Pregnant & Breastfeeding Women Who Get the COVID-19 Vaccine Are Protecting Their Infants, Research Suggests

Becky Cummings, who got vaccinated in December, snuggles her newborn, Clark, while he takes a nap.
Becky Cummings had multiple reasons to get vaccinated against COVID-19 while tending to her firstborn, Clark, who arrived in September 2020 at 27 weeks.
The 29-year-old intensive care unit nurse in Greensboro, North Carolina, had witnessed the devastation day in and day out as the virus took its toll on the young and old. But when she was offered the vaccine, she hesitated, skeptical of its rapid emergency use authorization.
Exclusion of pregnant and lactating mothers from clinical trials fueled her concerns. Ultimately, though, she concluded the benefits of vaccination outweighed the risks of contracting the potentially deadly virus.
"Long story short," Cummings says, in December "I got vaccinated to protect myself, my family, my patients, and the general public."
At the time, Cummings remained on the fence about breastfeeding, citing a lack of evidence to support its safety after vaccination, so she pumped and stashed breast milk in the freezer. Her son is adjusting to life as a preemie, requiring mother's milk to be thickened with formula, but she's becoming comfortable with the idea of breastfeeding as more research suggests it's safe.
"If I could pop him on the boob," she says, "I would do it in a heartbeat."
Now, a study recently published in the Journal of the American Medical Association found "robust secretion" of specific antibodies in the breast milk of mothers who received a COVID-19 vaccine, indicating a potentially protective effect against infection in their infants.
The presence of antibodies in the breast milk, detectable as early as two weeks after vaccination, lasted for six weeks after the second dose of the Pfizer-BioNTech vaccine.
"We believe antibody secretion into breast milk will persist for much longer than six weeks, but we first wanted to prove any secretion at all after vaccination," says Ilan Youngster, the study's corresponding author and head of pediatric infectious diseases at Shamir Medical Center in Zerifin, Israel.
That's why the research team performed a preliminary analysis at six weeks. "We are still collecting samples from participants and hope to soon be able to comment about the duration of secretion."
As with other respiratory illnesses, such as influenza and pertussis, secretion of antibodies in breast milk confers protection from infection in infants. The researchers expect a similar immune response from the COVID-19 vaccine and are expecting the findings to spur an increase in vaccine acceptance among pregnant and lactating women.
A COVID-19 outbreak struck three families the research team followed in the study, resulting in at least one non-breastfed sibling developing symptomatic infection; however, none of the breastfed babies became ill. "This is obviously not empirical proof," Youngster acknowledges, "but still a nice anecdote."
Leaps.org inquired whether infants who derive antibodies only through breast milk are likely to have a lower immunity than infants whose mothers were vaccinated while they were in utero. In other words, is maternal transmission of antibodies stronger during pregnancy than during breastfeeding, or about the same?
"This is a different kind of transmission," Youngster explains. "When a woman is infected or vaccinated during pregnancy, some antibodies will be transferred through the placenta to the baby's bloodstream and be present for several months." But in the nursing mother, that protection occurs through local action. "We always recommend breastfeeding whenever possible, and, in this case, it might have added benefits."
A study published online in March found COVID-19 vaccination provided pregnant and lactating women with robust immune responses comparable to those experienced by their nonpregnant counterparts. The study, appearing in the American Journal of Obstetrics and Gynecology, documented the presence of vaccine-generated antibodies in umbilical cord blood and breast milk after mothers had been vaccinated.
Natali Aziz, a maternal-fetal medicine specialist at Stanford University School of Medicine, notes that it's too early to draw firm conclusions about the reduction in COVID-19 infection rates among newborns of vaccinated mothers. Citing the two aforementioned research studies, she says it's biologically plausible that antibodies passed through the placenta and breast milk impart protective benefits. While thousands of pregnant and lactating women have been vaccinated against COVID-19, without incurring adverse outcomes, many are still wondering whether it's safe to breastfeed afterward.
It's important to bear in mind that pregnant women may develop more severe COVID-19 complications, which could lead to intubation or admittance to the intensive care unit. "We, in our practice, are supporting pregnant and breastfeeding patients to be vaccinated," says Aziz, who is also director of perinatal infectious diseases at Stanford Children's Health, which has been vaccinating new mothers and other hospitalized patients at discharge since late April.
Earlier in April, Huntington Hospital in Long Island, New York, began offering the COVID-19 vaccine to women after they gave birth. The hospital chose the one-shot Johnson & Johnson vaccine for postpartum patients, so they wouldn't need to return for a second shot while acclimating to life with a newborn, says Mitchell Kramer, chairman of obstetrics and gynecology.
The hospital suspended the program when the Food and Drug Administration and the Centers for Disease Control and Prevention paused use of the J&J vaccine starting April 13, while investigating several reports of dangerous blood clots and low platelet counts among more than 7 million people in the United States who had received that vaccine.
In lifting the pause April 23, the agencies announced the vaccine's fact sheets will bear a warning of the heightened risk for a rare but serious blood clot disorder among women under age 50. As a result, Kramer says, "we will likely not be using the J&J vaccine for our postpartum population."
So, would it make sense to vaccinate infants when one for them eventually becomes available, not just their mothers? "In general, most of the time, infants do not have as good of an immune response to vaccines," says Jonathan Temte, associate dean for public health and community engagement at the University of Wisconsin School of Medicine and Public Health in Madison.
"Many of our vaccines are held until children are six months of age. For example, the influenza vaccine starts at age six months, the measles vaccine typically starts one year of age, as do rubella and mumps. Immune response is typically not very good for viral illnesses in young infants under the age of six months."
So far, the FDA has granted emergency use authorization of the Pfizer-BioNTech vaccine for children as young as 16 years old. The agency is considering data from Pfizer to lower that age limit to 12. Studies are also underway in children under age 12. Meanwhile, data from Moderna on 12-to 17-year-olds and from Pfizer on 12- to 15-year-olds have not been made public. (Pfizer announced at the end of March that its vaccine is 100 percent effective in preventing COVID-19 in the latter age group, and FDA authorization for this population is expected soon.)
"There will be step-wise progression to younger children, with infants and toddlers being the last ones tested," says James Campbell, a pediatric infectious diseases physician and head of maternal and child clinical studies at the University of Maryland School of Medicine Center for Vaccine Development.
"Once the data are analyzed for safety, tolerability, optimal dose and regimen, and immune responses," he adds, "they could be authorized and recommended and made available to American children." The data on younger children are not expected until the end of this year, with regulatory authorization possible in early 2022.
For now, Vonnie Cesar, a family nurse practitioner in Smyrna, Georgia, is aiming to persuade expectant and new mothers to get vaccinated. She has observed that patients in metro Atlanta seem more inclined than their rural counterparts.
To quell some of their skepticism and fears, Cesar, who also teaches nursing students, conceived a visual way to demonstrate the novel mechanism behind the COVID-19 vaccine technology. Holding a palm-size physical therapy ball outfitted with clear-colored push pins, she simulates the spiked protein of the coronavirus. Slime slathered at the gaps permeates areas around the spikes—a process similar to how our antibodies build immunity to the virus.
These conversations often lead hesitant patients to discuss vaccination with their husbands or partners. "The majority of people I'm speaking with," she says, "are coming to the conclusion that this is the right thing for me, this is the common good, and they want to make sure that they're here for their children."
CORRECTION: An earlier version of this article mistakenly stated that the COVID-19 vaccines were granted emergency "approval." They have been granted emergency use authorization, not full FDA approval. We regret the error.
Researchers advance drugs that treat pain without addiction
New therapies are using creative approaches that target the body’s sensory neurons, which send pain signals to the brain.
Opioids are one of the most common ways to treat pain. They can be effective but are also highly addictive, an issue that has fueled the ongoing opioid crisis. In 2020, an estimated 2.3 million Americans were dependent on prescription opioids.
Opioids bind to receptors at the end of nerve cells in the brain and body to prevent pain signals. In the process, they trigger endorphins, so the brain constantly craves more. There is a huge risk of addiction in patients using opioids for chronic long-term pain. Even patients using the drugs for acute short-term pain can become dependent on them.
Scientists have been looking for non-addictive drugs to target pain for over 30 years, but their attempts have been largely ineffective. “We desperately need alternatives for pain management,” says Stephen E. Nadeau, a professor of neurology at the University of Florida.
A “dimmer switch” for pain
Paul Blum is a professor of biological sciences at the University of Nebraska. He and his team at Neurocarrus have created a drug called N-001 for acute short-term pain. N-001 is made up of specially engineered bacterial proteins that target the body’s sensory neurons, which send pain signals to the brain. The proteins in N-001 turn down pain signals, but they’re too large to cross the blood-brain barrier, so they don’t trigger the release of endorphins. There is no chance of addiction.
When sensory neurons detect pain, they become overactive and send pain signals to the brain. “We wanted a way to tone down sensory neurons but not turn them off completely,” Blum reveals. The proteins in N-001 act “like a dimmer switch, and that's key because pain is sensation overstimulated.”
Blum spent six years developing the drug. He finally managed to identify two proteins that form what’s called a C2C complex that changes the structure of a subunit of axons, the parts of neurons that transmit electrical signals of pain. Changing the structure reduces pain signaling.
“It will be a long path to get to a successful clinical trial in humans," says Stephen E. Nadeau, professor of neurology at the University of Florida. "But it presents a very novel approach to pain reduction.”
Blum is currently focusing on pain after knee and ankle surgery. Typically, patients are treated with anesthetics for a short time after surgery. But anesthetics usually only last for 4 to 6 hours, and long-term use is toxic. For some, the pain subsides. Others continue to suffer after the anesthetics have worn off and start taking opioids.
N-001 numbs sensation. It lasts for up to 7 days, much longer than any anesthetic. “Our goal is to prolong the time before patients have to start opioids,” Blum says. “The hope is that they can switch from an anesthetic to our drug and thereby decrease the likelihood they're going to take the opioid in the first place.”
Their latest animal trial showed promising results. In mice, N-001 reduced pain-like behaviour by 90 percent compared to the control group. One dose became effective in two hours and lasted a week. A high dose had pain-relieving effects similar to an opioid.
Professor Stephen P. Cohen, director of pain operations at John Hopkins, believes the Neurocarrus approach has potential but highlights the need to go beyond animal testing. “While I think it's promising, it's an uphill battle,” he says. “They have shown some efficacy comparable to opioids, but animal studies don't translate well to people.”
Nadeau, the University of Florida neurologist, agrees. “It will be a long path to get to a successful clinical trial in humans. But it presents a very novel approach to pain reduction.”
Blum is now awaiting approval for phase I clinical trials for acute pain. He also hopes to start testing the drug's effect on chronic pain.
Learning from people who feel no pain
Like Blum, a pharmaceutical company called Vertex is focusing on treating acute pain after surgery. But they’re doing this in a different way, by targeting a sodium channel that plays a critical role in transmitting pain signals.
In 2004, Stephen Waxman, a neurology professor at Yale, led a search for genetic pain anomalies and found that biologically related people who felt no pain despite fractures, burns and even childbirth had mutations in the Nav1.7 sodium channel. Further studies in other families who experienced no pain showed similar mutations in the Nav1.8 sodium channel.
Scientists set out to modify these channels. Many unsuccessful efforts followed, but Vertex has now developed VX-548, a medicine to inhibit Nav1.8. Typically, sodium ions flow through sodium channels to generate rapid changes in voltage which create electrical pulses. When pain is detected, these pulses in the Nav1.8 channel transmit pain signals. VX-548 uses small molecules to inhibit the channel from opening. This blocks the flow of sodium ions and the pain signal. Because Nav1.8 operates only in peripheral nerves, located outside the brain, VX-548 can relieve pain without any risk of addiction.
"Frankly we need drugs for chronic pain more than acute pain," says Waxman.
The team just finished phase II clinical trials for patients following abdominoplasty surgery and bunionectomy surgery.
After abdominoplasty surgery, 76 patients were treated with a high dose of VX-548. Researchers then measured its effectiveness in reducing pain over 48 hours, using the SPID48 scale, in which higher scores are desirable. The score for Vertex’s drug was 110.5 compared to 72.7 in the placebo group, whereas the score for patients taking an opioid was 85.2. The study involving bunionectomy surgery showed positive results as well.
Waxman, who has been at the forefront of studies into Nav1.7 and Nav1.8, believes that Vertex's results are promising, though he highlights the need for further clinical trials.
“Blocking Nav1.8 is an attractive target,” he says. “[Vertex is] studying pain that is relatively simple and uniform, and that's key to having a drug trial that is informative. But the study needs to be replicated and frankly we need drugs for chronic pain more than acute pain. If this is borne out by additional studies, it's one important step in a journey.”
Vertex will be launching phase III trials later this year.
Finding just the right amount of Nerve Growth Factor
Whereas Neurocarrus and Vertex are targeting short-term pain, a company called Levicept is concentrating on relieving chronic osteoarthritis pain. Around 32.5 million Americans suffer from osteoarthritis. Patients commonly take NSAIDs, or non-steroidal anti-inflammatory drugs, but they cannot be taken long-term. Some take opioids but they aren't very effective.
Levicept’s drug, Levi-04, is designed to modify a signaling pathway associated with pain. Nerve Growth Factor (NGF) is a neurotrophin: it’s involved in nerve growth and function. NGF signals by attaching to receptors. In pain there are excess neurotrophins attaching to receptors and activating pain signals.
“What Levi-04 does is it returns the natural equilibrium of neurotrophins,” says Simon Westbrook, the CEO and founder of Levicept. It stabilizes excess neurotrophins so that the NGF pathway does not signal pain. Levi-04 isn't addictive since it works within joints and in nerves outside the brain.
Westbrook was initially involved in creating an anti-NGF molecule for Pfizer called Tanezumab. At first, Tanezumab seemed effective in clinical trials and other companies even started developing their own versions. However, a problem emerged. Tanezumab caused rapidly progressive osteoarthritis, or RPOA, in some patients because it completely removed NGF from the system. NGF is not just involved in pain signalling, it’s also involved in bone growth and maintenance.
Levicept has found a way to modify the NGF pathway without completely removing NGF. They have now finished a small-scale phase I trial mainly designed to test safety rather than efficacy. “We demonstrated that Levi-04 is safe and that it bound to its target, NGF,” says Westbrook. It has not caused RPOA.
Professor Philip Conaghan, director of the Leeds Institute of Rheumatic and Musculoskeletal Medicine, believes that Levi-04 has potential but urges the need for caution. “At this early stage of development, their molecule looks promising for osteoarthritis pain,” he says. “They will have to watch out for RPOA which is a potential problem.”
Westbrook starts phase II trials with 500 patients this summer to check for potential side effects and test the drug’s efficacy.
There is a real push to find an effective alternative to opioids. “We have a lot of work to do,” says Professor Waxman. “But I am confident that we will be able to develop new, much more effective pain therapies.”
Tech-related injuries are becoming more common as many people depend on - and often develop addictions for - smart phones and computers.
In the 1990s, a mysterious virus spread throughout the Massachusetts Institute of Technology Artificial Intelligence Lab—or that’s what the scientists who worked there thought. More of them rubbed their aching forearms and massaged their cricked necks as new computers were introduced to the AI Lab on a floor-by-floor basis. They realized their musculoskeletal issues coincided with the arrival of these new computers—some of which were mounted high up on lab benches in awkward positions—and the hours spent typing on them.
Today, these injuries have become more common in a society awash with smart devices, sleek computers, and other gadgets. And we don’t just get hurt from typing on desktop computers; we’re massaging our sore wrists from hours of texting and Facetiming on phones, especially as they get bigger in size.
In 2007, the first iPhone measured 3.5-inches diagonally, a measurement known as the display size. That’s been nearly doubled by the newest iPhone 13 Pro, which has a 6.7-inch display. Other phones, too, like the Google Pixel 6 and the Samsung Galaxy S22, have bigger screens than their predecessors. Physical therapists and orthopedic surgeons have had to come up with names for a variety of new conditions: selfie elbow, tech neck, texting thumb. Orthopedic surgeon Sonya Sloan says she sees selfie elbow in younger kids and in women more often than men. She hears complaints related to technology once or twice a day.
The addictive quality of smartphones and social media means that people spend more time on their devices, which exacerbates injuries. According to Statista, 68 percent of those surveyed spent over three hours a day on their phone, and almost half spent five to six hours a day. Another report showed that people dedicate a third of their day to checking their phones, while the Media Effects Research Laboratory at Pennsylvania State University has found that bigger screens, ideal for entertainment purposes, immerse their users more than smaller screens. Oversized screens also provide easier navigation and more space for those with bigger hands or trouble seeing.
But others with conditions like arthritis can benefit from smaller phones. In March of 2016, Apple released the iPhone SE with a display size of 4.7 inches—an inch smaller than the iPhone 7, released that September. Apple has since come out with two more versions of the diminutive iPhone SE, one in 2020 and another in 2022.
These devices are now an inextricable part of our lives. So where does the burden of responsibility lie? Is it with consumers to adjust body positioning, get ergonomic workstations, and change habits to abate tech-related pain? Or should tech companies be held accountable?
Kavin Senapathy, a freelance science journalist, has the Google Pixel 6. She was drawn to the phone because Google marketed the Pixel 6’s camera as better at capturing different skin tones. But this phone boasts one of the largest display sizes on the market: 6.4 inches.
Senapathy was diagnosed with carpal and cubital tunnel syndromes in 2017 and fibromyalgia in 2019. She has had to create a curated ergonomic workplace setup, otherwise her wrists and hands get weak and tingly, and she’s had to adjust how she holds her phone to prevent pain flares.
Recently, Senapathy underwent an electromyography, or an EMG, in which doctors insert electrodes into muscles to measure their electrical activity. The electrical response of the muscles tells doctors whether the nerve cells and muscles are successfully communicating. Depending on her results, steroid shots and even surgery might be required. Senapathy wants to stick with her Pixel 6, but the pain she’s experiencing may push her to buy a smaller phone. Unfortunately, options for these modestly sized phones are more limited.
These devices are now an inextricable part of our lives. So where does the burden of responsibility lie? Is it with consumers like Senapathy to adjust body positioning, get ergonomic workstations, and change habits to abate tech-related pain? Or should tech companies be held accountable for creating addictive devices that lead to musculoskeletal injury?

Kavin Senapathy, a freelance journalist, bought the Google Pixel 6 because of its high-quality camera, but she’s had to adjust how she holds the oversized phone to prevent pain flares.
Kavin Senapathy
A one-size-fits-all mentality for smartphones will continue to lead to injuries because every user has different wants and needs. S. Shyam Sundar, the founder of Penn State’s lab on media effects and a communications professor, says the needs for mobility and portability conflict with the desire for greater visibility. “The best thing a company can do is offer different sizes,” he says.
Joanna Bryson, an AI ethics expert and professor at The Hertie School of Governance in Berlin, Germany, echoed these sentiments. “A lot of the lack of choice we see comes from the fact that the markets have consolidated so much,” she says. “We want to make sure there’s sufficient diversity [of products].”
Consumers can still maintain some control despite the ubiquity of tech. Sloan, the orthopedic surgeon, has to pester her son to change his body positioning when using his tablet. Our heads get heavier as they bend forward: at rest, they weigh 12 pounds, but bent 60 degrees, they weigh 60. “I have to tell him, ‘Raise your head, son!’” she says. It’s important, Sloan explains, to consider that growth and development will affect ligaments and bones in the neck, potentially making kids even more vulnerable to injuries from misusing gadgets. She recommends that parents limit their kids’ tech time to alleviate strain. She also suggested that tech companies implement a timer to remind us to change our body positioning.
In 2017, Nan-Wei Gong, a former contractor for Google, founded Figur8, which uses wearable trackers to measure muscle function and joint movement. It’s like physical therapy with biofeedback. “Each unique injury has a different biomarker,” says Gong. “With Figur8, you are comparing yourself to yourself.” This allows an individual to self-monitor for wear and tear and strengthen an injury in a way that’s efficient and designed for their body. Gong noticed that the work-from-home model during the COVID-19 pandemic created a new set of ergonomic problems that resulted in injuries. Figur8 provides real-time data for these injuries because “behavioral change requires feedback.”
Gong worked on a project called Jacquard while at Google. Textile experts weave conductive thread into their fabric, and the result is a patch of the fabric—like the cuff of a Levi’s jacket—that responds to commands on your smartphone. One swipe can call your partner or check the weather. It was designed with cyclists in mind who can’t easily check their phones, and it’s part of a growing movement in the tech industry to deliver creative, hands-free design. Gong thinks that engineers at large corporations like Google have accessibility in mind; it’s part of what drives their decisions for new products.
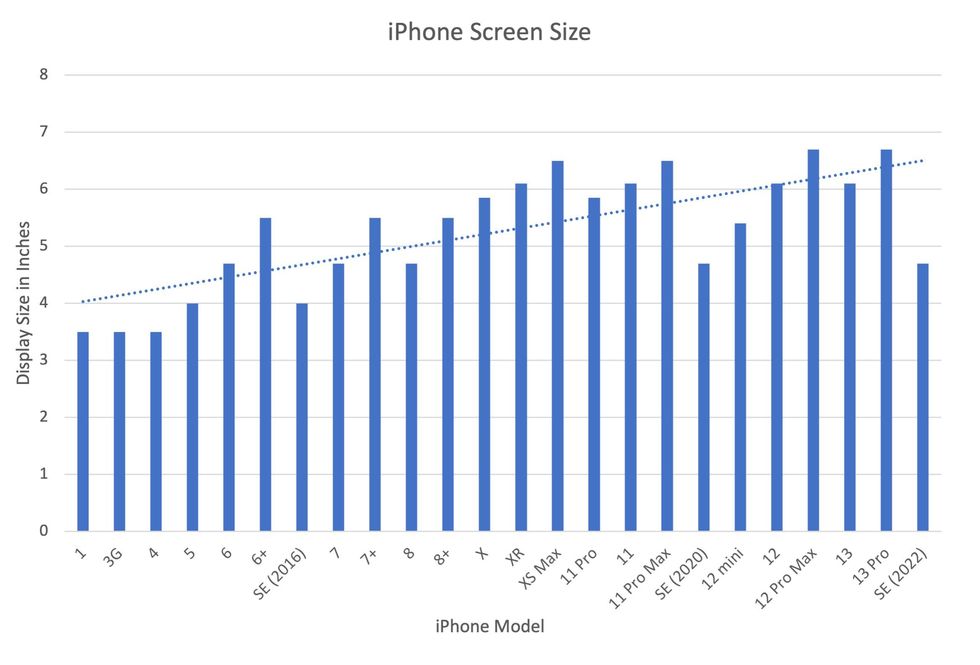
Display sizes of iPhones have become larger over time.
Sourced from Screenrant https://screenrant.com/iphone-apple-release-chronological-order-smartphone/ and Apple Tech Specs: https://www.apple.com/iphone-se/specs/
Back in Germany, Joanna Bryson reminds us that products like smartphones should adhere to best practices. These rules may be especially important for phones and other products with AI that are addictive. Disclosure, accountability, and regulation are important for AI, she says. “The correct balance will keep changing. But we have responsibilities and obligations to each other.” She was on an AI Ethics Council at Google, but the committee was disbanded after only one week due to issues with one of their members.
Bryson was upset about the Council’s dissolution but has faith that other regulatory bodies will prevail. OECD.AI, and international nonprofit, has drafted policies to regulate AI, which countries can sign and implement. “As of July 2021, 46 governments have adhered to the AI principles,” their website reads.
Sundar, the media effects professor, also directs Penn State’s Center for Socially Responsible AI. He says that inclusivity is a crucial aspect of social responsibility and how devices using AI are designed. “We have to go beyond first designing technologies and then making them accessible,” he says. “Instead, we should be considering the issues potentially faced by all different kinds of users before even designing them.”