7 Things to Know about the U.S.’s Capability to Detect Omicron
A visualization of the original coronavirus causing COVID-19, which has now been detected across the globe in a highly mutated form called Omicron.
If the new variant Omicron isn’t here already – which many experts suspect that it is – it will be soon. While we wait for scientists to conduct the necessary research to characterize its transmissibility, potential fitness at immune evasion, and disease severity, we wanted to give Leaps.org readers a window into how the U.S. is positioned to detect the variant. So we spoke to Kelly Wroblewski, director of infectious diseases at the Association of Public Health Laboratories, a membership organization that represents state and local government health labs in the United States. Here are seven insights she shared.
1) If you test positive for COVID-19 with a standard PCR test, the diagnostic report will not tell you which variant you have. There are no diagnostic tests available for your doctor to order to identify variants. To find out the variant, the specimen must be sent to a commercial, clinical, academic, or public health laboratory for genetic sequencing.
2) Today, the U.S. sequences about 5 to 10 percent of all diagnostic specimens that test positive for SARS-CoV-2 in order to determine which variants are circulating and where. Last week nationally, for example, labs sequenced about 80,000 samples. This represents a massive increase from last year at this time, when labs were only sequencing about 8,000 specimens per week. Currently, 99.5 percent of circulating SARS-CoV-2 virus in the U.S. is the Delta variant.
3) The U.S. is “very well prepared” to detect Omicron, Wroblewski says, “particularly compared to where we were when the Alpha variant, or B117 first emerged.” Of the hunt for Omicron, she adds, “it’s very reminiscent of that time, except we are doing so much more sequencing and we have so much better coverage with our sequencing geographically, and we're doing it in a much more timely way. We have the ability to find emerging variants that are circulating in 0.01 percent of the population.”
4) Deciding which specimens to sample is not totally random. Samples that have more virus are likely to lead to better sequencing results. Labs also look to have a diverse set of representative samples, meaning across geographic regions and across gender, race, ethnicity, and age groups. Clinical diversity is also important, such as including pregnant women, severe in-patient cases, mild cases, etc.
5) Sequencing more is not necessarily better to find Omicron faster. “We will increase the number of sequences to a certain extent,” Wroblewski says. “Where we exhibit some caution is doing that indiscriminately isn’t the most effective use of time and resources. The important thing is to try to find Omicron, and if you increase your testing capacity too much, right now, it's still predominantly Delta in the U.S. by a long shot. So you’re mostly going to sequence Delta and you run the risk of delaying your discovery of Omicron, if you focus solely on increasing sequencing.”
So besides just ramping up the sheer numbers of sequencing, diagnostic labs across the country are now advised to preferentially use a certain PCR test made by Thermo Fisher that can help hasten the detection of Omicron. It turns out that Omicron’s specific mutations in the Spike protein mean that the Spike is not picked up on this PCR test, which yields a type of result called an S-gene target failure. Yet the test will still accurately pick up a COVID-19 diagnosis, because it detects two other gene targets on Omicron that are not mutated. “That S-gene target failure gives you a good indication that you may have Omicron. It’s a good early screen.”
Labs will then still need to sequence the whole genome to confirm it matches the Omicron sequence. “So right now, the new recommendation is to use [the Thermo Fisher test] as much as possible to give us a better chance of detecting Omicron more quickly.”
6) This Thermo Fisher test is “fairly widely used” in the U.S. already, so many labs are already well positioned to make the shift. “In early to mid 2020,” Wroblewski explains, “when the supply chain issue for testing was acute, many public health labs implemented five, six, seven, eight different tests, just so they could get enough supplies to do all the testing. Now that we're in a much better place supply-chain wise, it's very difficult and time consuming and cumbersome to maintain all those different test methods all the time, and many, many labs scaled back to only one or two. And so this [new recommendation] would just be shifting to two for some labs that will be shifting to them.”
7) Once Omicron is found here, labs will be focused on finding as many cases as possible, and the CDC will be conducting a variety of studies to determine the impact of the variant on diagnostics, therapeutics, and vaccines. Epidemiologists at the local, state, and federal level will analyze which populations it is spreading in, as well as the severity of the disease it causes. They will work to sort out different impacts on vaccinated vs. unvaccinated populations. The ultimate goal, Wroblewski concludes, is to “use all of that information to make better public health decisions and inform the public about what’s going on.”
1) If you test positive for COVID-19 with a standard PCR test, the diagnostic report will not tell you which variant you have. There are no diagnostic tests available for your doctor to order to identify variants. To find out the variant, the specimen must be sent to a commercial, clinical, academic, or public health laboratory for genetic sequencing.
2) Today, the U.S. sequences about 5 to 10 percent of all diagnostic specimens that test positive for SARS-CoV-2 in order to determine which variants are circulating and where. Last week nationally, for example, labs sequenced about 80,000 samples. This represents a massive increase from last year at this time, when labs were only sequencing about 8,000 specimens per week. Currently, 99.5 percent of circulating SARS-CoV-2 virus in the U.S. is the Delta variant.
3) The U.S. is “very well prepared” to detect Omicron, Wroblewski says, “particularly compared to where we were when the Alpha variant, or B117 first emerged.” Of the hunt for Omicron, she adds, “it’s very reminiscent of that time, except we are doing so much more sequencing and we have so much better coverage with our sequencing geographically, and we're doing it in a much more timely way. We have the ability to find emerging variants that are circulating in 0.01 percent of the population.”
4) Deciding which specimens to sample is not totally random. Samples that have more virus are likely to lead to better sequencing results. Labs also look to have a diverse set of representative samples, meaning across geographic regions and across gender, race, ethnicity, and age groups. Clinical diversity is also important, such as including pregnant women, severe in-patient cases, mild cases, etc.
5) Sequencing more is not necessarily better to find Omicron faster. “We will increase the number of sequences to a certain extent,” Wroblewski says. “Where we exhibit some caution is doing that indiscriminately isn’t the most effective use of time and resources. The important thing is to try to find Omicron, and if you increase your testing capacity too much, right now, it's still predominantly Delta in the U.S. by a long shot. So you’re mostly going to sequence Delta and you run the risk of delaying your discovery of Omicron, if you focus solely on increasing sequencing.”
So besides just ramping up the sheer numbers of sequencing, diagnostic labs across the country are now advised to preferentially use a certain PCR test made by Thermo Fisher that can help hasten the detection of Omicron. It turns out that Omicron’s specific mutations in the Spike protein mean that the Spike is not picked up on this PCR test, which yields a type of result called an S-gene target failure. Yet the test will still accurately pick up a COVID-19 diagnosis, because it detects two other gene targets on Omicron that are not mutated. “That S-gene target failure gives you a good indication that you may have Omicron. It’s a good early screen.”
Labs will then still need to sequence the whole genome to confirm it matches the Omicron sequence. “So right now, the new recommendation is to use [the Thermo Fisher test] as much as possible to give us a better chance of detecting Omicron more quickly.”
6) This Thermo Fisher test is “fairly widely used” in the U.S. already, so many labs are already well positioned to make the shift. “In early to mid 2020,” Wroblewski explains, “when the supply chain issue for testing was acute, many public health labs implemented five, six, seven, eight different tests, just so they could get enough supplies to do all the testing. Now that we're in a much better place supply-chain wise, it's very difficult and time consuming and cumbersome to maintain all those different test methods all the time, and many, many labs scaled back to only one or two. And so this [new recommendation] would just be shifting to two for some labs that will be shifting to them.”
7) Once Omicron is found here, labs will be focused on finding as many cases as possible, and the CDC will be conducting a variety of studies to determine the impact of the variant on diagnostics, therapeutics, and vaccines. Epidemiologists at the local, state, and federal level will analyze which populations it is spreading in, as well as the severity of the disease it causes. They will work to sort out different impacts on vaccinated vs. unvaccinated populations. The ultimate goal, Wroblewski concludes, is to “use all of that information to make better public health decisions and inform the public about what’s going on.”
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
An intergalactic explorer on a hypothetical mission to Mars.
Social isolation. Strange pathogens outside. Strategic resource planning. Our Earthbound pandemic-driven social distancing could be mistaken for adapting to another, foreign planet. After all, we're donning all our protective apparel to go on an airplane or to the grocery store, nevertheless to just open our front door. Perhaps this is training for the world galactic visionaries Elon Musk, Jeff Bezos, and Richard Branson see in our future.
"There are parallels to the individual psychological experience, but from an operational standpoint, it is too different."
Ready to go live on Mars or something? Not so fast, experts say. The experience of shelter in place isn't parallel to being a space settler, or even an astronaut.
"Certain aspects are similar, but still, honestly, there are too many differences to say it preps us," says Angelo Vermeulen, co-founder of the art-science collective SEADS (Space Ecologies Art and Design) Network. In 2013, he served as a NASA crew commander for a four-month Mars-on-Earth mission, isolated in a geometric biodome with five others. "There are parallels to the individual psychological experience, but from an operational standpoint, it is too different. You don't need a spacesuit, aren't threatened by a thin atmosphere or worried about being overpowered by radiation."
Outside threats aside, we have a bigger experience gap: Most of us didn't see this pandemic coming and weren't trained to survive the current new normal. NASA astronauts get at least two years of basic training. We received none. Intergalactic explorers understand gravity, air pressure, and other important criteria based on decades of space knowledge. Alternatively, new novel coronavirus data is coming in real time, changing the threats, precautions, and needs dramatically. Things feel a little different when you're winging it.
Lastly, with respect to Apollo 13, space travelers have a timeline for when their experience will be over. There are mishaps, challenges and adjustments, but every well-supported journeyperson leaves Earth with an agenda (and a team back home to help keep them on track).
The pandemic, on the other hand, has no definitive end. It is unclear when a reliable vaccine will be readily available. It is also not known how long we should shelter-in-place, as pulling the trigger too early could bring another wave of illness. We are missing definitive milestones, which, Vermeulen says, would make our isolation experience easier to navigate. "When you're on a mission, the end date is always on the horizon. You can celebrate the midpoint and check off major milestones, which helps."
Also, unlike a kid pretending to be in a rocket, most of us didn't dream of one day being socially isolated for an indeterminate amount of time. "If you're ambitious and working in the field, then it is your goal in life to experience [space and the related isolation]," he says. "With the pandemic, though, nobody chose to do this."
[Editor's Note: This article was originally published on June 8th, 2020 as part of a standalone magazine called GOOD10: The Pandemic Issue. Produced as a partnership among LeapsMag, The Aspen Institute, and GOOD, the magazine is available for free online.]
As We Wait for a Vaccine, Scientists Work to Scale Up the Best COVID-19 Antibodies to Give New Patients
In this illustration of immune defense, Y-shaped proteins called antibodies attack a virus.
When we get sick, our immune system sends its soldier cells to the battlefield. Called B-cells, they "examine" the foreign particles that shouldn't be in our bloodstream—and start producing the antibodies, the proteins to neutralize the invaders.
To screen the antibodies, scientists have developed a proprietary way to make the effective ones glow – like a literal "lightbulb" moment.
The better these antibodies are at neutralizing the pathogen, the faster we recover.
The antibodies acquired from COVID-19 survivors already showed promise in treating other patients, but because they must be obtained from people, generating a regular supply is not feasible. To close the gap, researchers are trying to identify the B-cells that make the best antibodies—and then farm them in laboratories at scale.
Scientists at Berkley Lights, a biotechnology company in California, have been screening B-cells from recovered patients and testing the antibodies they release for virus-neutralizing abilities. To screen the antibodies, scientists there have developed a proprietary way to make the effective ones glow – like a literal "lightbulb" moment.
So how does it work? First, the individual B-cells are placed into microscopic chambers called nano-pens, where they secrete the antibodies. Once released, the antibodies are flushed over tiny beads that have bits of the viral particles attached to them, along with special molecules that can emit fluorescent light.
"When an antibody binds to the bead, we see a bright light on the bead," explains John Proctor, the company's senior vice president of antibody therapeutics. "So we can identify which cells are making the antibodies."
Then the antibodies are tested for their ability to counteract the coronavirus's spike proteins, which the virus uses to break into our cells. Not all antibodies are equally good at this crucial defense move—some can block only parts of the virus's machinery, while others can neutralize it completely. Proctor and his colleagues are looking for the latter.
Once scientists identify the best performing B-cells, they crack the cells open—or in scientific terms "lyse" them—and extract the genetic instructions for making the antibodies. As it turns out, B-cells aren't very efficient at pumping out massive amounts of antibodies, so scientists insert these genetic instructions into a different, more prolific type of cell.
Named Chinese Hamster Ovary Cells or CHO, these cells are commonly used in the pharmaceutical industry because they can generate therapeutic proteins en masse. Under the right nutrient conditions, which include a lot of sugar, CHO cells can keep making the antibodies at commercial levels. "They are engineered to operate in very large bioreactors," Proctor explains.
While traditional antibody screening can take three months, the Beacon System can do it in less than 24 hours.
Berkeley Lights' technology has already been used to screen the antibodies of recovered patients from Vanderbilt University Medical Center. In another example, a biotech company GenScript ProBio used the platform to screen mice engineered to have human antibodies for the coronavirus.
In addition to its small, lab-on-a-chip size, Berkeley Lights' system allows scientists to greatly speed up the screening process. While traditional antibody screening can take three months, the Beacon System can do it in less than 24 hours. "We only need one B-cell per pen and a couple of beads to see that fluorescent signal," Proctor says. "It is a more advanced way to process and analyze cells, and that level of sensitivity is unique to our technology."
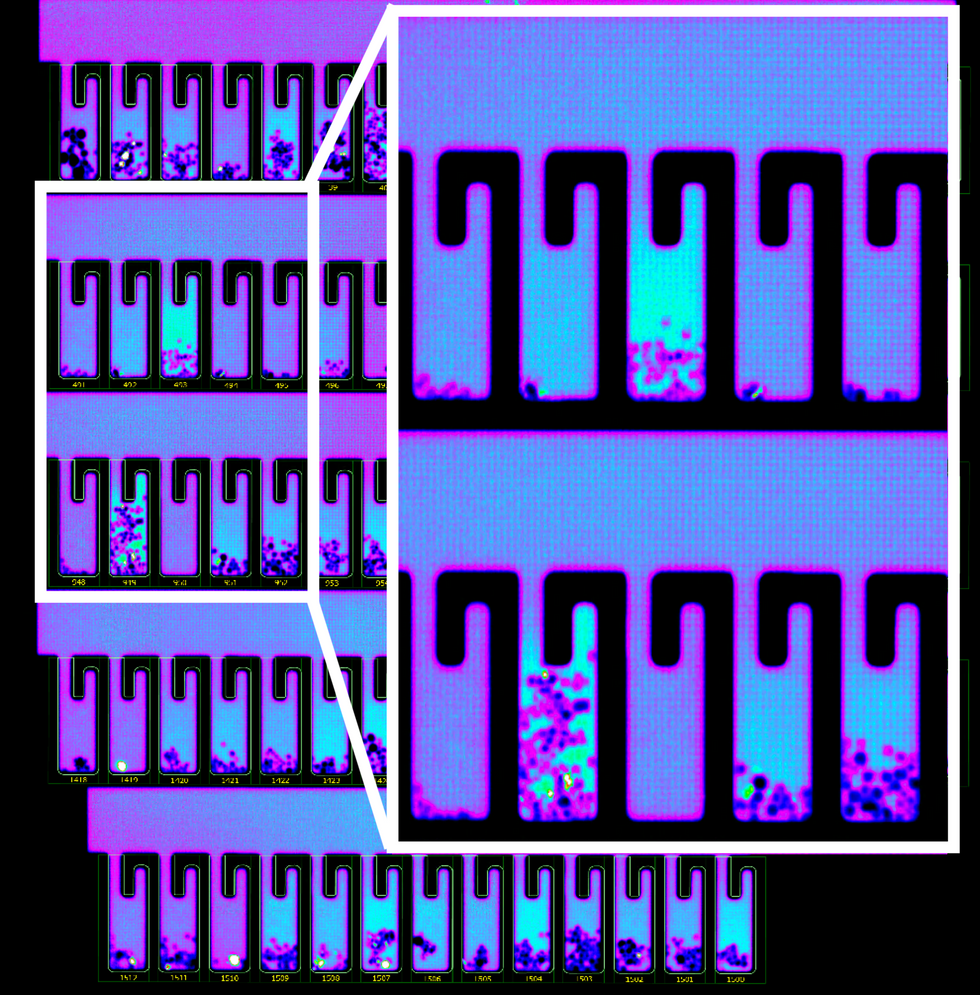
B-cells secreting antibodies inside the Berkeley Lights Beacon System Nano-Pens.
While vaccines are likely to take months to develop and test, antibodies might arrive to the battleground sooner. With the extremely limited treatment options for COVID-19, antibody-based therapeutics can potentially bridge this gap.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.


