New Tests Measure Your Body’s Biological Age, Offering a Glimpse into the Future of Health Care
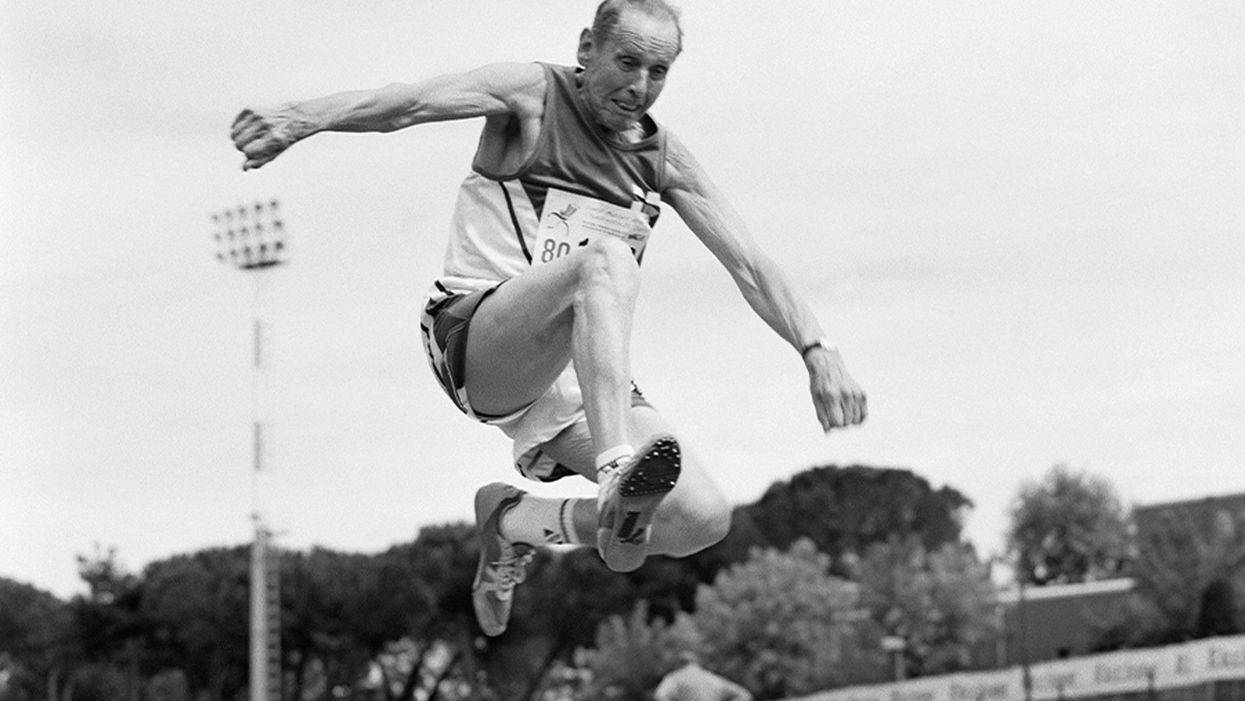
A senior long jumper competes in the 80-84-year-old age division at the 2007 World Masters Championships Stadia (track and field competition) at Riccione Stadium in Riccione, Italy on September 6, 2007. From the book project Racing Age.
What if a simple blood test revealed how fast you're aging, and this meant more to you and your insurance company than the number of candles on your birthday cake?
The question of why individuals thrive or decline has loomed large in 2020, with COVID-19 harming people of all ages, while leaving others asymptomatic. Meanwhile, scientists have produced new measures, called aging clocks, that attempt to predict mortality and may eventually affect how we perceive aging.
Take, for example, "senior" athletes who perform more like 50-year-olds. But people over 65 are lumped into one category, whether they are winning marathons or using a walker. Meanwhile, I'm entering "middle age," a label just as vague. It's frustrating to have a better grasp on the lifecycle of my phone than my own body.
That could change soon, due to clock technology. In 2013, UCLA biostatistician Steven Horvath took a new approach to an old carnival trick, guessing people's ages by looking at epigenetics: how chemical compounds in our cells turn genetic instructions on or off. Exercise, pollutants, and other aspects of lifestyle and environment can flip these switches, converting a skin cell into a hair cell, for example. Then, hair may sprout from your ears.
Horvath's epigenetic clock approximated age within just a few years; an above-average estimate suggested fast aging. This "basically changed everything," said Vadim Gladyshev, a Harvard geneticist, leading to more epigenetic clocks and, just since May, additional clocks of the heart, products of cell metabolism, and microbes in a person's mouth and gut.
Machine learning is fueling these discoveries. Scientists send algorithms hunting through jungles of health data for factors related to physical demise. "Nothing in [the aging] industry has progressed as much as biomarkers," said Alex Zhavoronkov, CEO of Deep Longevity, a pioneer in learning-based clocks.
Researchers told LeapsMag that this tech could help identify age-related vulnerabilities to diseases—including COVID-19—and protective drugs.
Clocking disease vulnerability
In July, Yale researcher Morgan Levine found people were more likely to be hospitalized and die from COVID-19 if their aging clocks were ticking ahead of their calendar years. This effect held regardless of pre-existing conditions.
The study used Levine's biological aging clock, called PhenoAge, which is more accurate than previous versions. To develop it, she looked at data on health indices over several decades, focusing on nine hallmarks of aging—such as inflammation—that correspond to when people die. Then she used AI to find which epigenetic patterns in blood samples were strongly associated with physical aging. The PhenoAge clock reads these patterns to predict biological age; mortality goes up 62 percent among the fastest agers.
The cocktail, aimed at restoring immune function, reversed age by an average of 2.5 years, according to an epigenetic clock measurement taken before and after the intervention.
Because PhenoAge links chronic inflammation to aging and vulnerability, Levine proposed treating "inflammaging" to counter COVID-19.
Gladyshev reported similar findings, and Nir Barzilai, director of the Institute of Aging Research at Albert Einstein College of Medicine, agreed that biological age deserves greater focus. PhenoAge is an important innovation, he said, but most precise when measuring average age across large populations. Until clocks—including his blood protein version—account for differences in how individuals age, "Multi-morbidity is really the major biomarker" for a given person. Barzilai thinks individuals over 65 with two or more diseases are biologically older than their chronological age—about half the population in this study.
He believes COVID-19 efforts aren't taking stock of these differences. "The scientists are living in silos," he said, with many unaware aging has a biology that can be targeted.
The missed opportunities could be profound, especially for lower-income communities with disproportionately advanced aging. Barzilai has read eight different observational studies finding decreased COVID-19 severity among people taking metformin, the diabetes drug, which is believed to slow down the major hallmarks of biological aging, such as inflammation. Once a vaccine is identified, biologically older people could supplement it with metformin, but the medical establishment requires lengthy clinical trials. "The conservatism is taking over in days of war," Barzilai said.
Drug benefits on time
Clocks, once validated, could gauge drug effectiveness against age-related diseases quicker and cheaper than trials that track health outcomes over many years, expediting FDA approval of such therapies. For this to happen, though, the FDA must see evidence that rewinding clocks or improving related biomarkers leads to clinical benefits for patients. Researchers believe that clinical applications for at least some of these clocks are five to 10 years away.
Progress was made in last year's TRIIM trial, run by immunologist Gregory Fahy at Stanford Medical Center. People in their 50s took growth hormone, metformin and another diabetes drug, dehydroepiandrosterone, for 12 months. The cocktail, aimed at restoring immune function, reversed age by an average of 2.5 years, according to an epigenetic clock measurement taken before and after the intervention. Don't quit your gym just yet; TRIIM included just nine Caucasian men. A follow-up with 85 diverse participants begins next month.
But even group averages of epigenetic measures can be questionable, explained Willard Freeman, a researcher with the Reynolds Oklahoma Center on Aging. Consider this odd finding: heroin addicts tend to have younger epigenetic ages. "With the exception of Keith Richards, I don't think heroin is a great way to live a long healthy life," Freeman said.
Such confounders reveal that scientists—and AI—are still struggling to unearth the roots of aging. Do clocks simply reflect damage, mirrors to show who's the frailest of them all? Or do they programmatically drive aging? The answer involves vast complexity, like trying to deduce the direct causes of a 17-car pileup on a potholed road in foggy conditions. Except, instead of 17 cars, it's millions of epigenetic sites and thousands of potential genes, RNA molecules and blood proteins acting on aging and each other.
Because the various measures—epigenetics, microbes, etc.—capture distinct aging dimensions, an important goal is unifying them into one "mosaic of biological ages," as Levine called it. Gladyshev said more datasets are needed. Just yesterday, though, Zhavoronkov launched Deep Longevity's groundbreaking composite of metrics to consumers – something that was previously available only to clinicians. The iPhone app allows users to upload their own samples and tracks aging on multiple levels – epigenetic, behavioral, microbiome, and more. It even includes a deep psychological clock asking if people feel as old as they are. Perhaps Twain's adage about mind over matter is evidence-backed.
Zhavoronkov appeared youthful in our Zoom interview, but admitted self-testing shows an advanced age because "I do not sleep"; indeed, he'd scheduled me at midnight Hong Kong time. Perhaps explaining his insomnia, he fears economic collapse if age-related diseases cost the global economy over $30 trillion by 2030. Rather than seeking eternal life, researchers like Zhavoronkov aim to increase health span: fully living our final decades without excess pain and hospital bills.
It's also a lucrative sales pitch to 7.8 billion aging humans.
Get your bio age
Levine, the Yale scientist, has partnered with Elysium Health to sell Index, an epigenetic measure launched in late 2019, direct to consumers, using their saliva samples. Elysium will roll out additional measures as research progresses, starting with an assessment of how fast someone is accumulating cells that no longer divide. "The more measures to capture specific processes, the more we can actually understand what's unique for an individual," Levine said.
Another company, InsideTracker, with an advisory board headlined by Harvard's David Sinclair, eschews the quirkiness of epigenetics. Its new InnerAge 2.0 test, announced this month, analyzes 18 blood biomarkers associated with longevity.
"You can imagine payers clamoring to charge people for costs with a kind of personal responsibility to them."
Because aging isn't considered a disease, consumer aging tests don't require FDA approval, and some researchers are skeptical of their use in the near future. "I'm on the fence as to whether these things are ready to be rolled out," said Freeman, the Oklahoma researcher. "We need to do our traditional experimental study design to [be] confident they're actually useful."
Then, 50-year-olds who are biologically 45 may wait five years for their first colonoscopy, Barzilai said. Despite some forerunners, clinical applications for individuals are mostly prospective, yet I was intrigued. Could these clocks reveal if I'm following the footsteps of the super-agers? Or will I rack up the hospital bills of Zhavoronkov's nightmares?
I sent my blood for testing with InsideTracker. Fearing the worst—an InnerAge accelerated by a couple of decades—I asked thought leaders where this technology is headed.
Insurance 2030
With continued advances, by 2030 you'll learn your biological age with a glance at your wristwatch. You won't be the only monitor; your insurance company may send an alert if your age goes too high, threatening lost rewards.
If this seems implausible, consider that life insurer John Hancock already tracks a VitalityAge. With Obamacare incentivizing companies to engage policyholders in improving health, many are dangling rewards for fitness. BlueCross BlueShield covers 25 percent of InsideTracker's cost, and UnitedHealthcare offers a suite of such programs, including "missions" for policyholders to lower their Rally age. "People underestimate the amount of time they're sedentary," said Michael Bess, vice president of healthcare strategies. "So having this technology to drive positive reinforcement is just another way to encourage healthy behavior."
It's unclear if these programs will close health gaps, or simply attract customers already prioritizing fitness. And insurers could raise your premium if you don't measure up. Obamacare forbids discrimination based on pre-existing conditions, but will accelerated age qualify for this protection?
Liz McFall, a sociologist at the University of Edinburgh, thinks the answer depends on whether we view aging as controllable. "You can imagine payers clamoring to charge people for costs with a kind of personal responsibility to them," she said.
That outcome troubles Mark Rothstein, director of the Institute of Bioethics at the University of Louisville. "For those living with air pollution and unsafe water, in food deserts and where you can't safely exercise, then [insurers] take the results in terms of biological stressors, now you're adding insult to injury," he said.
Government could subsidize aging clocks and interventions for older people with fewer resources for controlling their health—and the greatest room for improving their epigenetic age. Rothstein supports that policy, but said, "I don't see it happening."
Bio age working for you
2030 again. A job posting seeks a "go-getter," so you attach a doctor's note to your resume proving you're ten years younger than your chronological age.
This prospect intrigued Cathy Ventrell-Monsees, senior advisor at the Equal Employment Opportunity Commission. "Any marker other than age is a step forward," she said. "Age simply doesn't determine any kind of cognitive or physical ability."
What if the assessment isn't voluntary? Armed with AI, future employers could surveil a candidate's biological age from their head-shot. Haut.ai is already marketing an uncannily accurate PhotoAgeClock. Its CEO, Anastasia Georgievskaya, noted this tech's promise in other contexts; it could help people literally see the connection between healthier lifestyles and looking young and attractive. "The images keep people quite engaged," she told me.
Updating laws could minimize drawbacks. Employers are already prohibited from using genetic information to discriminate (think 23andMe). The ban could be extended to epigenetics. "I would imagine biomarkers for aging go a similar path as genetic nondiscrimination," said McFall, the sociologist.
Will we use aging clocks to screen candidates for the highest office? Barzilai, the Albert Einstein College of Medicine researcher, believes Trump and Biden have similar biological ages. But one of Barzilai's factors, BMI, is warped by Trump miraculously getting taller. "Usually people get shorter with age," Barzilai said. "His weight has been increasing, but his BMI stays the same."
As for my bio age? InnerAge suggested I'm four years younger—and by boosting my iron levels, the program suggests, I could be younger still.
We need standards for these tests, and customers must understand their shortcomings. With such transparency, though, the benefits could be compelling. In March, Theresa Brown, a 44-year-old from Kansas, learned her InnerAge was 57.2. She followed InsideTracker's recommendations, including regular intermittent fasting. Retested five months later, her age had dropped to 34.1. "It's not that I guaranteed another 10 or 20 years to my life. It's that it encourages me. Whether I really am or not, I just feel younger. I'll take that."
Which leads back to Zhavoronkov's psychological clock. Perhaps lowering our InnerAges can be the self-fulfilling prophesy that helps Theresa and me age like the super-athletes who thrive longer than expected. McFall noted the power of simple, sufficiently credible goals for encouraging better health. Think 10,000 steps per day, she said.
Want to be 34 again? Just do it.
Yet, many people's budgets just don't allow gym memberships, nutritious groceries, or futuristic aging clocks. Bill Gates cautioned we overestimate progress in the next two years, while underestimating the next ten. Policies should ensure that age testing and interventions are distributed fairly.
"Within the next 5 to 10 years," said Gladyshev, "there will be drugs and lifestyle changes which could actually increase lifespan or healthspan for the entire population."
Opioid prescription policies may hurt those in chronic pain
Guidelines aim to prevent opioid-related deaths by making it more challenging to get prescriptions, but they can also block access for those who desperately need them.
Tinu Abayomi-Paul works as a writer and activist, plus one unwanted job: Trying to fill her opioid prescription. She says that some pharmacists laugh and tell her that no one needs the amount of pain medication that she is seeking. Another pharmacist near her home in Venus, Tex., refused to fill more than seven days of a 30-day prescription.
To get a new prescription—partially filled opioid prescriptions can’t be dispensed later—Abayomi-Paul needed to return to her doctor’s office. But without her medication, she was having too much pain to travel there, much less return to the pharmacy. She rationed out the pills over several weeks, an agonizing compromise that left her unable to work, interact with her children, sleep restfully, or leave the house. “Don’t I deserve to do more than survive?” she says.
Abayomi-Paul’s pain results from a degenerative spine disorder, chronic lymphocytic leukemia, and more than a dozen other diagnoses and disabilities. She is part of a growing group of people with chronic pain who have been negatively impacted by the fallout from efforts to prevent opioid overdose deaths.
Guidelines for dispensing these pills are complicated because many opioids, like codeine, oxycodone, and morphine, are prescribed legally for pain. Yet, deaths from opioids have increased rapidly since 1999 and become a national emergency. Many of them, such as heroin, are used illegally. The CDC identified three surges in opioid use: an increase in opioid prescriptions in the ‘90s, a surge of heroin around 2010, and an influx of fentanyl and other powerful synthetic opioids in 2013.
As overdose deaths grew, so did public calls to address them, prompting the CDC to change its prescription guidelines in 2016. The new guidelines suggested limiting medication for acute pain to a seven-day supply, capping daily doses of morphine, and other restrictions. Some statistics suggest that these policies have worked; from 2016 to 2019, prescriptions for opiates fell 44 percent. Physicians also started progressively lowering opioid doses for patients, a practice called tapering. A study tracking nearly 100,000 Medicare subscribers on opioids found that about 13 percent of patients were tapering in 2012, and that number increased to about 23 percent by 2017.
But some physicians may be too aggressive with this tapering strategy. About one in four people had doses reduced by more than 10 percent per week, a rate faster than the CDC recommends. The approach left people like Abayomi-Paul without the medication they needed. Every year, Abayomi-Paul says, her prescriptions are harder to fill. David Brushwood, a pharmacy professor who specializes in policy and outcomes at the University of Florida in Gainesville, says opioid dosing isn’t one-size-fits-all. “Patients need to be taken care of individually, not based on what some government agency says they need,” he says.
‘This is not survivable’
Health policy and disability rights attorney Erin Gilmer advocated for people with pain, using her own experience with chronic pain and a host of medical conditions as a guidepost. She launched an advocacy website, Healthcare as a Human Right, and shared her struggles on Twitter: “This pain is more than anything I've endured before and I've already been through too much. Yet because it's not simply identified no one believes it's as bad as it is. This is not survivable.”
When her pain dramatically worsened midway through 2021, Gilmer’s posts grew ominous: “I keep thinking it can't possibly get worse but somehow every day is worse than the last.”
The CDC revised its guidelines in 2022 after criticisms that people with chronic pain were being undertreated, enduring dangerous withdrawal symptoms, and suffering psychological distress. (Long-term opioid use can cause physical dependency, an adaptive reaction that is different than the compulsive misuse associated with a substance use disorder.) It was too late for Gilmer. On July 7, 2021, the 38-year-old died by suicide.
Last August, an Ohio district court ruling set forth a new requirement for Walgreens, Walmart, and CVS pharmacists in two counties. These pharmacists must now document opioid prescriptions that are turned down, even for customers who have no previous purchases at that pharmacy, and they’re required to share this information with other locations in the same chain. None of the three pharmacies responded to an interview request from Leaps.org.
In a practice called red flagging, pharmacists may label a prescription suspicious for a variety of reasons, such as if a pharmacist observes an unusually high dose, a long distance from the patient’s home to the pharmacy, or cash payment. Pharmacists may question patients or prescribers to resolve red flags but, regardless of the explanation, they’re free to refuse to fill a prescription.
As the risk of litigation has grown, so has finger-pointing, says Seth Whitelaw, a compliance consultant at Whitelaw Compliance Group in West Chester, PA, who advises drug, medical device, and biotech companies. Drugmakers accused in National Prescription Opioid Litigation (NPOL), a complex set of thousands of cases on opioid epidemic deaths, which includes the Ohio district case, have argued that they shouldn’t be responsible for the large supply of opiates and overdose deaths. Yet, prosecutors alleged that these pharmaceutical companies hid addiction and overdose risks when labeling opioids, while distributors and pharmacists failed to identify suspicious orders or scripts.
Patients and pharmacists fear red flags
The requirements that pharmacists document prescriptions they refuse to fill so far only apply to two counties in Ohio. But Brushwood fears they will spread because of this precedent, and because there’s no way for pharmacists to predict what new legislation is on the way. “There is no definition of a red flag, there are no lists of red flags. There is no instruction on what to do when a red flag is detected. There’s no guidance on how to document red flags. It is a standardless responsibility,” Brushwood says. This adds trepidation for pharmacists—and more hoops to jump through for patients.
“I went into the doctor one day here and she said, ‘I'm going to stop prescribing opioids to all my patients effective immediately,” Nicolson says.
“We now have about a dozen studies that show that actually ripping somebody off their medication increases their risk of overdose and suicide by three to five times, destabilizes their health and mental health, often requires some hospitalization or emergency care, and can cause heart attacks,” says Kate Nicolson, founder of the National Pain Advocacy Center based in Boulder, Colorado. “It can kill people.” Nicolson was in pain for decades due to a surgical injury to the nerves leading to her spinal cord before surgeries fixed the problem.
Another issue is that primary care offices may view opioid use as a reason to turn down new patients. In a 2021 study, secret shoppers called primary care clinics in nine states, identifying themselves as long-term opioid users. When callers said their opioids were discontinued because their former physician retired, as opposed to an unspecified reason, they were more likely to be offered an appointment. Even so, more than 40 percent were refused an appointment. The study authors say their findings suggest that some physicians may try to avoid treating people who use opioids.
Abayomi-Paul says red flagging has changed how she fills prescriptions. “Once I go to one place, I try to [continue] going to that same place because of the amount of records that I have and making sure my medications don’t conflict,” Abayomi-Paul says.
Nicolson moved to Colorado from Washington D.C. in 2015, before the CDC issued its 2016 guidelines. When the guidelines came out, she found the change to be shockingly abrupt. “I went into the doctor one day here and she said, ‘I'm going to stop prescribing opioids to all my patients effective immediately.’” Since then, she’s spoken with dozens of patients who have been red-flagged or simply haven’t been able to access pain medication.
Despite her expertise, Nicolson isn’t positive she could successfully fill an opioid prescription today even if she needed one. At this point, she’s not sure exactly what various pharmacies would view as a red flag. And she’s not confident that these red flags even work. “You can have very legitimate reasons for being 50 miles away or having to go to multiple pharmacies, given that there are drug shortages now, as well as someone refusing to fill [a prescription.] It doesn't mean that you’re necessarily ‘drug seeking.’”
While there’s no easy solution. Whitelaw says clarifying the role of pharmacists and physicians in patient access to opioids could help people get the medication they need. He is seeking policy changes that focus on the needs of people in pain more than the number of prescriptions filled. He also advocates standardizing the definition of red flags and procedures for resolving them. Still, there will never be a single policy that can be applied to all people, explains Brushwood, the University of Florida professor. “You have to make a decision about each individual prescription.”
Recent immigration restrictions have left many foreign researchers' projects and careers in limbo—and some in jeopardy.
This article is part of the magazine, "The Future of Science In America: The Election Issue," co-published by LeapsMag, the Aspen Institute Science & Society Program, and GOOD.
When COVID-19 cases were surging in New York City in early spring, Chitra Mohan, a postdoctoral fellow at Weill Cornell, was overwhelmed with worry. But the pandemic was only part of her anxieties. Having come to the United States from India on a student visa that allowed her to work for a year after completing her degree, she had applied for a two-year extension, typically granted for those in STEM fields. But due to a clerical error—Mohan used an electronic signatureinstead of a handwritten one— her application was denied and she could no longerwork in the United States.
"I was put on unpaid leave and I lost my apartment and my health insurance—and that was in the middle of COVID!" she says.
Meanwhile her skills were very much needed in those unprecedented times. A molecular biologist studying how DNA can repair itself, Mohan was trained in reverse transcription polymerase chain reaction or RT-PCR—a lab technique that detects pathogens and is used to diagnose COVID-19. Mohan wanted to volunteer at testing centers, but because she couldn't legally work in the U.S., she wasn't allowed to help either. She moved to her cousin's house, hired a lawyer, and tried to restore her work status.
"I spent about $4,000 on lawyer fees and another $1,200 to pay for the motions I filed," she recalls. "I had to borrow money from my parents and my cousin because without my salary I just didn't have the $7,000 at hand." But the already narrow window of opportunity slammed completely shut when the Trump administration suspended issuing new visas for foreign researchers in June. All Mohan's attempts were denied. In August, she had to leave the country. "Given the recent work visa ban by the administration, all my options in the U.S. are closed," she wrote a bitter note on Twitter. "I have to uproot my entire life in NY for the past 6 years and leave." She eventually found a temporary position in Calcutta, where she can continue research.
Mohan is hardly alone in her visa saga. Many foreign scholars on H- and J-type visas and other permits that let them remain employed in America had been struggling to keep their rights to continue research, which in certain cases is crucial to battling the pandemic. Some had to leave the country, some filed every possible extension to buy time, and others are stuck in their home countries, unable to return. The already cumbersome process of applying for visas and extensions became crippled during the lockdowns. But in June, when President Trump extended and expanded immigration restrictions to cut the number of immigrant workers entering the U.S., the new limits left researchers' projects and careers in limbo—and some in jeopardy.
"We have been a beneficiary of this flow of human capacity and resource investment for many generations—and this is now threatened."
Rakesh Ramachandran, whose computational biology work contributed to one of the first coronavirus studies to map out its protein structures—is stranded in India. In early March, he had travelled there to attend a conference and visit the American consulate to stamp his H1 visa for a renewal, already granted. The pandemic shut down both the conference and the consulates, and Ramachandran hasn't been able to come back since. The consulates finally opened in September, but so far the online portal has no available appointment slots. "I'm told to keep trying," Ramachandran says.
The visa restrictions affected researchers worldwide, regardless of disciplines or countries. A Ph.D. student in neuroscience, Morgane Leroux had to do her experiments with mice at Gladstone Institutes in America and analyze the data back home at Sorbonne University in France. She had finished her first round of experiments when the lockdowns forced her to return to Paris, and she hasn't been able to come back to resume her work since. "I can't continue the experiments, which is really frustrating," she says, especially because she doesn't know what it means for her Ph.D. "I may have to entirely change my subject," she says, which she doesn't want to do—it would be a waste of time and money.
But besides wreaking havoc in scholars' personal lives and careers, the visa restrictions had—and will continue to have—tremendous deleterious effects on America's research and its global scientific competitiveness. "It's incredibly short-sighted and self-destructing to restrict the immigration of scientists into the U.S.," says Benjamin G. Neel, who directs the Laura and Isaac Perlmutter Cancer Center at New York University. "If they can't come here, they will go elsewhere," he says, causing a brain drain.

Neel in his lab with postdocs
(Courtesy of Neel)
Neel felt the outcomes of the shortsighted policies firsthand. In the past few months, his lab lost two postdoctoral researchers who had made major strides in understanding the biology of several particularly stubborn, treatment-resistant malignancies. One postdoc studied the underlying mechanisms responsible for 90 percent of pancreatic cancers and half of the colon ones. The other one devised a new system of modeling ovarian cancer in mice to test new therapeutic drug combinations for the deadliest tumor types—but had to return home to China.
"By working around the clock, she was able to get her paper accepted, but she hasn't been able to train us to use this new system, which can set us back six months," Neel says.
Her discoveries also helped the lab secure about $900,000 in grants for new research. Losing people like this is "literally killing the goose that lays the golden eggs," Neel adds. "If you want to make America poor again, this is the way to do it."
Cassidy R. Sugimoto at Indiana University Bloomington, who studies how scientific knowledge is produced and disseminated, says that scientists are the most productive when they are free to move, exchange ideas, and work at labs with the best equipment. Restricting that freedom reduces their achievement.
"Several empirical studied demonstrated the benefits to the U.S. by attracting and retaining foreign scientists. The disproportional number of our Nobel Prize winners were not only foreign-born but also foreign-educated," she says. Scientific advancement bolsters the country's economic prowess, too, so turning scholars away is bad for the economy long-term. "We have been a beneficiary of this flow of human capacity and resource investment for many generations—and this is now threatened," Sugimoto adds—because scientists will look elsewhere. "We are seeing them shifting to other countries that are more hospitable, both ideologically and in terms of health security. Many visiting scholars, postdocs, and graduate students who would otherwise come to the United States are now moving to Canada."
It's not only the Ph.D. students and postdocs who are affected. In some cases, even well-established professors who have already made their marks in the field and direct their own labs at prestigious research institutions may have to pack up and leave the country in the next few months. One scientist who directs a prominent neuroscience lab is betting on his visa renewal and a green card application, but if that's denied, the entire lab may be in jeopardy, as many grants hinge on his ability to stay employed in America.
"It's devastating to even think that it can happen," he says—after years of efforts invested. "I can't even comprehend how it would feel. It would be terrifying and really sad." (He asked to withhold his name for fear that it may adversely affect his applications.) Another scientist who originally shared her story for this article, later changed her mind and withdrew, worrying that speaking out may hurt the entire project, a high-profile COVID-19 effort. It's not how things should work in a democratic country, scientists admit, but that's the reality.
Still, some foreign scholars are speaking up. Mehmet Doğan, a physicist at University of California Berkeley who has been fighting a visa extension battle all year, says it's important to push back in an organized fashion with petitions and engage legislators. "This administration was very creative in finding subtle and not so subtle ways to make our lives more difficult," Doğan says. He adds that the newest rules, proposed by the Department of Homeland Security on September 24, could further limit the time scholars can stay, forcing them into continuous extension battles. That's why the upcoming election might be a turning point for foreign academics. "This election will decide if many of us will see the U.S. as the place to stay and work or whether we look at other countries," Doğan says, echoing the worries of Neel, Sugimoto, and others in academia.

Dogan on Zoom talking to his fellow union members of the Academic Researchers United, a union of almost 5,000 Academic Researchers.
(Credit: Ceyda Durmaz Dogan)
If this year has shown us anything, it is that viruses and pandemics know no borders as they sweep across the globe. Likewise, science can't be restrained by borders either. "Science is an international endeavor," says Neel—and right now humankind now needs unified scientific research more than ever, unhindered by immigration hurdles and visa wars. Humanity's wellbeing in America and beyond depends on it.
[Editor's Note: To read other articles in this special magazine issue, visit the beautifully designed e-reader version.]
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.

