peers. I had to overcome the preconceived, racialized, limitations on my abilities that academic advisors projected onto me as they characterized my course load as too ambitious or declared me unfit for medical school. I had to overcome the lack of social capital that comes with being from a low-resourced rural community and learn all the idiosyncrasies of academia from how to write professional emails to how and when to solicit feedback. I viewed my Blackness, queerness, and transness as inconveniences of identity that made my life harder.
It was only as I went on to graduate and medical school that I saw how much strength comes from who I am. My perspective allows me to conduct insightful, high-impact, and creative research that speaks to uplifting my various intersecting communities. My work on health equity for transgender people of color (TPOC) and BIPOC trainees in medicine is my form of advocacy. My publications are love letters to my communities, telling them that I see them and that I am with them. They are also indictments of the systems that oppress them and evidence that supports policy innovations and help move our society toward a more equitable future.
To Educators and Institutions: Allyship is active and uncomfortable. In the last 20 years, institutions have professed interest in diversifying their members and supporting marginalized groups. However, despite these proclamations, most have fallen short of truly allying themselves to communities in need of support. People often assume that allyship is defined by intent; that they are allies to Black people in the #BLM era because they, too, believe that Black lives have value. This is decency, not allyship. In the wake of the tragic killings of Breonna Taylor and George Floyd, and the ongoing racial inequity of the COVID-19 pandemic, every person of color that I know in academia has been invited to a townhall on racism. These meetings risk re-traumatizing Black people if they feel coerced into sharing their experiences with racism in front of their white colleagues. This is exploitation, not allyship. These discussions must be carefully designed to prioritize Black voices but not depend on them. They must rely on shared responsibility for strategizing systemic change that centers the needs of Black and marginalized voices while diffusing the requisite labor across the entire institution.
Allyship requires a commitment to actions, not ideas. In education this is fostering safe environments for BIPOC and LGBTQ+ students. It is changing the culture of your institution such that anti-racism is a shared value and that work to establish anti-racist practices is distributed across all groups rather than just an additional tax on minority students and faculty. It is providing dedicated spaces for BIPOC and LGBTQ+ students where they can build community amongst themselves away from the gaze of majority white, heterosexual, and cisgender groups that dominate other spaces. It is also building the infrastructure to educate all members of your institution on issues facing BIPOC and LGBTQ+ students rather than relying on members of those communities to educate others through divulging their personal experiences.
Among well-intentioned ally hopefuls, anxiety can be a major barrier to action. Anxiety around the possibility of making a mistake, saying the wrong thing, hurting or offending someone, and having uncomfortable conversations. I'm here to alleviate any uncertainty around that: You will likely make mistakes, you may receive backlash, you will undoubtedly have uncomfortable conversations, and you may have to apologize. Steel yourself to that possibility and view it as an asset. People give their most unfiltered feedback when they have been hurt, so take that as an opportunity to guide change within your organizations and your own practices. How you respond to criticism will determine your allyship status. People are more likely to forgive when a commitment to change is quickly and repeatedly demonstrated.
The first step to moving forward in an anti-racist framework is to compensate the students for their labor in making the institution more inclusive.
To BIPOC and LGBTQ+ Trainees: Your labor is worth compensation and recognition. It is difficult to see your institution failing to adequately support members of your community without feeling compelled to act. As a Black person in medicine I have served on nearly every committee related to diversity recruitment and admissions. As a queer person I have sat on many taskforces dedicated to improving trans education in medical curricula. I have spent countless hours improving the institutions at which I have been educated and will likely spend countless more. However, over the past few years, I have realized that those hours do not generally advance my academic and professional goals. My peers who do not share in my marginalized identities do not have the external pressure to sequester large parts of their time for institutional change. While I was drafting emails to administrators or preparing journal clubs to educate students on trans health, my peers were studying.
There were periods in my education where there were appreciable declines in my grades and research productivity because of the time I spent on institutional reform. Without care, this phenomenon can translate to a perceived achievement gap. It is not that BIPOC and LGBTQ+ achieve less; in fact, in many ways we achieve more. However, we expend much of our effort on activities that are not traditionally valued as accomplishments for career advancement. The only way to change this norm is to start demanding compensation for your labor and respectfully declining if it is not provided. Compensation can be monetary, but it can also be opportunities for professional identity formation. For uncompensated work that I feel particularly compelled to do, I strategize how it can benefit me before starting the project. Can I write it up for publication in a peer-reviewed scientific journal? Can I find an advisor to support the task force and write a letter of reference on my behalf? Can I use the project to apply for external research funding or scholarships? These are all ways of translating the work that matters to you into the currency that the medical establishment values as productivity.
To Educators and Institutions: Compensate marginalized members of your organizations for making it better. Racism is the oldest institution in America. It is built into the foundation of the country and rests in the very top office in our nation's capital. Analogues of racism, specifically gender-based discrimination, transphobia, and classism, have similarly seeped into the fabric of our country and education system. Given their ubiquity, how can we expect to combat these issues cheaply? Today, anti-racism work is in vogue in academia, and institutions have looked to their Black and otherwise marginalized students to provide ways that the institution can improve. We, as students, regularly respond with well-researched, scholarly, actionable lists of specific interventions that are the result of dozens (sometimes hundreds) of hours of unpaid labor. Then, administrators dissect these interventions and scale them back citing budgetary concerns or hiring limitations.
It gives the impression that they view racism as an easy issue to fix, that can be slotted in under an existing line item, rather than the severe problem requiring radical reform that it actually is. The first step to moving forward in an anti-racist framework is to compensate the students for their labor in making the institution more inclusive. Inclusion and equity improve the educational environment for all students, so in the same way one would pay a consultant for an audit that identifies weaknesses in your institution, you should pay your students who are investing countless hours in strategic planning. While financial compensation is usually preferable, institutions can endow specific equity-related student awards, fellowships, and research programs that allow the work that students are already doing to help further their careers. Next, it is important to invest. Add anti-racism and equity interventions as specific items in departmental and institutional budgets so that there is annual reserved capital dedicated to these improvements, part of which can include the aforementioned student compensation.
To BIPOC and LGBTQ+ Trainees: Seek and be mentors.Early in my training, I often lamented the lack of mentors who shared important identities with myself. I initially sought a Black, queer mentor in medicine who could open doors and guide me from undergrad pre-med to university professor. Unfortunately, given the composition of the U.S. academy, this was not a realistic goal. While our white, cisgender, heterosexual colleagues can identify mentors they reflect, we have to operate on a different mentorship model. In my experience, it is more effective to assemble a mentorship network: a group of allies who facilitate your professional and personal development across one or more arenas. For me, as a physician-scholar-advocate, I need professional mentors who support my specific research interests, help me develop as a policy innovator and advocate, and who can guide my overall career trajectory on the short- and long- term time scales.
Rather than expecting one mentor to fulfill all those roles, as well as be Black and queer, I instead seek a set of mentors that can share in these roles, all of whom are informed or educable on the unique needs of Black and queer trainees. When assembling your own mentorship network, remember personal mentors who can help you develop self-care strategies and achieve work-life balance. Also, there is much value in peer mentorship. Some of my best mentors are my contemporaries. Your experiences have allowed you to accumulate knowledge—share that knowledge with each other.
To Educators and Institutions: Hire better mentors. Be better mentors. Poor mentorship is a challenge throughout academia that is amplified for BIPOC and LGBTQ+ trainees. Part of this challenge is due to priorities established in the hiring process. Institutions need to update hiring practices to explicitly evaluate faculty and staff candidates for their ability to be good mentors, particularly to students from marginalized communities. This can be achieved by including diverse groups of students on hiring committees and allowing them to interview candidates and assess how the candidate will support student needs. Also, continually evaluate current faculty and staff based on standardized feedback from students that will allow you to identify and intervene on deficits and continually improve the quality of mentorship at your institution.
The suggestions I provided are about navigating medical education, as it exists now. I hope that incorporating these practices will allow institutions to better serve the BIPOC and LGBTQ+ trainees that help make their communities vibrant. I also hope that my fellow BIPOC and LGBTQ+ trainees can see themselves in this conversation and feel affirmed and equipped in navigating medicine based on the tools I provide here. However, my words are only a tempering measure. True justice in medical education and health will only happen when we overhaul our institutions and dismantle systems of oppression in our society.
[Editor's Note: To read other articles in this special magazine issue, visit the beautifully designed e-reader version.]
Thanks to safety cautions from the COVID-19 pandemic, a strain of influenza has been completely eliminated.
If you were one of the millions who masked up, washed your hands thoroughly and socially distanced, pat yourself on the back—you may have helped change the course of human history.
Scientists say that thanks to these safety precautions, which were introduced in early 2020 as a way to stop transmission of the novel COVID-19 virus, a strain of influenza has been completely eliminated. This marks the first time in human history that a virus has been wiped out through non-pharmaceutical interventions, such as vaccines.
The flu shot, explained
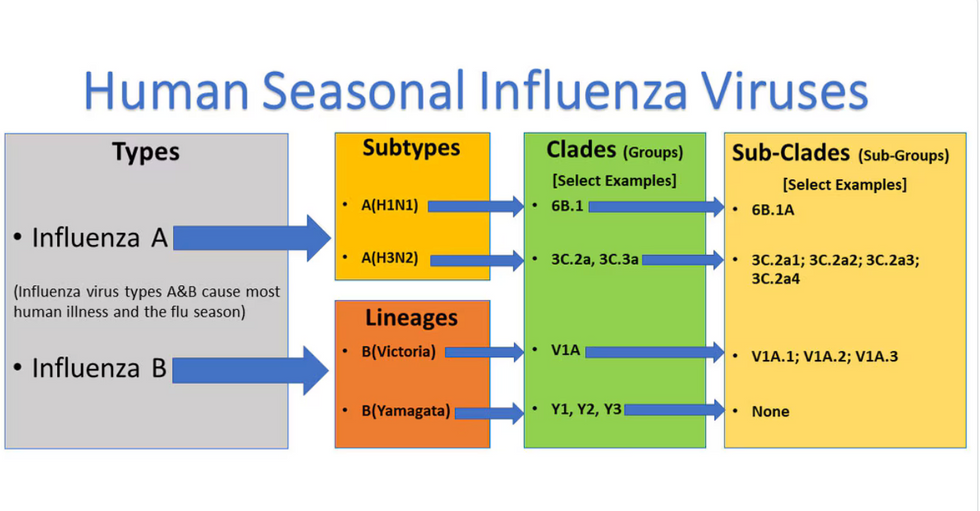
Influenza viruses type A and B are responsible for the majority of human illnesses and the flu season.
Centers for Disease Control
For more than a decade, flu shots have protected against two types of the influenza virus–type A and type B. While there are four different strains of influenza in existence (A, B, C, and D), only strains A, B, and C are capable of infecting humans, and only A and B cause pandemics. In other words, if you catch the flu during flu season, you’re most likely sick with flu type A or B.
Flu vaccines contain inactivated—or dead—influenza virus. These inactivated viruses can’t cause sickness in humans, but when administered as part of a vaccine, they teach a person’s immune system to recognize and kill those viruses when they’re encountered in the wild.
Each spring, a panel of experts gives a recommendation to the US Food and Drug Administration on which strains of each flu type to include in that year’s flu vaccine, depending on what surveillance data says is circulating and what they believe is likely to cause the most illness during the upcoming flu season. For the past decade, Americans have had access to vaccines that provide protection against two strains of influenza A and two lineages of influenza B, known as the Victoria lineage and the Yamagata lineage. But this year, the seasonal flu shot won’t include the Yamagata strain, because the Yamagata strain is no longer circulating among humans.
How Yamagata Disappeared

Flu surveillance data from the Global Initiative on Sharing All Influenza Data (GISAID) shows that the Yamagata lineage of flu type B has not been sequenced since April 2020.
Nature
Experts believe that the Yamagata lineage had already been in decline before the pandemic hit, likely because the strain was naturally less capable of infecting large numbers of people compared to the other strains. When the COVID-19 pandemic hit, the resulting safety precautions such as social distancing, isolating, hand-washing, and masking were enough to drive the virus into extinction completely.
Because the strain hasn’t been circulating since 2020, the FDA elected to remove the Yamagata strain from the seasonal flu vaccine. This will mark the first time since 2012 that the annual flu shot will be trivalent (three-component) rather than quadrivalent (four-component).
Should I still get the flu shot?
The flu shot will protect against fewer strains this year—but that doesn’t mean we should skip it. Influenza places a substantial health burden on the United States every year, responsible for hundreds of thousands of hospitalizations and tens of thousands of deaths. The flu shot has been shown to prevent millions of illnesses each year (more than six million during the 2022-2023 season). And while it’s still possible to catch the flu after getting the flu shot, studies show that people are far less likely to be hospitalized or die when they’re vaccinated.
Another unexpected benefit of dropping the Yamagata strain from the seasonal vaccine? This will possibly make production of the flu vaccine faster, and enable manufacturers to make more vaccines, helping countries who have a flu vaccine shortage and potentially saving millions more lives.
After his grandmother’s dementia diagnosis, one man invented a snack to keep her healthy and hydrated.
Founder Lewis Hornby and his grandmother Pat, sampling Jelly Drops—an edible gummy containing water and life-saving electrolytes.
On a visit to his grandmother’s nursing home in 2016, college student Lewis Hornby made a shocking discovery: Dehydration is a common (and dangerous) problem among seniors—especially those that are diagnosed with dementia.
Hornby’s grandmother, Pat, had always had difficulty keeping up her water intake as she got older, a common issue with seniors. As we age, our body composition changes, and we naturally hold less water than younger adults or children, so it’s easier to become dehydrated quickly if those fluids aren’t replenished. What’s more, our thirst signals diminish naturally as we age as well—meaning our body is not as good as it once was in letting us know that we need to rehydrate. This often creates a perfect storm that commonly leads to dehydration. In Pat’s case, her dehydration was so severe she nearly died.
When Lewis Hornby visited his grandmother at her nursing home afterward, he learned that dehydration especially affects people with dementia, as they often don’t feel thirst cues at all, or may not recognize how to use cups correctly. But while dementia patients often don’t remember to drink water, it seemed to Hornby that they had less problem remembering to eat, particularly candy.

Hornby wanted to create a solution for elderly people who struggled keeping their fluid intake up. He spent the next eighteen months researching and designing a solution and securing funding for his project. In 2019, Hornby won a sizable grant from the Alzheimer’s Society, a UK-based care and research charity for people with dementia and their caregivers. Together, through the charity’s Accelerator Program, they created a bite-sized, sugar-free, edible jelly drop that looked and tasted like candy. The candy, called Jelly Drops, contained 95% water and electrolytes—important minerals that are often lost during dehydration. The final product launched in 2020—and was an immediate success. The drops were able to provide extra hydration to the elderly, as well as help keep dementia patients safe, since dehydration commonly leads to confusion, hospitalization, and sometimes even death.
Not only did Jelly Drops quickly become a favorite snack among dementia patients in the UK, but they were able to provide an additional boost of hydration to hospital workers during the pandemic. In NHS coronavirus hospital wards, patients infected with the virus were regularly given Jelly Drops to keep their fluid levels normal—and staff members snacked on them as well, since long shifts and personal protective equipment (PPE) they were required to wear often left them feeling parched.
In April 2022, Jelly Drops launched in the United States. The company continues to donate 1% of its profits to help fund Alzheimer’s research.

