I'm a Healthy Young Woman: Here's Why I Would Get Tested for Alzheimer's Now
The author as a child with her father in 1981, before he was diagnosed with Alzheimer's.
Editor's Note: A team of researchers in Italy recently used artificial intelligence and machine learning to diagnose Alzheimer's disease on a brain scan an entire decade before symptoms show up in the patient. While some people argue that early detection is critical, others believe the knowledge would do more harm than good. LeapsMag invited contributors with opposite opinions to share their perspectives.
Alzheimer's doesn't run in my family. When my father was diagnosed at the age of 58, we looked at his familial history. Both his parents lived into their late 80's. All of their surviving siblings were similarly long-lived and none had had Alzheimer's or any related dementias. My dad had spent 20 years working for the United Nations in the 60's and 70's in Africa. He was convinced that the Alzheimer's had come from his time spent in dodgy mines where he was exposed without the proper protections to all kinds of chemical processes.
Maybe that was true. Maybe it wasn't. The theory that metals, particularly aluminum, is an environmental factor leading to Alzheimer's has been around for a while. It's mostly been debunked, but clearly something is causing this epidemic as the vast majority of the cases in the world today are age-related. But no one knows what the trigger is, nor are we close to knowing.
If my father had had the Alzheimer's gene, I would go get myself checked for it. If some new MRI were commercially available to scan my brain and let me know if I was developing Alzheimer's, I would also take that test. There are four reasons why.
First, studies have shown that lifestyle has a major impact on the disease. I already run three miles a day. I eat relatively healthily. But like anyone, I don't live strictly on boiled chicken and broccoli. And I definitely enjoy a glass of wine or two. If I knew I had a propensity for the disease, or was developing it, I would be more diligent. I would eat my broccoli and cut out my wine. Life would be less fun, but I'd get more life and that's what's important.

The last picture taken of the author with her father before his death, in 2015.
Secondly, I would also have time to create an end-of-life plan the way my father did not. He told me repeatedly early on in his diagnosis that he did not want to live when he no longer knew me, when he became a burden, when he couldn't feed or bathe himself. I did my best in his final years to help him die quicker: I know that was what he wanted. But, given U.S. laws, all that meant was taking him off his heart and stroke medications and letting him eat anything he wanted, no matter how unhealthy. Knowing what's to come, having seen him go through it, I might consider moving to Belgium, which has begun to allow assisted suicide of those living with Alzheimer's and dementia if they can clearly state their intentions early on in the disease when they still have clarity of mind.
Next, I could help. Right now, there are dozens of Alzheimer's and dementia studies in the works. They are short thousands of willing test subjects. One of the top barriers to learning what's triggering the disease, and finding a cure, is populating these studies. So, knowing would make me a stronger candidate and would potentially help others down the road.
Finally, it would change my priorities. My father died the longest death possible: he succumbed last year more than 15 years after his diagnosis. My mother died the quickest possible way: she had a stress-related brain aneurysm 10 years after my father's diagnosis. Caring for him was too much for her and aneurysms ran in her family; her mother died of one as well. I already get a scan once every five years to see if I'm developing a brain aneurysm. If I am, odds are only 66% that they can operate on it—some aneurysms develop much too deep in the brain to operate, like my mother's.
Would she have wanted to know? Even though the aneurysm in her case was inoperable? I'm not sure. But I imagine if she had known, she would've lived her final years differently. She might have taken that trip to Alaska that she debated but thought was too expensive. She might have gotten organized earlier to make out a will so I wasn't left with chaos in the wake of her death; we'd planned for my father's death, knowing he was ill, but not my mother's. And she might have finally gotten around to dictating her story to me, as she'd always promised me she would when she found the time.
Telling my father's story at the end of his life helped his care.
With my startup MemoryWell, I spend my life now collecting senior stories before they are lost, in part because telling my father's story at the end of his life helped his care. But it's also in part for the story I lost with my mother.
If I knew that my time was limited, I'd not worry so much about saving for retirement. I'd make progress on my bucket list: hike Machu Picchu, scuba dive the Maldives, or raft the Grand Canyon. I'd tell my loved ones as much as I can in my time remaining how much they mean to me. And I would spend more time writing my own story to pass it down—finally finishing the book I've been working on. Maybe it's the writer in me, or maybe it's that I don't have kids of my own yet to carry on a legacy, but I'd want my story to be known, to have others learn from my experiences. And that's the biggest gift knowing would give me.
Editor's Note: Consider the other side of the argument here.
Thanks to safety cautions from the COVID-19 pandemic, a strain of influenza has been completely eliminated.
If you were one of the millions who masked up, washed your hands thoroughly and socially distanced, pat yourself on the back—you may have helped change the course of human history.
Scientists say that thanks to these safety precautions, which were introduced in early 2020 as a way to stop transmission of the novel COVID-19 virus, a strain of influenza has been completely eliminated. This marks the first time in human history that a virus has been wiped out through non-pharmaceutical interventions, such as vaccines.
The flu shot, explained
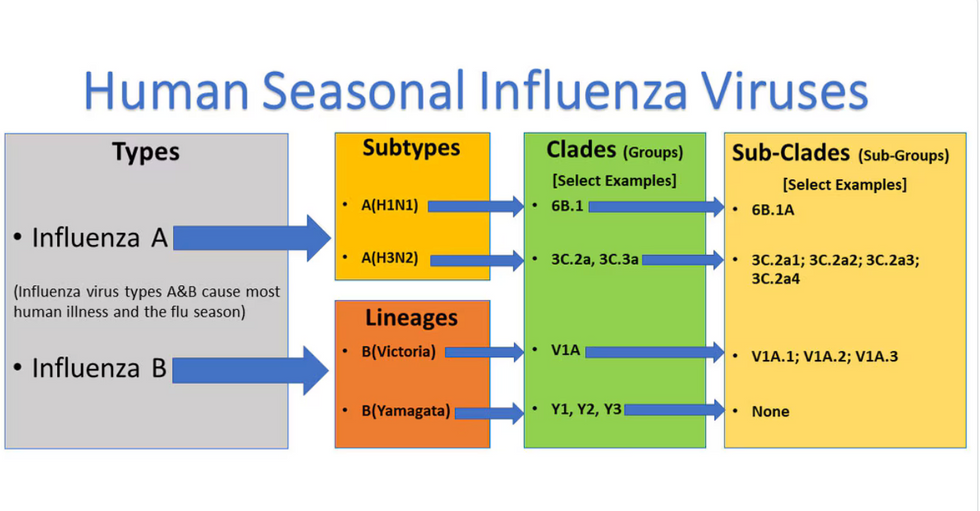
Influenza viruses type A and B are responsible for the majority of human illnesses and the flu season.
Centers for Disease Control
For more than a decade, flu shots have protected against two types of the influenza virus–type A and type B. While there are four different strains of influenza in existence (A, B, C, and D), only strains A, B, and C are capable of infecting humans, and only A and B cause pandemics. In other words, if you catch the flu during flu season, you’re most likely sick with flu type A or B.
Flu vaccines contain inactivated—or dead—influenza virus. These inactivated viruses can’t cause sickness in humans, but when administered as part of a vaccine, they teach a person’s immune system to recognize and kill those viruses when they’re encountered in the wild.
Each spring, a panel of experts gives a recommendation to the US Food and Drug Administration on which strains of each flu type to include in that year’s flu vaccine, depending on what surveillance data says is circulating and what they believe is likely to cause the most illness during the upcoming flu season. For the past decade, Americans have had access to vaccines that provide protection against two strains of influenza A and two lineages of influenza B, known as the Victoria lineage and the Yamagata lineage. But this year, the seasonal flu shot won’t include the Yamagata strain, because the Yamagata strain is no longer circulating among humans.
How Yamagata Disappeared

Flu surveillance data from the Global Initiative on Sharing All Influenza Data (GISAID) shows that the Yamagata lineage of flu type B has not been sequenced since April 2020.
Nature
Experts believe that the Yamagata lineage had already been in decline before the pandemic hit, likely because the strain was naturally less capable of infecting large numbers of people compared to the other strains. When the COVID-19 pandemic hit, the resulting safety precautions such as social distancing, isolating, hand-washing, and masking were enough to drive the virus into extinction completely.
Because the strain hasn’t been circulating since 2020, the FDA elected to remove the Yamagata strain from the seasonal flu vaccine. This will mark the first time since 2012 that the annual flu shot will be trivalent (three-component) rather than quadrivalent (four-component).
Should I still get the flu shot?
The flu shot will protect against fewer strains this year—but that doesn’t mean we should skip it. Influenza places a substantial health burden on the United States every year, responsible for hundreds of thousands of hospitalizations and tens of thousands of deaths. The flu shot has been shown to prevent millions of illnesses each year (more than six million during the 2022-2023 season). And while it’s still possible to catch the flu after getting the flu shot, studies show that people are far less likely to be hospitalized or die when they’re vaccinated.
Another unexpected benefit of dropping the Yamagata strain from the seasonal vaccine? This will possibly make production of the flu vaccine faster, and enable manufacturers to make more vaccines, helping countries who have a flu vaccine shortage and potentially saving millions more lives.
After his grandmother’s dementia diagnosis, one man invented a snack to keep her healthy and hydrated.
Founder Lewis Hornby and his grandmother Pat, sampling Jelly Drops—an edible gummy containing water and life-saving electrolytes.
On a visit to his grandmother’s nursing home in 2016, college student Lewis Hornby made a shocking discovery: Dehydration is a common (and dangerous) problem among seniors—especially those that are diagnosed with dementia.
Hornby’s grandmother, Pat, had always had difficulty keeping up her water intake as she got older, a common issue with seniors. As we age, our body composition changes, and we naturally hold less water than younger adults or children, so it’s easier to become dehydrated quickly if those fluids aren’t replenished. What’s more, our thirst signals diminish naturally as we age as well—meaning our body is not as good as it once was in letting us know that we need to rehydrate. This often creates a perfect storm that commonly leads to dehydration. In Pat’s case, her dehydration was so severe she nearly died.
When Lewis Hornby visited his grandmother at her nursing home afterward, he learned that dehydration especially affects people with dementia, as they often don’t feel thirst cues at all, or may not recognize how to use cups correctly. But while dementia patients often don’t remember to drink water, it seemed to Hornby that they had less problem remembering to eat, particularly candy.

Hornby wanted to create a solution for elderly people who struggled keeping their fluid intake up. He spent the next eighteen months researching and designing a solution and securing funding for his project. In 2019, Hornby won a sizable grant from the Alzheimer’s Society, a UK-based care and research charity for people with dementia and their caregivers. Together, through the charity’s Accelerator Program, they created a bite-sized, sugar-free, edible jelly drop that looked and tasted like candy. The candy, called Jelly Drops, contained 95% water and electrolytes—important minerals that are often lost during dehydration. The final product launched in 2020—and was an immediate success. The drops were able to provide extra hydration to the elderly, as well as help keep dementia patients safe, since dehydration commonly leads to confusion, hospitalization, and sometimes even death.
Not only did Jelly Drops quickly become a favorite snack among dementia patients in the UK, but they were able to provide an additional boost of hydration to hospital workers during the pandemic. In NHS coronavirus hospital wards, patients infected with the virus were regularly given Jelly Drops to keep their fluid levels normal—and staff members snacked on them as well, since long shifts and personal protective equipment (PPE) they were required to wear often left them feeling parched.
In April 2022, Jelly Drops launched in the United States. The company continues to donate 1% of its profits to help fund Alzheimer’s research.

