A new approach to kidney transplants would reprogram the immune system

If approved by the FDA, a new procedure for kidney transplants that doesn't require anti-rejection medication could soon become the standard of care.
Talaris Therapeutics, Inc., a biotech company based in Louisville, Ky., is edging closer to eradicating the need for immunosuppressive drugs for kidney transplant patients.
In a series of research trials, Talaris is infusing patients with immune system stem cells from their kidney donor to create a donor-derived immune system that accepts the organ without the need for anti-rejection medications. That newly generated system does not attack other parts of the recipient’s body and also fights off infections and diseases as a healthy immune system would.
Talaris is now moving into the final clinical trial, phase III, before submitting for FDA approval. Known as Freedom-1, this trial has 17 sites open throughout the U.S., and Talaris will enroll a total of 120 kidney transplant recipients. One day after receiving their donor’s kidney, 80 people will undergo the company’s therapy, involving the donor’s stem cells and other critical cells that are processed at their facility. Forty will have a regular kidney transplant and remain on immunosuppression to provide a control group.
“The beauty of this procedure is that I don’t have to take all of the anti-rejection drugs,” says Robert Waddell, a finance professional. “I forget that I ever had any kidney issues. That’s how impactful it is.”
The procedure was pioneered decades ago by Suzanne Ildstad as a faculty member at the University of Pittsburgh before she became founding CEO of Talaris and then its Chief Scientific Officer. If approved by the FDA, the method could soon become the standard of care for patients in need of a kidney transplant.
“We are working to find a way to reprogram the immune system of transplant recipients so that it sees the donated organ as [belonging to one]self and doesn’t attack it,” explains Scott Requadt, CEO of Talaris. “That obviates the need for lifelong immunosuppression.”
Each year, there are roughly 20,000 kidney transplants, making kidneys the most transplanted organ. About 6,500 of those come from living donors, while deceased donors provide roughly 13,000.
One of the challenges, Requadt points out, is that kidney transplant recipients aren’t always aware of all the implications of immunosuppression. Typically, they will need to take about 20 anti-rejection drugs several times a day to provide immunosuppression as well as treat complications caused by the toxicities of immunosuppression medications. The side effects of chronic immunosuppression include weight gain, high blood pressure, and high cholesterol. These cardiovascular comorbidities, Requadt says, are “often more frequently the cause of death than failure of a transplanted organ.”
Patients who are chronically immunosuppressed generally have much higher rates of infections and cancers that have an immune component to them, such as skin cancers.
For the past couple of years, those patients have experienced heightened anxiety because of the COVID-19 pandemic. Immune-suppressing medicine used to protect their new organ also makes it hard for patients to build immunity to foreign invaders like COVID-19.
A study appearing in the Proceedings of the National Academy of Sciences found the probability of a pandemic with similar impact to COVID-19 is about 2 percent in any year, and estimated that the probability of novel disease outbreaks will grow three-fold in the next few decades. All the more reason to identify an FDA-approved alternative to harsh immunosuppressive drugs.
Of the 18 patients during the phase II research trial who received the Talaris therapy, didn’t take immunosuppression medication and were vaccinated, only two ended up with a COVID infection, according to a review of the data. Among patients who needed to continue taking immunosuppressants or those who didn’t have them but were unvaccinated, the rates of infection were between 40 and 60 percent.
In the earlier phase II study by Talaris with 37 patients, the combined transplantation approach allowed 70 percent of patients to get off all immunosuppression.
“We’ve followed that whole cohort for more than six and a half years and one of them for 12 years from transplant, and every single patient that we got off immunosuppression has been able to stay off,” Requadt says.
That one patient, Robert Waddell, 55, was especially thankful to be weaned off immunosuppressive drugs approximately one year after his transplant procedure. The Louisville resident had long watched his mother, sister and other family members with polycystic kidney disease, or PKD, suffer the effects of chronic immunosuppression. That became his greatest fear when he was diagnosed with end stage renal failure.
Waddell enrolled in the phase II research taking place in Louisville after learning about it in early 2006. He chose to remain in the study when it relocated its clinical headquarters to Northwestern University’s medical center in Chicago a couple years later.
Before surgery, he underwent an enervating regimen of chemotherapy and radiation. It’s required to clear out a patient’s bone marrow cells so that they can be replaced by the donor’s cells. Waddell says the result was worth it: he had his combined kidney and immune system stem cell transplant in May 2009, without any need for chronic immunosuppression.
“I call it ‘short-term pain, long-term gain,’ because it was difficult to go through the conditioning, but after that, it was great,” he says. “I’ve talked to so many kidney recipients who say, ‘I wish I would have done that,’ because most people don’t think about clinical trials, but I was very fortunate.”
Waddell has every reason to support the success of this research, especially given the genetic disorder, PKD, that has plagued his family. One of his four children has PKD. He is anxious for the procedure to become standard of care, if and when his son needs it.

The Talaris procedure was pioneered decades ago by Suzanne Ildstad, founding CEO of Talaris and the company's Chief Scientific Officer, pictured here with the current CEO, Scott Requadt.
Talaris
“The beauty of this procedure is that I don’t have to take all of the anti-rejection drugs,” says Waddell, a finance professional. “I forget that I ever had any kidney issues. That’s how impactful it is.”
Talaris will continue to follow Waddell and the rest of his cohort to track the effectiveness and safety of the procedure. According to Requadt, the average life of a transplanted kidney is 12 to 15 years, partly because the immunosuppressive drugs worsen the functioning of the organ each year.
“We were the first group to show that we could robustly and fairly reproducibly do this in a clinical setting in humans,” Requadt says. “Most important, we’ve been able to show that we can still get a good engraftment of the stem cells from the donor, even if there is a profound…mismatch between the donor and the recipient’s immune systems.”
In kidney transplantation, it’s important to match for human leukocyte antigens (HLA) because there is a better graft survival in HLA-identical kidney transplants compared with HLA mismatched transplants.
About three months after the transplant, Talaris researchers look for evidence that the donated immune cells and stem cells have engrafted, while making a donor immune system for the patient. If more than 50 percent of the T cells contain the donor’s DNA after six months, patients can start taking fewer immunosuppressants.
“We know from phase II that in our patients who were able to tolerize [accept the organ without rejection] to their donated organ, we saw completely preserved and in fact slightly increased kidney function,” Requadt says. “So, it stands to reason that if you eliminate the drugs that are associated with declining kidney function that you would preserve kidney function, so hopefully the patient will have that one kidney for life.”
Matthew Cooper, director of kidney and pancreas transplantation for MedStar Georgetown Transplant Institute in Washington, DC, states that, “Right now, the Achilles’ heel is we have such a long waiting list and few donors that people die every day waiting for a kidney transplant. Eventually, we will eliminate the organ shortage so that people won’t die from organ failure.”
Cooper, a nationally recognized clinical transplant surgeon for 20 years, says when he started his career, finding a way for patients to forgo immunosuppression was considered “the Holy Grail” of modern transplant medicine.
“Now that we’ve got the protocols in place and some personal examples of how that can happen, it’s pretty exciting to see that all coming together,” he adds.
A robot server, controlled remotely by a disabled worker, delivers drinks to patrons at the DAWN cafe in Tokyo.
A sleek, four-foot tall white robot glides across a cafe storefront in Tokyo’s Nihonbashi district, holding a two-tiered serving tray full of tea sandwiches and pastries. The cafe’s patrons smile and say thanks as they take the tray—but it’s not the robot they’re thanking. Instead, the patrons are talking to the person controlling the robot—a restaurant employee who operates the avatar from the comfort of their home.
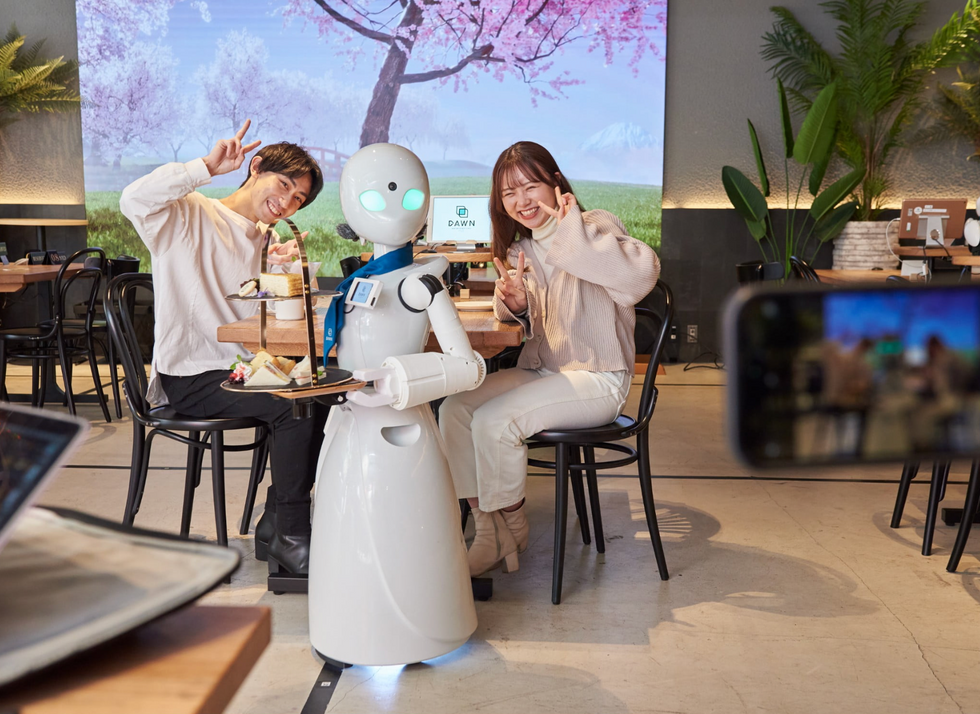
It’s a typical scene at DAWN, short for Diverse Avatar Working Network—a cafe that launched in Tokyo six years ago as an experimental pop-up and quickly became an overnight success. Today, the cafe is a permanent fixture in Nihonbashi, staffing roughly 60 remote workers who control the robots remotely and communicate to customers via a built-in microphone.
More than just a creative idea, however, DAWN is being hailed as a life-changing opportunity. The workers who control the robots remotely (known as “pilots”) all have disabilities that limit their ability to move around freely and travel outside their homes. Worldwide, an estimated 16 percent of the global population lives with a significant disability—and according to the World Health Organization, these disabilities give rise to other problems, such as exclusion from education, unemployment, and poverty.
These are all problems that Kentaro Yoshifuji, founder and CEO of Ory Laboratory, which supplies the robot servers at DAWN, is looking to correct. Yoshifuji, who was bedridden for several years in high school due to an undisclosed health problem, launched the company to help enable people who are house-bound or bedridden to more fully participate in society, as well as end the loneliness, isolation, and feelings of worthlessness that can sometimes go hand-in-hand with being disabled.
“It’s heartbreaking to think that [people with disabilities] feel they are a burden to society, or that they fear their families suffer by caring for them,” said Yoshifuji in an interview in 2020. “We are dedicating ourselves to providing workable, technology-based solutions. That is our purpose.”

Shota, Kuwahara, a DAWN employee with muscular dystrophy, agrees. "There are many difficulties in my daily life, but I believe my life has a purpose and is not being wasted," he says. "Being useful, able to help other people, even feeling needed by others, is so motivational."
A woman receives a mammogram, which can detect the presence of tumors in a patient's breast.
When a patient is diagnosed with early-stage breast cancer, having surgery to remove the tumor is considered the standard of care. But what happens when a patient can’t have surgery?
Whether it’s due to high blood pressure, advanced age, heart issues, or other reasons, some breast cancer patients don’t qualify for a lumpectomy—one of the most common treatment options for early-stage breast cancer. A lumpectomy surgically removes the tumor while keeping the patient’s breast intact, while a mastectomy removes the entire breast and nearby lymph nodes.
Fortunately, a new technique called cryoablation is now available for breast cancer patients who either aren’t candidates for surgery or don’t feel comfortable undergoing a surgical procedure. With cryoablation, doctors use an ultrasound or CT scan to locate any tumors inside the patient’s breast. They then insert small, needle-like probes into the patient's breast which create an “ice ball” that surrounds the tumor and kills the cancer cells.
Cryoablation has been used for decades to treat cancers of the kidneys and liver—but only in the past few years have doctors been able to use the procedure to treat breast cancer patients. And while clinical trials have shown that cryoablation works for tumors smaller than 1.5 centimeters, a recent clinical trial at Memorial Sloan Kettering Cancer Center in New York has shown that it can work for larger tumors, too.
In this study, doctors performed cryoablation on patients whose tumors were, on average, 2.5 centimeters. The cryoablation procedure lasted for about 30 minutes, and patients were able to go home on the same day following treatment. Doctors then followed up with the patients after 16 months. In the follow-up, doctors found the recurrence rate for tumors after using cryoablation was only 10 percent.
For patients who don’t qualify for surgery, radiation and hormonal therapy is typically used to treat tumors. However, said Yolanda Brice, M.D., an interventional radiologist at Memorial Sloan Kettering Cancer Center, “when treated with only radiation and hormonal therapy, the tumors will eventually return.” Cryotherapy, Brice said, could be a more effective way to treat cancer for patients who can’t have surgery.
“The fact that we only saw a 10 percent recurrence rate in our study is incredibly promising,” she said.

