Is It Possible to Predict Your Face, Voice, and Skin Color from Your DNA?
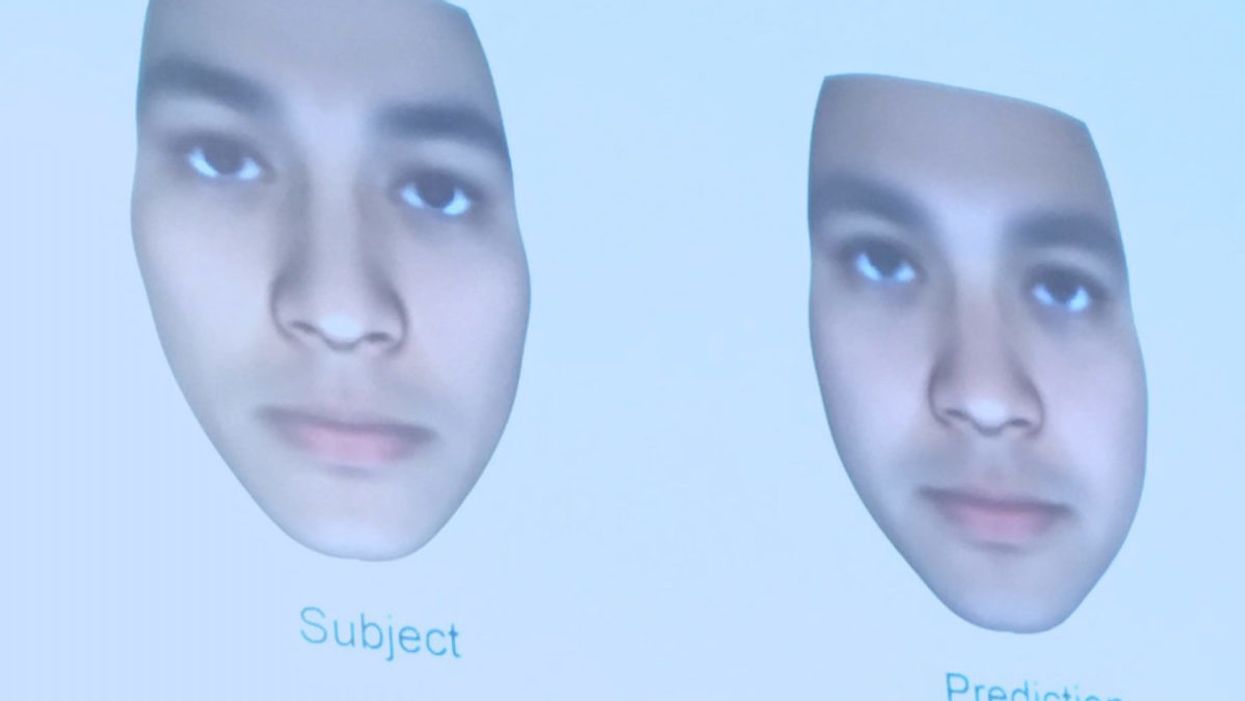
A slide from J. Craig Venter's recent study on facial prediction presented at the Summit Conference in Los Angeles on Nov. 3, 2017.
Renowned genetics pioneer Dr. J Craig Venter is no stranger to controversy.
Back in 2000, he famously raced the public Human Genome Project to decode all three billion letters of the human genome for the first time. A decade later, he ignited a new debate when his team created a bacterial cell with a synthesized genome.
Most recently, he's jumped back into the fray with a study in the September issue of the Proceedings of the National Academy of Sciences about the predictive potential of genomic data to identify individual traits such as voice, facial structure and skin color.
The new study raises significant questions about the privacy of genetic data.
His study applied whole-genome sequencing and statistical modeling to predict traits in 1,061 people of diverse ancestry. His approach aimed to reconstruct a person's physical characteristics based on DNA, and 74 percent of the time, his algorithm could correctly identify the individual in a random lineup of 10 people from his company's database.
While critics have been quick to cast doubt on the plausibility of his claims, the ability to discern people's observable traits, or phenotypes, from their genomes may grow more precise as technology improves, raising significant questions about the privacy and usage of genetic information in the long term.

J. Craig Venter showing slides from his recent study on facial prediction at the Summit Conference in Los Angeles on Nov. 3, 2017.
(Courtesy of Kira Peikoff)
Critics: Study Was Incomplete, Problematic
Before even redressing these potential legal and ethical considerations, some scientists simply said the study's main result was invalid. They pointed out that the methodology worked much better in distinguishing between people of different ethnicities than those of the same ethnicity. One of the most outspoken critics, Yaniv Erlich, a geneticist at Columbia University, said, "The method doesn't work. The results were like, 'If you have a lineup of ten people, you can predict eight."
Erlich, who reviewed Venter's paper for Science, where it was rejected, said that he came up with the same results—correctly predicting eight of ten people—by just looking at demographic factors such as age, gender and ethnicity. He added that Venter's recent rebuttal to his criticism was that 'Once we have thousands of phenotypes, it might work better.' But that, Erlich argued, would be "a major breach of privacy. Nobody has thousands of phenotypes for people."
Other critics suggested that the study's results discourage the sharing of genetic data, which is becoming increasingly important for medical research. They go one step further and imply that people's possible hesitation to share their genetic information in public databases may actually play into Venter's hands.
Venter's own company, Human Longevity Inc., aims to build the world's most comprehensive private database on human genotypes and phenotypes. The vastness of this information stands to improve the accuracy of whole genome and microbiome sequencing for individuals—analyses that come at a hefty price tag. Today, Human Longevity Inc. will sequence your genome and perform a battery of other health-related tests at an entry cost of $4900, going up to $25,000. Venter initially agreed to comment for this article, but then could not be reached.
"The bigger issue is how do we understand and use genetic information and avoid harming people."
Opens Up Pandora's Box of Ethical Issues
Whether Venter's study is valid may not be as important as the Pandora's box of potential ethical and legal issues that it raises for future consideration. "I think this story is one along a continuum of stories we've had on the issue of identifiability based on genomic information in the past decade," said Amy McGuire, a biomedical ethics professor at Baylor College of Medicine. "It does raise really interesting and important questions about privacy, and socially, how we respond to these types of scientific advancements. A lot of our focus from a policy and ethics perspective is to protect privacy."
McGuire, who is also the Director of the Center for Medical Ethics and Health Policy at Baylor, added that while protecting privacy is very important, "the bigger issue is how do we understand and use genetic information and avoid harming people." While we've taken "baby steps," she said, towards enacting laws in the U.S. that fight genetic determinism—such as the Genetic Information and Nondiscrimination Act, which prohibits discrimination based on genetic information in health insurance and employment—some areas remain unprotected, such as for life insurance and disability.

J. Craig Venter showing slides from his recent study on facial prediction at the Summit Conference in Los Angeles on Nov. 3, 2017.
(Courtesy of Kira Peikoff)
Physical reconstructions like those in Venter's study could also be inappropriately used by law enforcement, said Leslie Francis, a law and philosophy professor at the University of Utah, who has written about the ethical and legal issues related to sharing genomic data.
"If [Venter's] findings, or findings like them, hold up, the implications would be significant," Francis said. Law enforcement is increasingly using DNA identification from genetic material left at crime scenes to weed out innocent and guilty suspects, she explained. This adds another potentially complicating layer.
"There is a shift here, from using DNA sequencing techniques to match other DNA samples—as when semen obtained from a rape victim is then matched (or not) with a cheek swab from a suspect—to using DNA sequencing results to predict observable characteristics," Francis said. She added that while the former necessitates having an actual DNA sample for a match, the latter can use DNA to pre-emptively (and perhaps inaccurately) narrow down suspects.
"My worry is that if this [the study's methodology] turns out to be sort-of accurate, people will think it is better than what it is," said Francis. "If law enforcement comes to rely on it, there will be a host of false positives and false negatives. And we'll face new questions, [such as] 'Which is worse? Picking an innocent as guilty, or failing to identify someone who is guilty?'"
Risking Privacy Involves a Tradeoff
When people voluntarily risk their own privacy, that involves a tradeoff, McGuire said. A 2014 study that she conducted among people who were very sick, or whose children were very sick, found that more than half were willing to share their health information, despite concerns about privacy, because they saw a big benefit in advancing research on their conditions.
"We've focused a lot of our policy attention on restricting access, but we don't have a system of accountability when there's a breach."
"To make leaps and bounds in medicine and genomics, we need to create a database of millions of people signing on to share their genetic and health information in order to improve research and clinical care," McGuire said. "They are going to risk their privacy, and we have a social obligation to protect them."
That also means "punishing bad actors," she continued. "We've focused a lot of our policy attention on restricting access, but we don't have a system of accountability when there's a breach."
Even though most people using genetic information have good intentions, the consequences if not are troubling. "All you need is one bad actor who decimates the trust in the system, and it has catastrophic consequences," she warned. That hasn't happened on a massive scale yet, and even if it did, some experts argue that obtaining the data is not the real risk; what is more concerning is hacking individuals' genetic information to be used against them, such as to prove someone is unfit for a particular job because of a genetic condition like Alzheimer's, or that a parent is unfit for custody because of a genetic disposition to mental illness.
Venter, in fact, told an audience at the recent Summit conference in Los Angeles that his new study's approach could not only predict someone's physical appearance from their DNA, but also some of their psychological traits, such as the propensity for an addictive personality. In the future, he said, it will be possible to predict even more about mental health from the genome.
What is most at risk on a massive scale, however, is not so much genetic information as demographic identifiers included in medical records, such as birth dates and social security numbers, said Francis, the law and philosophy professor. "The much more interesting and lucrative security breaches typically involve not people interested in genetic information per se, but people interested in the information in health records that you can't change."
Hospitals have been hacked for this kind of information, including an incident at the Veterans Administration in 2006, in which the laptop and external hard drive of an agency employee that contained unencrypted information on 26.5 million patients were stolen from the employee's house.
So, what can people do to protect themselves? "Don't share anything you wouldn't want the world to see," Francis said. "And don't click 'I agree' without actually reading privacy policies or terms and conditions. They may surprise you."
Breakthrough therapies are breaking patients' banks. Key changes could improve access, experts say.
Single-treatment therapies are revolutionizing medicine. But insurers and patients wonder whether they can afford treatment and, if they can, whether the high costs are worthwhile.
CSL Behring’s new gene therapy for hemophilia, Hemgenix, costs $3.5 million for one treatment, but helps the body create substances that allow blood to clot. It appears to be a cure, eliminating the need for other treatments for many years at least.
Likewise, Novartis’s Kymriah mobilizes the body’s immune system to fight B-cell lymphoma, but at a cost $475,000. For patients who respond, it seems to offer years of life without the cancer progressing.
These single-treatment therapies are at the forefront of a new, bold era of medicine. Unfortunately, they also come with new, bold prices that leave insurers and patients wondering whether they can afford treatment and, if they can, whether the high costs are worthwhile.
“Most pharmaceutical leaders are there to improve and save people’s lives,” says Jeremy Levin, chairman and CEO of Ovid Therapeutics, and immediate past chairman of the Biotechnology Innovation Organization. If the therapeutics they develop are too expensive for payers to authorize, patients aren’t helped.
“The right to receive care and the right of pharmaceuticals developers to profit should never be at odds,” Levin stresses. And yet, sometimes they are.
Leigh Turner, executive director of the bioethics program, University of California, Irvine, notes this same tension between drug developers that are “seeking to maximize profits by charging as much as the market will bear for cell and gene therapy products and other medical interventions, and payers trying to control costs while also attempting to provide access to medical products with promising safety and efficacy profiles.”
Why Payers Balk
Health insurers can become skittish around extremely high prices, yet these therapies often accompany significant overall savings. For perspective, the estimated annual treatment cost for hemophilia exceeds $300,000. With Hemgenix, payers would break even after about 12 years.
But, in 12 years, will the patient still have that insurer? Therein lies the rub. U.S. payers, are used to a “pay-as-you-go” model, in which the lifetime costs of therapies typically are shared by multiple payers over many years, as patients change jobs. Single treatment therapeutics eliminate that cost-sharing ability.
"As long as formularies are based on profits to middlemen…Americans’ healthcare costs will continue to skyrocket,” says Patricia Goldsmith, the CEO of CancerCare.
“There is a phenomenally complex, bureaucratic reimbursement system that has grown, layer upon layer, during several decades,” Levin says. As medicine has innovated, payment systems haven’t kept up.
Therefore, biopharma companies begin working with insurance companies and their pharmacy benefit managers (PBMs), which act on an insurer’s behalf to decide which drugs to cover and by how much, early in the drug approval process. Their goal is to make sophisticated new drugs available while still earning a return on their investment.
New Payment Models
Pay-for-performance is one increasingly popular strategy, Turner says. “These models typically link payments to evidence generation and clinically significant outcomes.”
A biotech company called bluebird bio, for example, offers value-based pricing for Zynteglo, a $2.8 million possible cure for the rare blood disorder known as beta thalassaemia. It generally eliminates patients’ need for blood transfusions. The company is so sure it works that it will refund 80 percent of the cost of the therapy if patients need blood transfusions related to that condition within five years of being treated with Zynteglo.
In his February 2023 State of the Union speech, President Biden proposed three pilot programs to reduce drug costs. One of them, the Cell and Gene Therapy Access Model calls on the federal Centers for Medicare & Medicaid Services to establish outcomes-based agreements with manufacturers for certain cell and gene therapies.
A mortgage-style payment system is another, albeit rare, approach. Amortized payments spread the cost of treatments over decades, and let people change employers without losing their healthcare benefits.
Only about 14 percent of all drugs that enter clinical trials are approved by the FDA. Pharma companies, therefore, have an exigent need to earn a profit.
The new payment models that are being discussed aren’t solutions to high prices, says Bill Kramer, senior advisor for health policy at Purchaser Business Group on Health (PBGH), a nonprofit that seeks to lower health care costs. He points out that innovative pricing models, although well-intended, may distract from the real problem of high prices. They are attempts to “soften the blow. The best thing would be to charge a reasonable price to begin with,” he says.
Instead, he proposes making better use of research on cost and clinical effectiveness. The Institute for Clinical and Economic Review (ICER) conducts such research in the U.S., determining whether the benefits of specific drugs justify their proposed prices. ICER is an independent non-profit research institute. Its reports typically assess the degrees of improvement new therapies offer and suggest prices that would reflect that. “Publicizing that data is very important,” Kramer says. “Their results aren’t used to the extent they could and should be.” Pharmaceutical companies tend to price their therapies higher than ICER’s recommendations.
Drug Development Costs Soar
Drug developers have long pointed to the onerous costs of drug development as a reason for high prices.
A 2020 study found the average cost to bring a drug to market exceeded $1.1 billion, while other studies have estimated overall costs as high as $2.6 billion. The development timeframe is about 10 years. That’s because modern therapeutics target precise mechanisms to create better outcomes, but also have high failure rates. Only about 14 percent of all drugs that enter clinical trials are approved by the FDA. Pharma companies, therefore, have an exigent need to earn a profit.
Skewed Incentives Increase Costs
Pricing isn’t solely at the discretion of pharma companies, though. “What patients end up paying has much more to do with their PBMs than the actual price of the drug,” Patricia Goldsmith, CEO, CancerCare, says. Transparency is vital.
PBMs control patients’ access to therapies at three levels, through price negotiations, pricing tiers and pharmacy management.
When negotiating with drug manufacturers, Goldsmith says, “PBMs exchange a preferred spot on a formulary (the insurer’s or healthcare provider’s list of acceptable drugs) for cash-base rebates.” Unfortunately, 25 percent of the time, those rebates are not passed to insurers, according to the PBGH report.
Then, PBMs use pricing tiers to steer patients and physicians to certain drugs. For example, Kramer says, “Sometimes PBMs put a high-cost brand name drug in a preferred tier and a lower-cost competitor in a less preferred, higher-cost tier.” As the PBGH report elaborates, “(PBMs) are incentivized to include the highest-priced drugs…since both manufacturing rebates, as well as the administrative fees they charge…are calculated as a percentage of the drug’s price.
Finally, by steering patients to certain pharmacies, PBMs coordinate patients’ access to treatments, control patients’ out-of-pocket costs and receive management fees from the pharmacies.
Therefore, Goldsmith says, “As long as formularies are based on profits to middlemen…Americans’ healthcare costs will continue to skyrocket.”
Transparency into drug pricing will help curb costs, as will new payment strategies. What will make the most impact, however, may well be the development of a new reimbursement system designed to handle dramatic, breakthrough drugs. As Kramer says, “We need a better system to identify drugs that offer dramatic improvements in clinical care.”
In today's podcast episode, law professor Gaia Bernstein talks about the challenges of keeping control over our thoughts and actions, even when some powerful forces are pushing in the other direction.
Each afternoon, kids walk through my neighborhood, on their way back home from school, and almost all of them are walking alone, staring down at their phones. It's a troubling site. This daily parade of the zombie children just can’t bode well for the future.
That’s one reason I felt like Gaia Bernstein’s new book was talking directly to me. A law professor at Seton Hall, Gaia makes a strong argument that people are so addicted to tech at this point, we need some big, system level changes to social media platforms and other addictive technologies, instead of just blaming the individual and expecting them to fix these issues.
Gaia’s book is called Unwired: Gaining Control Over Addictive Technologies. It’s fascinating and I had a chance to talk with her about it for today’s podcast. At its heart, our conversation is really about how and whether we can maintain control over our thoughts and actions, even when some powerful forces are pushing in the other direction.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
We discuss the idea that, in certain situations, maybe it's not reasonable to expect that we’ll be able to enjoy personal freedom and autonomy. We also talk about how to be a good parent when it sometimes seems like our kids prefer to be raised by their iPads; so-called educational video games that actually don’t have anything to do with education; the root causes of tech addictions for people of all ages; and what kinds of changes we should be supporting.
Gaia is Seton’s Hall’s Technology, Privacy and Policy Professor of Law, as well as Co-Director of the Institute for Privacy Protection, and Co-Director of the Gibbons Institute of Law Science and Technology. She’s the founding director of the Institute for Privacy Protection. She created and spearheaded the Institute’s nationally recognized Outreach Program, which educated parents and students about technology overuse and privacy.
Professor Bernstein's scholarship has been published in leading law reviews including the law reviews of Vanderbilt, Boston College, Boston University, and U.C. Davis. Her work has been selected to the Stanford-Yale Junior Faculty Forum and received extensive media coverage. Gaia joined Seton Hall's faculty in 2004. Before that, she was a fellow at the Engelberg Center of Innovation Law & Policy and at the Information Law Institute of the New York University School of Law. She holds a J.S.D. from the New York University School of Law, an LL.M. from Harvard Law School, and a J.D. from Boston University.
Gaia’s work on this topic is groundbreaking I hope you’ll listen to the conversation and then consider pre-ordering her new book. It comes out on March 28.


