The Science of Why Adjusting to Omicron Is So Tough
A brain expert weighs in on the cognitive biases that hold us back from adjusting to the new reality of Omicron.
We are sticking our heads into the sand of reality on Omicron, and the results may be catastrophic.
Omicron is over 4 times more infectious than Delta. The Pfizer two-shot vaccine offers only 33% protection from infection. A Pfizer booster vaccine does raises protection to about 75%, but wanes to around 30-40 percent 10 weeks after the booster.
The only silver lining is that Omicron appears to cause a milder illness than Delta. Yet the World Health Organization has warned about the “mildness” narrative.
That’s because the much faster disease transmission and vaccine escape undercut the less severe overall nature of Omicron. That’s why hospitals have a large probability of being overwhelmed, as the Center for Disease Control warned, in this major Omicron wave.
Yet despite this very serious threat, we see the lack of real action. The federal government tightened international travel guidelines and is promoting boosters. Certainly, it’s crucial to get as many people to get their booster – and initial vaccine doses – as soon as possible. But the government is not taking the steps that would be the real game-changers.
Pfizer’s anti-viral drug Paxlovid decreases the risk of hospitalization and death from COVID by 89%. Due to this effectiveness, the FDA approved Pfizer ending the trial early, because it would be unethical to withhold the drug from people in the control group. Yet the FDA chose not to hasten the approval process along with the emergence of Omicron in late November, only getting around to emergency authorization in late December once Omicron took over. That delay meant the lack of Paxlovid for the height of the Omicron wave, since it takes many weeks to ramp up production, resulting in an unknown number of unnecessary deaths.
We humans are prone to falling for dangerous judgment errors called cognitive biases.
Widely available at-home testing would enable people to test themselves quickly, so that those with mild symptoms can quarantine instead of infecting others. Yet the federal government did not make tests available to patients when Omicron emerged in late November. That’s despite the obviousness of the coming wave based on the precedent of South Africa, UK, and Denmark and despite the fact that the government made vaccines freely available. Its best effort was to mandate that insurance cover reimbursements for these kits, which is way too much of a barrier for most people. By the time Omicron took over, the federal government recognized its mistake and ordered 500 million tests to be made available in January. However, that’s far too late. And the FDA also played a harmful role here, with its excessive focus on accuracy going back to mid-2020, blocking the widespread availability of cheap at-home tests. By contrast, Europe has a much better supply of tests, due to its approval of quick and slightly less accurate tests.
Neither do we see meaningful leadership at the level of employers. Some are bringing out the tired old “delay the office reopening” play. For example, Google, Uber, and Ford, along with many others, have delayed the return to the office for several months. Those that already returned are calling for stricter pandemic measures, such as more masks and social distancing, but not changing their work arrangements or adding sufficient ventilation to address the spread of COVID.
Despite plenty of warnings from risk management and cognitive bias experts, leaders are repeating the same mistakes we fell into with Delta. And so are regular people. For example, surveys show that Omicron has had very little impact on the willingness of unvaccinated Americans to get a first vaccine dose, or of vaccinated Americans to get a booster. That’s despite Omicron having taken over from Delta in late December.
What explains this puzzling behavior on both the individual and society level? We humans are prone to falling for dangerous judgment errors called cognitive biases. Rooted in wishful thinking and gut reactions, these mental blindspots lead to poor strategic and financial decisions when evaluating choices.
These cognitive biases stem from the more primitive, emotional, and intuitive part of our brains that ensured survival in our ancestral environment. This quick, automatic reaction of our emotions represents the autopilot system of thinking, one of the two systems of thinking in our brains. It makes good decisions most of the time but also regularly makes certain systematic thinking errors, since it’s optimized to help us survive. In modern society, our survival is much less at risk, and our gut is more likely to compel us to focus on the wrong information to make decisions.
One of the biggest challenges relevant to Omicron is the cognitive bias known as the ostrich effect. Named after the myth that ostriches stick their heads into the sand when they fear danger, the ostrich effect refers to people denying negative reality. Delta illustrated the high likelihood of additional dangerous variants, yet we failed to pay attention to and prepare for such a threat.
We want the future to be normal. We’re tired of the pandemic and just want to get back to pre-pandemic times. Thus, we greatly underestimate the probability and impact of major disruptors, like new COVID variants. That cognitive bias is called the normalcy bias.
When we learn one way of functioning in any area, we tend to stick to that way of functioning. You might have heard of this as the hammer-nail syndrome: when you have a hammer, everything looks like a nail. That syndrome is called functional fixedness. This cognitive bias causes those used to their old ways of action to reject any alternatives, including to prepare for a new variant.
Our minds naturally prioritize the present. We want what we want now, and downplay the long-term consequences of our current desires. That fallacious mental pattern is called hyperbolic discounting, where we excessively discount the benefits of orienting toward the future and focus on the present. A clear example is focusing on the short-term perceived gains of trying to return to normal over managing the risks of future variants.
The way forward into the future is to defeat cognitive biases and avoid denying reality by rethinking our approach to the future.
The FDA requires a serious overhaul. It’s designed for a non-pandemic environment, where the goal is to have a highly conservative, slow-going, and risk-averse approach so that the public feels confident trusting whatever it approved. That’s simply unacceptable in a fast-moving pandemic, and we are bound to face future pandemics in the future.
The federal government needs to have cognitive bias experts weigh in on federal policy. Putting all of its eggs in one basket – vaccinations – is not a wise move when we face the risks of a vaccine-escaping variant. Its focus should also be on expediting and prioritizing anti-virals, scaling up cheap rapid testing, and subsidizing high-filtration masks.
For employers, instead of dictating a top-down approach to how employees collaborate, companies need to adopt a decentralized team-led approach. Each individual team leader of a rank-and-file employee team should determine what works best for their team. After all, team leaders tend to know much more of what their teams need, after all. Moreover, they can respond to local emergencies like COVID surges.
At the same time, team leaders need to be trained to integrate best practices for hybrid and remote team leadership. Companies transitioned to telework abruptly as part of the March 2020 lockdowns. They fell into the cognitive bias of functional fixedness and transposed their pre-existing, in-office methods of collaboration on remote work. Zoom happy hours are a clear example: The large majority of employees dislike them, and research shows they are disconnecting, rather than connecting.
Yet supervisors continue to use them, despite the existence of much better methods of facilitating colalboration, which have been shown to work, such as virtual water cooler discussions, virtual coworking, and virtual mentoring. Leaders also need to facilitate innovation in hybrid and remote teams through techniques such as virtual asynchronous brainstorming. Finally, team leaders need to adjust performance evaluation to adapt to the needs of hybrid and remote teams.
On an individual level, people built up certain expectations during the first two years of the pandemic, and they don't apply with Omicron. For example, most people still think that a cloth mask is a fine source of protection. In reality, you really need an N-95 mask, since Omicron is so much more infectious. Another example is that many people don’t realize that symptom onset is much quicker with Omicron, and they aren’t prepared for the consequences.
Remember that we have a huge number of people who are asymptomatic, often without knowing it, due to the much higher mildness of Omicron. About 8% of people admitted to hospitals for other reasons in San Francisco test positive for COVID without symptoms, which we can assume translates for other cities. That means many may think they're fine and they're actually infectious. The result is a much higher chance of someone getting many other people sick.
During this time of record-breaking cases, you need to be mindful about your internalized assumptions and adjust your risk calculus accordingly. So if you can delay higher-risk activities, January and February might be the time to do it. Prepare for waves of disruptions to continue over time, at least through the end of February.
Of course, you might also choose to not worry about getting infected. If you are vaccinated and boosted, and do not have any additional health risks, you are very unlikely to have a serious illness due to Omicron. You can just take the small risk of a serious illness – which can happen – and go about your daily life. If doing so, watch out for those you care about who do have health concerns, since if you infect them, they might not have a mild case even with Omicron.
In short, instead of trying to turn back the clock to the lost world of January 2020, consider how we might create a competitive advantage in our new future. COVID will never go away: we need to learn to live with it. That means reacting appropriately and thoughtfully to new variants and being intentional about our trade-offs.
The Friday Five: How to exercise for cancer prevention
How to exercise for cancer prevention. Plus, a device that brings relief to back pain, ingredients for reducing Alzheimer's risk, the world's oldest disease could make you young again, and more.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Here are the promising studies covered in this week's Friday Five:
- How to exercise for cancer prevention
- A device that brings relief to back pain
- Ingredients for reducing Alzheimer's risk
- Is the world's oldest disease the fountain of youth?
- Scared of crossing bridges? Your phone can help
New approach to brain health is sparking memories
This fall, Robert Reinhart of Boston University published a study finding that electrical stimulation can boost memory - and Reinhart was surprised to discover the effects lasted a full month.
What if a few painless electrical zaps to your brain could help you recall names, perform better on Wordle or even ward off dementia?
This is where neuroscientists are going in efforts to stave off age-related memory loss as well as Alzheimer’s disease. Medications have shown limited effectiveness in reversing or managing loss of brain function so far. But new studies suggest that firing up an aging neural network with electrical or magnetic current might keep brains spry as we age.
Welcome to non-invasive brain stimulation (NIBS). No surgery or anesthesia is required. One day, a jolt in the morning with your own battery-operated kit could replace your wake-up coffee.
Scientists believe brain circuits tend to uncouple as we age. Since brain neurons communicate by exchanging electrical impulses with each other, the breakdown of these links and associations could be what causes the “senior moment”—when you can’t remember the name of the movie you just watched.
In 2019, Boston University researchers led by Robert Reinhart, director of the Cognitive and Clinical Neuroscience Laboratory, showed that memory loss in healthy older adults is likely caused by these disconnected brain networks. When Reinhart and his team stimulated two key areas of the brain with mild electrical current, they were able to bring the brains of older adult subjects back into sync — enough so that their ability to remember small differences between two images matched that of much younger subjects for at least 50 minutes after the testing stopped.
Reinhart wowed the neuroscience community once again this fall. His newer study in Nature Neuroscience presented 150 healthy participants, ages 65 to 88, who were able to recall more words on a given list after 20 minutes of low-intensity electrical stimulation sessions over four consecutive days. This amounted to a 50 to 65 percent boost in their recall.
Even Reinhart was surprised to discover the enhanced performance of his subjects lasted a full month when they were tested again later. Those who benefited most were the participants who were the most forgetful at the start.

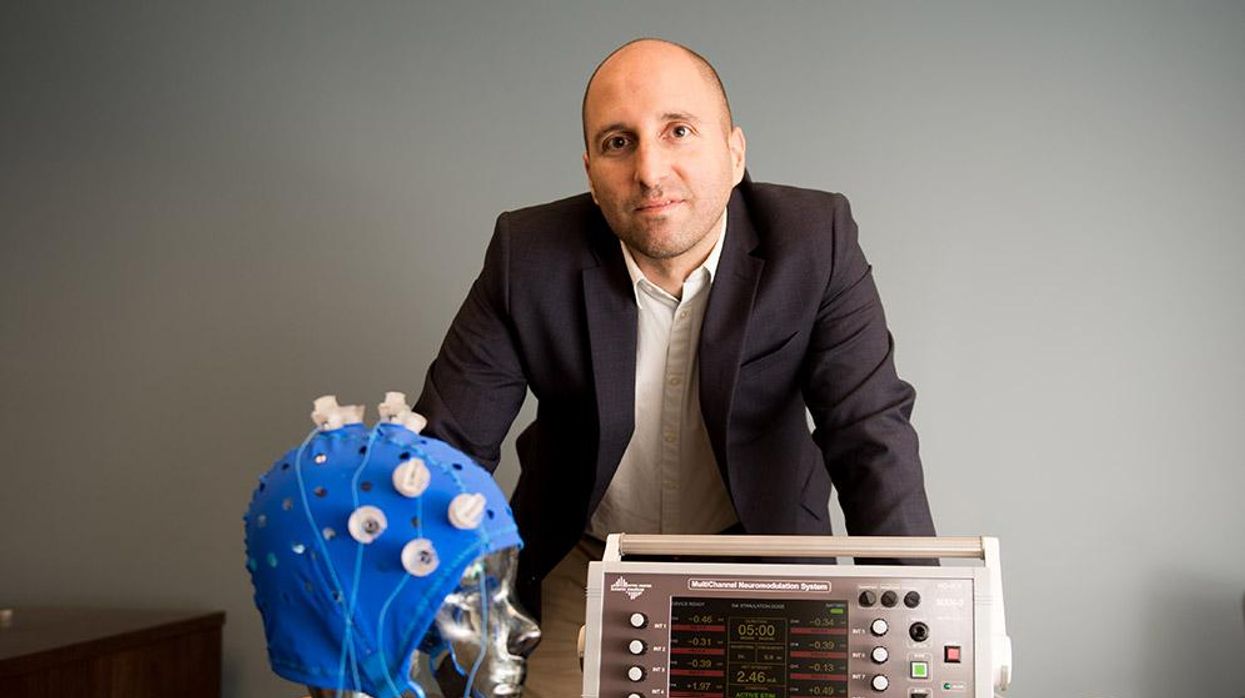
An older person participates in Robert Reinhart's research on brain stimulation.
Robert Reinhart
Reinhart’s subjects only suffered normal age-related memory deficits, but NIBS has great potential to help people with cognitive impairment and dementia, too, says Krista Lanctôt, the Bernick Chair of Geriatric Psychopharmacology at Sunnybrook Health Sciences Center in Toronto. Plus, “it is remarkably safe,” she says.
Lanctôt was the senior author on a meta-analysis of brain stimulation studies published last year on people with mild cognitive impairment or later stages of Alzheimer’s disease. The review concluded that magnetic stimulation to the brain significantly improved the research participants’ neuropsychiatric symptoms, such as apathy and depression. The stimulation also enhanced global cognition, which includes memory, attention, executive function and more.
This is the frontier of neuroscience.
The two main forms of NIBS – and many questions surrounding them
There are two types of NIBS. They differ based on whether electrical or magnetic stimulation is used to create the electric field, the type of device that delivers the electrical current and the strength of the current.
Transcranial Current Brain Stimulation (tES) is an umbrella term for a group of techniques using low-wattage electrical currents to manipulate activity in the brain. The current is delivered to the scalp or forehead via electrodes attached to a nylon elastic cap or rubber headband.
Variations include how the current is delivered—in an alternating pattern or in a constant, direct mode, for instance. Tweaking frequency, potency or target brain area can produce different effects as well. Reinhart’s 2022 study demonstrated that low or high frequencies and alternating currents were uniquely tied to either short-term or long-term memory improvements.
Sessions may be 20 minutes per day over the course of several days or two weeks. “[The subject] may feel a tingling, warming, poking or itching sensation,” says Reinhart, which typically goes away within a minute.
The other main approach to NIBS is Transcranial Magnetic Simulation (TMS). It involves the use of an electromagnetic coil that is held or placed against the forehead or scalp to activate nerve cells in the brain through short pulses. The stimulation is stronger than tES but similar to a magnetic resonance imaging (MRI) scan.
The subject may feel a slight knocking or tapping on the head during a 20-to-60-minute session. Scalp discomfort and headaches are reported by some; in very rare cases, a seizure can occur.
No head-to-head trials have been conducted yet to evaluate the differences and effectiveness between electrical and magnetic current stimulation, notes Lanctôt, who is also a professor of psychiatry and pharmacology at the University of Toronto. Although TMS was approved by the FDA in 2008 to treat major depression, both techniques are considered experimental for the purpose of cognitive enhancement.
“One attractive feature of tES is that it’s inexpensive—one-fifth the price of magnetic stimulation,” Reinhart notes.
Don’t confuse either of these procedures with the horrors of electroconvulsive therapy (ECT) in the 1950s and ‘60s. ECT is a more powerful, riskier procedure used only as a last resort in treating severe mental illness today.
Clinical studies on NIBS remain scarce. Standardized parameters and measures for testing have not been developed. The high heterogeneity among the many existing small NIBS studies makes it difficult to draw general conclusions. Few of the studies have been replicated and inconsistencies abound.
Scientists are still lacking so much fundamental knowledge about the brain and how it works, says Reinhart. “We don’t know how information is represented in the brain or how it’s carried forward in time. It’s more complex than physics.”
Lanctôt’s meta-analysis showed improvements in global cognition from delivering the magnetic form of the stimulation to people with Alzheimer’s, and this finding was replicated inan analysis in the Journal of Prevention of Alzheimer’s Disease this fall. Neither meta-analysis found clear evidence that applying the electrical currents, was helpful for Alzheimer’s subjects, but Lanctôt suggests this might be merely because the sample size for tES was smaller compared to the groups that received TMS.
At the same time, London neuroscientist Marco Sandrini, senior lecturer in psychology at the University of Roehampton, critically reviewed a series of studies on the effects of tES on episodic memory. Often declining with age, episodic memory relates to recalling a person’s own experiences from the past. Sandrini’s review concluded that delivering tES to the prefrontal or temporoparietal cortices of the brain might enhance episodic memory in older adults with Alzheimer’s disease and amnesiac mild cognitive impairment (the predementia phase of Alzheimer’s when people start to have symptoms).
Researchers readily tick off studies needed to explore, clarify and validate existing NIBS data. What is the optimal stimulus session frequency, spacing and duration? How intense should the stimulus be and where should it be targeted for what effect? How might genetics or degree of brain impairment affect responsiveness? Would adjunct medication or cognitive training boost positive results? Could administering the stimulus while someone sleeps expedite memory consolidation?
Using MRI or another brain scan along with computational modeling of the current flow, a clinician could create a treatment that is customized to each person’s brain.
While Sandrini’s review reported improvements induced by tES in the recall or recognition of words and images, there is no evidence it will translate into improvements in daily activities. This is another question that will require more research and testing, Sandrini notes.
Scientists are still lacking so much fundamental knowledge about the brain and how it works, says Reinhart. “We don’t know how information is represented in the brain or how it’s carried forward in time. It’s more complex than physics.”
Where the science is headed
Learning how to apply precision medicine to NIBS is the next focus in advancing this technology, says Shankar Tumati, a post-doctoral fellow working with Lanctôt.
There is great variability in each person’s brain anatomy—the thickness of the skull, the brain’s unique folds, the amount of cerebrospinal fluid. All of these structural differences impact how electrical or magnetic stimulation is distributed in the brain and ultimately the effects.
Using MRI or another brain scan along with computational modeling of the current flow, a clinician could create a treatment that is customized to each person’s brain, from where to put the electrodes to determining the exact dose and duration of stimulation needed to achieve lasting results, Sandrini says.
Above all, most neuroscientists say that largescale research studies over long periods of time are necessary to confirm the safety and durability of this therapy for the purpose of boosting memory. Short of that, there can be no FDA approval or medical regulation for this clinical use.
Lanctôt urges people to seek out clinical NIBS trials in their area if they want to see the science advance. “That is how we’ll find the answers,” she says, predicting it will be 5 to 10 years to develop each additional clinical application of NIBS. Ultimately, she predicts that reigning in Alzheimer’s disease and mild cognitive impairment will require a multi-pronged approach that includes lifestyle and medications, too.
Sandrini believes that scientific efforts should focus on preventing or delaying Alzheimer’s. “We need to start intervention earlier—as soon as people start to complain about forgetting things,” he says. “Changes in the brain start 10 years before [there is a problem]. Once Alzheimer’s develops, it is too late.”