I’m a Black, Genderqueer Medical Student: Here’s My Hard-Won Wisdom for Students and Educational Institutions

Advice follows for how to improve higher education for marginalized communities.
This article is part of the magazine, "The Future of Science In America: The Election Issue," co-published by LeapsMag, the Aspen Institute Science & Society Program, and GOOD.
In the last 12 years, I have earned degrees from Harvard College and Duke University and trained in an M.D.-Ph.D. program at the University of Pennsylvania. Through this process, I have assembled much educational privilege and can now speak with the authority that is conferred in these ivory towers. Along the way, as a Black, genderqueer, first-generation, low-income trainee, the systems of oppression that permeate American society—racism, transphobia, and classism, among others—coalesced in the microcosm of academia into a unique set of challenges that I had to navigate. I would like to share some of the lessons I have learned over the years in the format of advice for both Black, Indigenous, and other People of Color (BIPOC) and LGBTQ+ trainees as well as members of the education institutions that seek to serve them.
To BIPOC and LGBTQ+ Trainees: Who you are is an asset, not an obstacle. Throughout my undergraduate years, I viewed my background as something to overcome. I had to overcome the instances of implicit bias and overt discrimination I experienced in my classes and among my peers. I had to overcome the preconceived, racialized, limitations on my abilities that academic advisors projected onto me as they characterized my course load as too ambitious or declared me unfit for medical school. I had to overcome the lack of social capital that comes with being from a low-resourced rural community and learn all the idiosyncrasies of academia from how to write professional emails to how and when to solicit feedback. I viewed my Blackness, queerness, and transness as inconveniences of identity that made my life harder.
It was only as I went on to graduate and medical school that I saw how much strength comes from who I am. My perspective allows me to conduct insightful, high-impact, and creative research that speaks to uplifting my various intersecting communities. My work on health equity for transgender people of color (TPOC) and BIPOC trainees in medicine is my form of advocacy. My publications are love letters to my communities, telling them that I see them and that I am with them. They are also indictments of the systems that oppress them and evidence that supports policy innovations and help move our society toward a more equitable future.
To Educators and Institutions: Allyship is active and uncomfortable. In the last 20 years, institutions have professed interest in diversifying their members and supporting marginalized groups. However, despite these proclamations, most have fallen short of truly allying themselves to communities in need of support. People often assume that allyship is defined by intent; that they are allies to Black people in the #BLM era because they, too, believe that Black lives have value. This is decency, not allyship. In the wake of the tragic killings of Breonna Taylor and George Floyd, and the ongoing racial inequity of the COVID-19 pandemic, every person of color that I know in academia has been invited to a townhall on racism. These meetings risk re-traumatizing Black people if they feel coerced into sharing their experiences with racism in front of their white colleagues. This is exploitation, not allyship. These discussions must be carefully designed to prioritize Black voices but not depend on them. They must rely on shared responsibility for strategizing systemic change that centers the needs of Black and marginalized voices while diffusing the requisite labor across the entire institution.
Allyship requires a commitment to actions, not ideas. In education this is fostering safe environments for BIPOC and LGBTQ+ students. It is changing the culture of your institution such that anti-racism is a shared value and that work to establish anti-racist practices is distributed across all groups rather than just an additional tax on minority students and faculty. It is providing dedicated spaces for BIPOC and LGBTQ+ students where they can build community amongst themselves away from the gaze of majority white, heterosexual, and cisgender groups that dominate other spaces. It is also building the infrastructure to educate all members of your institution on issues facing BIPOC and LGBTQ+ students rather than relying on members of those communities to educate others through divulging their personal experiences.
Among well-intentioned ally hopefuls, anxiety can be a major barrier to action. Anxiety around the possibility of making a mistake, saying the wrong thing, hurting or offending someone, and having uncomfortable conversations. I'm here to alleviate any uncertainty around that: You will likely make mistakes, you may receive backlash, you will undoubtedly have uncomfortable conversations, and you may have to apologize. Steel yourself to that possibility and view it as an asset. People give their most unfiltered feedback when they have been hurt, so take that as an opportunity to guide change within your organizations and your own practices. How you respond to criticism will determine your allyship status. People are more likely to forgive when a commitment to change is quickly and repeatedly demonstrated.
The first step to moving forward in an anti-racist framework is to compensate the students for their labor in making the institution more inclusive.
To BIPOC and LGBTQ+ Trainees: Your labor is worth compensation and recognition. It is difficult to see your institution failing to adequately support members of your community without feeling compelled to act. As a Black person in medicine I have served on nearly every committee related to diversity recruitment and admissions. As a queer person I have sat on many taskforces dedicated to improving trans education in medical curricula. I have spent countless hours improving the institutions at which I have been educated and will likely spend countless more. However, over the past few years, I have realized that those hours do not generally advance my academic and professional goals. My peers who do not share in my marginalized identities do not have the external pressure to sequester large parts of their time for institutional change. While I was drafting emails to administrators or preparing journal clubs to educate students on trans health, my peers were studying.
There were periods in my education where there were appreciable declines in my grades and research productivity because of the time I spent on institutional reform. Without care, this phenomenon can translate to a perceived achievement gap. It is not that BIPOC and LGBTQ+ achieve less; in fact, in many ways we achieve more. However, we expend much of our effort on activities that are not traditionally valued as accomplishments for career advancement. The only way to change this norm is to start demanding compensation for your labor and respectfully declining if it is not provided. Compensation can be monetary, but it can also be opportunities for professional identity formation. For uncompensated work that I feel particularly compelled to do, I strategize how it can benefit me before starting the project. Can I write it up for publication in a peer-reviewed scientific journal? Can I find an advisor to support the task force and write a letter of reference on my behalf? Can I use the project to apply for external research funding or scholarships? These are all ways of translating the work that matters to you into the currency that the medical establishment values as productivity.
To Educators and Institutions: Compensate marginalized members of your organizations for making it better. Racism is the oldest institution in America. It is built into the foundation of the country and rests in the very top office in our nation's capital. Analogues of racism, specifically gender-based discrimination, transphobia, and classism, have similarly seeped into the fabric of our country and education system. Given their ubiquity, how can we expect to combat these issues cheaply? Today, anti-racism work is in vogue in academia, and institutions have looked to their Black and otherwise marginalized students to provide ways that the institution can improve. We, as students, regularly respond with well-researched, scholarly, actionable lists of specific interventions that are the result of dozens (sometimes hundreds) of hours of unpaid labor. Then, administrators dissect these interventions and scale them back citing budgetary concerns or hiring limitations.
It gives the impression that they view racism as an easy issue to fix, that can be slotted in under an existing line item, rather than the severe problem requiring radical reform that it actually is. The first step to moving forward in an anti-racist framework is to compensate the students for their labor in making the institution more inclusive. Inclusion and equity improve the educational environment for all students, so in the same way one would pay a consultant for an audit that identifies weaknesses in your institution, you should pay your students who are investing countless hours in strategic planning. While financial compensation is usually preferable, institutions can endow specific equity-related student awards, fellowships, and research programs that allow the work that students are already doing to help further their careers. Next, it is important to invest. Add anti-racism and equity interventions as specific items in departmental and institutional budgets so that there is annual reserved capital dedicated to these improvements, part of which can include the aforementioned student compensation.
To BIPOC and LGBTQ+ Trainees: Seek and be mentors. Early in my training, I often lamented the lack of mentors who shared important identities with myself. I initially sought a Black, queer mentor in medicine who could open doors and guide me from undergrad pre-med to university professor. Unfortunately, given the composition of the U.S. academy, this was not a realistic goal. While our white, cisgender, heterosexual colleagues can identify mentors they reflect, we have to operate on a different mentorship model. In my experience, it is more effective to assemble a mentorship network: a group of allies who facilitate your professional and personal development across one or more arenas. For me, as a physician-scholar-advocate, I need professional mentors who support my specific research interests, help me develop as a policy innovator and advocate, and who can guide my overall career trajectory on the short- and long- term time scales.
Rather than expecting one mentor to fulfill all those roles, as well as be Black and queer, I instead seek a set of mentors that can share in these roles, all of whom are informed or educable on the unique needs of Black and queer trainees. When assembling your own mentorship network, remember personal mentors who can help you develop self-care strategies and achieve work-life balance. Also, there is much value in peer mentorship. Some of my best mentors are my contemporaries. Your experiences have allowed you to accumulate knowledge—share that knowledge with each other.
To Educators and Institutions: Hire better mentors. Be better mentors. Poor mentorship is a challenge throughout academia that is amplified for BIPOC and LGBTQ+ trainees. Part of this challenge is due to priorities established in the hiring process. Institutions need to update hiring practices to explicitly evaluate faculty and staff candidates for their ability to be good mentors, particularly to students from marginalized communities. This can be achieved by including diverse groups of students on hiring committees and allowing them to interview candidates and assess how the candidate will support student needs. Also, continually evaluate current faculty and staff based on standardized feedback from students that will allow you to identify and intervene on deficits and continually improve the quality of mentorship at your institution.
The suggestions I provided are about navigating medical education, as it exists now. I hope that incorporating these practices will allow institutions to better serve the BIPOC and LGBTQ+ trainees that help make their communities vibrant. I also hope that my fellow BIPOC and LGBTQ+ trainees can see themselves in this conversation and feel affirmed and equipped in navigating medicine based on the tools I provide here. However, my words are only a tempering measure. True justice in medical education and health will only happen when we overhaul our institutions and dismantle systems of oppression in our society.
[Editor's Note: To read other articles in this special magazine issue, visit the beautifully designed e-reader version.]
Stronger psychedelics that rewire the brain, with Doug Drysdale
Today's podcast episode features Doug Drysdale, CEO of Cybin, a company that is leading innovations in psilocybin, mushrooms that may help people with anxiety and depression.
A promising development in science in recent years has been the use technology to optimize something natural. One-upping nature's wisdom isn't easy. In many cases, we haven't - and maybe we can't - figure it out. But today's episode features a fascinating example: using tech to optimize psychedelic mushrooms.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
These mushrooms have been used for religious, spiritual and medicinal purposes for thousands of years, but only in the past several decades have scientists brought psychedelics into the lab to enhance them and maximize their therapeutic value.
Today’s podcast guest, Doug Drysdale, is doing important work to lead this effort. Drysdale is the CEO of a company called Cybin that has figured out how to make psilocybin more potent, so it can be administered in smaller doses without side effects.
The natural form of psilocybin has been studied increasingly in the realm of mental health. Taking doses of these mushrooms appears to help people with anxiety and depression by spurring the development of connections in the brain, an example of neuroplasticity. The process basically shifts the adult brain from being fairly rigid like dried clay into a malleable substance like warm wax - the state of change that's constantly underway in the developing brains of children.
Neuroplasticity in adults seems to unlock some of our default ways of of thinking, the habitual thought patterns that’ve been associated with various mental health problems. Some promising research suggests that psilocybin causes a reset of sorts. It makes way for new, healthier thought patterns.
So what is Drysdale’s secret weapon to bring even more therapeutic value to psilocybin? It’s a process called deuteration. It focuses on the hydrogen atoms in psilocybin. These atoms are very light and don’t stick very well to carbon, which is another atom in psilocybin. As a result, our bodies can easily breaks down the bonds between the hydrogen and carbon atoms. For many people, that means psilocybin gets cleared from the body too quickly, before it can have a therapeutic benefit.
In deuteration, scientists do something simple but ingenious: they replace the hydrogen atoms with a molecule called deuterium. It’s twice as heavy as hydrogen and forms tighter bonds with the carbon. Because these pairs are so rock-steady, they slow down the rate at which psilocybin is metabolized, so it has more sustained effects on our brains.
Cybin isn’t Drysdale’s first go around at this - far from it. He has over 30 years of experience in the healthcare sector. During this time he’s raised around $4 billion of both public and private capital, and has been named Ernst and Young Entrepreneur of the Year. Before Cybin, he was the founding CEO of a pharmaceutical company called Alvogen, leading it from inception to around $500 million in revenues, across 35 countries. Drysdale has also been the head of mergers and acquisitions at Actavis Group, leading 15 corporate acquisitions across three continents.
In this episode, Drysdale walks us through the promising research of his current company, Cybin, and the different therapies he’s developing for anxiety and depression based not just on psilocybin but another psychedelic compound found in plants called DMT. He explains how they seem to have such powerful effects on the brain, as well as the potential for psychedelics to eventually support other use cases, including helping us strive toward higher levels of well-being. He goes on to discuss his views on mindfulness and lifestyle factors - such as optimal nutrition - that could help bring out hte best in psychedelics.
Show links:
Doug Drysdale full bio
Doug Drysdale twitter
Cybin website
Cybin development pipeline
Cybin's promising phase 2 research on depression
Johns Hopkins psychedelics research and psilocybin research
Mets owner Steve Cohen invests in psychedelic therapies

Doug Drysdale, CEO of Cybin
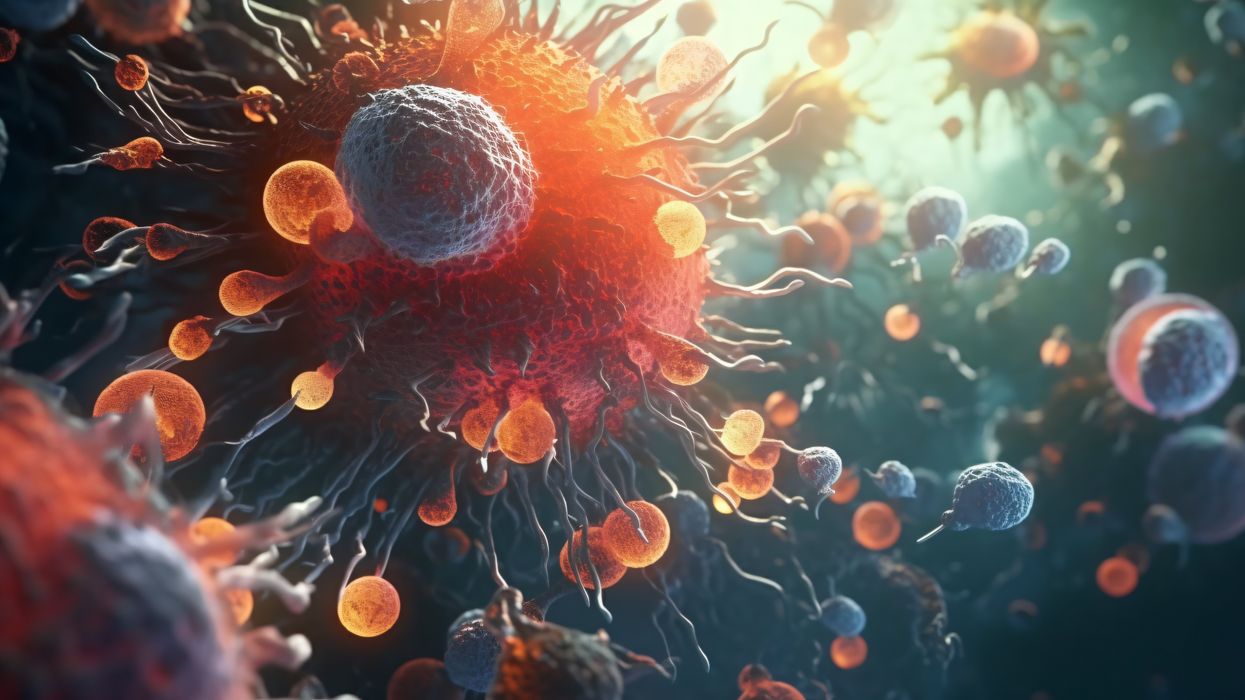
How the body's immune resilience affects our health and lifespan
Immune cells battle an infection.
Story by Big Think
It is a mystery why humans manifest vast differences in lifespan, health, and susceptibility to infectious diseases. However, a team of international scientists has revealed that the capacity to resist or recover from infections and inflammation (a trait they call “immune resilience”) is one of the major contributors to these differences.
Immune resilience involves controlling inflammation and preserving or rapidly restoring immune activity at any age, explained Weijing He, a study co-author. He and his colleagues discovered that people with the highest level of immune resilience were more likely to live longer, resist infection and recurrence of skin cancer, and survive COVID and sepsis.
Measuring immune resilience
The researchers measured immune resilience in two ways. The first is based on the relative quantities of two types of immune cells, CD4+ T cells and CD8+ T cells. CD4+ T cells coordinate the immune system’s response to pathogens and are often used to measure immune health (with higher levels typically suggesting a stronger immune system). However, in 2021, the researchers found that a low level of CD8+ T cells (which are responsible for killing damaged or infected cells) is also an important indicator of immune health. In fact, patients with high levels of CD4+ T cells and low levels of CD8+ T cells during SARS-CoV-2 and HIV infection were the least likely to develop severe COVID and AIDS.
Individuals with optimal levels of immune resilience were more likely to live longer.
In the same 2021 study, the researchers identified a second measure of immune resilience that involves two gene expression signatures correlated with an infected person’s risk of death. One of the signatures was linked to a higher risk of death; it includes genes related to inflammation — an essential process for jumpstarting the immune system but one that can cause considerable damage if left unbridled. The other signature was linked to a greater chance of survival; it includes genes related to keeping inflammation in check. These genes help the immune system mount a balanced immune response during infection and taper down the response after the threat is gone. The researchers found that participants who expressed the optimal combination of genes lived longer.
Immune resilience and longevity
The researchers assessed levels of immune resilience in nearly 50,000 participants of different ages and with various types of challenges to their immune systems, including acute infections, chronic diseases, and cancers. Their evaluation demonstrated that individuals with optimal levels of immune resilience were more likely to live longer, resist HIV and influenza infections, resist recurrence of skin cancer after kidney transplant, survive COVID infection, and survive sepsis.
However, a person’s immune resilience fluctuates all the time. Study participants who had optimal immune resilience before common symptomatic viral infections like a cold or the flu experienced a shift in their gene expression to poor immune resilience within 48 hours of symptom onset. As these people recovered from their infection, many gradually returned to the more favorable gene expression levels they had before. However, nearly 30% who once had optimal immune resilience did not fully regain that survival-associated profile by the end of the cold and flu season, even though they had recovered from their illness.
Intriguingly, some people who are 90+ years old still have optimal immune resilience, suggesting that these individuals’ immune systems have an exceptional capacity to control inflammation and rapidly restore proper immune balance.
This could suggest that the recovery phase varies among people and diseases. For example, young female sex workers who had many clients and did not use condoms — and thus were repeatedly exposed to sexually transmitted pathogens — had very low immune resilience. However, most of the sex workers who began reducing their exposure to sexually transmitted pathogens by using condoms and decreasing their number of sex partners experienced an improvement in immune resilience over the next 10 years.
Immune resilience and aging
The researchers found that the proportion of people with optimal immune resilience tended to be highest among the young and lowest among the elderly. The researchers suggest that, as people age, they are exposed to increasingly more health conditions (acute infections, chronic diseases, cancers, etc.) which challenge their immune systems to undergo a “respond-and-recover” cycle. During the response phase, CD8+ T cells and inflammatory gene expression increase, and during the recovery phase, they go back down.
However, over a lifetime of repeated challenges, the immune system is slower to recover, altering a person’s immune resilience. Intriguingly, some people who are 90+ years old still have optimal immune resilience, suggesting that these individuals’ immune systems have an exceptional capacity to control inflammation and rapidly restore proper immune balance despite the many respond-and-recover cycles that their immune systems have faced.
Public health ramifications could be significant. Immune cell and gene expression profile assessments are relatively simple to conduct, and being able to determine a person’s immune resilience can help identify whether someone is at greater risk for developing diseases, how they will respond to treatment, and whether, as well as to what extent, they will recover.