Researchers Behaving Badly: Known Frauds Are "the Tip of the Iceberg"

Disgraced stem cell researcher and celebrity surgeon Paolo Macchiarini.
Last week, the whistleblowers in the Paolo Macchiarini affair at Sweden's Karolinska Institutet went on the record here to detail the retaliation they suffered for trying to expose a star surgeon's appalling research misconduct.
Scientific fraud of the type committed by Macchiarini is rare, but studies suggest that it's on the rise.
The whistleblowers had discovered that in six published papers, Macchiarini falsified data, lied about the condition of patients and circumvented ethical approvals. As a result, multiple patients suffered and died. But Karolinska turned a blind eye for years.
Scientific fraud of the type committed by Macchiarini is rare, but studies suggest that it's on the rise. Just this week, for example, Retraction Watch and STAT together broke the news that a Harvard Medical School cardiologist and stem cell researcher, Piero Anversa, falsified data in a whopping 31 papers, which now have to be retracted. Anversa had claimed that he could regenerate heart muscle by injecting bone marrow cells into damaged hearts, a result that no one has been able to duplicate.
A 2009 study published in the Public Library of Science (PLOS) found that about two percent of scientists admitted to committing fabrication, falsification or plagiarism in their work. That's a small number, but up to one third of scientists admit to committing "questionable research practices" that fall into a gray area between rigorous accuracy and outright fraud.
These dubious practices may include misrepresentations, research bias, and inaccurate interpretations of data. One common questionable research practice entails formulating a hypothesis after the research is done in order to claim a successful premise. Another highly questionable practice that can shape research is ghost-authoring by representatives of the pharmaceutical industry and other for-profit fields. Still another is gifting co-authorship to unqualified but powerful individuals who can advance one's career. Such practices can unfairly bolster a scientist's reputation and increase the likelihood of getting the work published.
The above percentages represent what scientists admit to doing themselves; when they evaluate the practices of their colleagues, the numbers jump dramatically. In a 2012 study published in the Journal of Research in Medical Sciences, researchers estimated that 14 percent of other scientists commit serious misconduct, while up to 72 percent engage in questionable practices. While these are only estimates, the problem is clearly not one of just a few bad apples.
In the PLOS study, Daniele Fanelli says that increasing evidence suggests the known frauds are "just the 'tip of the iceberg,' and that many cases are never discovered" because fraud is extremely hard to detect.
Essentially everyone wants to be associated with big breakthroughs, and they may overlook scientifically shaky foundations when a major advance is claimed.
In addition, it's likely that most cases of scientific misconduct go unreported because of the high price of whistleblowing. Those in the Macchiarini case showed extraordinary persistence in their multi-year campaign to stop his deadly trachea implants, while suffering serious damage to their careers. Such heroic efforts to unmask fraud are probably rare.
To make matters worse, there are numerous players in the scientific world who may be complicit in either committing misconduct or covering it up. These include not only primary researchers but co-authors, institutional executives, journal editors, and industry leaders. Essentially everyone wants to be associated with big breakthroughs, and they may overlook scientifically shaky foundations when a major advance is claimed.
Another part of the problem is that it's rare for students in science and medicine to receive an education in ethics. And studies have shown that older, more experienced and possibly jaded researchers are more likely to fudge results than their younger, more idealistic colleagues.
So, given the steep price that individuals and institutions pay for scientific misconduct, what compels them to go down that road in the first place? According to the JRMS study, individuals face intense pressures to publish and to attract grant money in order to secure teaching positions at universities. Once they have acquired positions, the pressure is on to keep the grants and publishing credits coming in order to obtain tenure, be appointed to positions on boards, and recruit flocks of graduate students to assist in research. And not to be underestimated is the human ego.
Paolo Macchiarini is an especially vivid example of a scientist seeking not only fortune, but fame. He liberally (and falsely) claimed powerful politicians and celebrities, even the Pope, as patients or admirers. He may be an extreme example, but we live in an age of celebrity scientists who bring huge amounts of grant money and high prestige to the institutions that employ them.
The media plays a significant role in both glorifying stars and unmasking frauds. In the Macchiarini scandal, the media first lifted him up, as in NBC's laudatory documentary, "A Leap of Faith," which painted him as a kind of miracle-worker, and then brought him down, as in the January 2016 documentary, "The Experiments," which chronicled the agonizing death of one of his patients.
Institutions can also play a crucial role in scientific fraud by putting more emphasis on the number and frequency of papers published than on their quality. The whole course of a scientist's career is profoundly affected by something called the h-index. This is a number based on both the frequency of papers published and how many times the papers are cited by other researchers. Raising one's ranking on the h-index becomes an overriding goal, sometimes eclipsing the kind of patient, time-consuming research that leads to true breakthroughs based on reliable results.
Universities also create a high-pressured environment that encourages scientists to cut corners. They, too, place a heavy emphasis on attracting large monetary grants and accruing fame and prestige. This can lead them, just as it led Karolinska, to protect a star scientist's sloppy or questionable research. According to Dr. Andrew Rosenberg, who is director of the Center for Science and Democracy at the U.S.-based Union of Concerned Scientists, "Karolinska defended its investment in an individual as opposed to the long-term health of the institution. People were dying, and they should have outsourced the investigation from the very beginning."
Having institutions investigate their own practices is a conflict of interest from the get-go, says Rosenberg.
Scientists, universities, and research institutions are also not immune to fads. "Hot" subjects attract grant money and confer prestige, incentivizing scientists to shift their research priorities in a direction that garners more grants. This can mean neglecting the scientist's true area of expertise and interests in favor of a subject that's more likely to attract grant money. In Macchiarini's case, he was allegedly at the forefront of the currently sexy field of regenerative medicine -- a field in which Karolinska was making a huge investment.
The relative scarcity of resources intensifies the already significant pressure on scientists. They may want to publish results rapidly, since they face many competitors for limited grant money, academic positions, students, and influence. The scarcity means that a great many researchers will fail while only a few succeed. Once again, the temptation may be to rush research and to show it in the most positive light possible, even if it means fudging or exaggerating results.
Though the pressures facing scientists are very real, the problem of misconduct is not inevitable.
Intense competition can have a perverse effect on researchers, according to a 2007 study in the journal Science of Engineering and Ethics. Not only does it place undue pressure on scientists to succeed, it frequently leads to the withholding of information from colleagues, which undermines a system in which new discoveries build on the previous work of others. Researchers may feel compelled to withhold their results because of the pressure to be the first to publish. The study's authors propose that more investment in basic research from governments could alleviate some of these competitive pressures.
Scientific journals, although they play a part in publishing flawed science, can't be expected to investigate cases of suspected fraud, says the German science blogger Leonid Schneider. Schneider's writings helped to expose the Macchiarini affair.
"They just basically wait for someone to retract problematic papers," he says.
He also notes that, while American scientists can go to the Office of Research Integrity to report misconduct, whistleblowers in Europe have no external authority to whom they can appeal to investigate cases of fraud.
"They have to go to their employer, who has a vested interest in covering up cases of misconduct," he says.
Science is increasingly international. Major studies can include collaborators from several different countries, and he suggests there should be an international body accessible to all researchers that will investigate suspected fraud.
Ultimately, says Rosenberg, the scientific system must incorporate trust. "You trust co-authors when you write a paper, and peer reviewers at journals trust that scientists at research institutions like Karolinska are acting with integrity."
Without trust, the whole system falls apart. It's the trust of the public, an elusive asset once it has been betrayed, that science depends upon for its very existence. Scientific research is overwhelmingly financed by tax dollars, and the need for the goodwill of the public is more than an abstraction.
The Macchiarini affair raises a profound question of trust and responsibility: Should multiple co-authors be held responsible for a lead author's misconduct?
Karolinska apparently believes so. When the institution at last owned up to the scandal, it vindictively found Karl Henrik-Grinnemo, one of the whistleblowers, guilty of scientific misconduct as well. It also designated two other whistleblowers as "blameworthy" for their roles as co-authors of the papers on which Macchiarini was the lead author.
As a result, the whistleblowers' reputations and employment prospects have become collateral damage. Accusations of research misconduct can be a career killer. Research grants dry up, employment opportunities evaporate, publishing becomes next to impossible, and collaborators vanish into thin air.
Grinnemo contends that co-authors should only be responsible for their discrete contributions, not for the data supplied by others.
"Different aspects of a paper are highly specialized," he says, "and that's why you have multiple authors. You cannot go through every single bit of data because you don't understand all the parts of the article."
This is especially true in multidisciplinary, translational research, where there are sometimes 20 or more authors. "You have to trust co-authors, and if you find something wrong you have to notify all co-authors. But you couldn't go through everything or it would take years to publish an article," says Grinnemo.
Though the pressures facing scientists are very real, the problem of misconduct is not inevitable. Along with increased support from governments and industry, a change in academic culture that emphasizes quality over quantity of published studies could help encourage meritorious research.
But beyond that, trust will always play a role when numerous specialists unite to achieve a common goal: the accumulation of knowledge that will promote human health, wealth, and well-being.
[Correction: An earlier version of this story mistakenly credited The New York Times with breaking the news of the Anversa retractions, rather than Retraction Watch and STAT, which jointly published the exclusive on October 14th. The piece in the Times ran on October 15th. We regret the error.]
Why you should (virtually) care
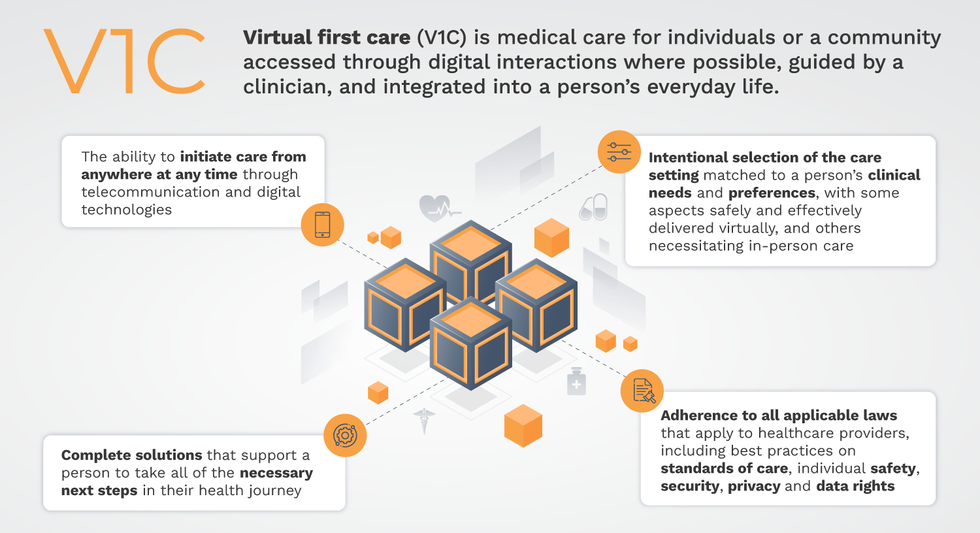
Virtual-first care, or V1C, could increase the quality of healthcare and make it more patient-centric by letting patients combine in-person visits with virtual options such as video for seeing their care providers.
As the pandemic turns endemic, healthcare providers have been eagerly urging patients to return to their offices to enjoy the benefits of in-person care.
But wait.
The last two years have forced all sorts of organizations to be nimble, adaptable and creative in how they work, and this includes healthcare providers’ efforts to maintain continuity of care under the most challenging of conditions. So before we go back to “business as usual,” don’t we owe it to those providers and ourselves to admit that business as usual did not work for most of the people the industry exists to help? If we’re going to embrace yet another period of change – periods that don’t happen often in our complex industry – shouldn’t we first stop and ask ourselves what we’re trying to achieve?
Certainly, COVID has shown that telehealth can be an invaluable tool, particularly for patients in rural and underserved communities that lack access to specialty care. It’s also become clear that many – though not all – healthcare encounters can be effectively conducted from afar. That said, the telehealth tactics that filled the gap during the pandemic were largely stitched together substitutes for existing visit-based workflows: with offices closed, patients scheduled video visits for help managing the side effects of their blood pressure medications or to see their endocrinologist for a quarterly check-in. Anyone whose children slogged through the last year or two of remote learning can tell you that simply virtualizing existing processes doesn’t necessarily improve the experience or the outcomes!
But what if our approach to post-pandemic healthcare came from a patient-driven perspective? We have a fleeting opportunity to advance a care model centered on convenient and equitable access that first prioritizes good outcomes, then selects approaches to care – and locations – tailored to each patient. Using the example of education, imagine how effective it would be if each student, regardless of their school district and aptitude, received such individualized attention.
That’s the idea behind virtual-first care (V1C), a new care model centered on convenient, customized, high-quality care that integrates a full suite of services tailored directly to patients’ clinical needs and preferences. This package includes asynchronous communication such as texting; video and other live virtual modes; and in-person options.
V1C goes beyond what you might think of as standard “telehealth” by using evidence-based protocols and tools that include traditional and digital therapeutics and testing, personalized care plans, dynamic patient monitoring, and team-based approaches to care. This could include spit kits mailed for laboratory tests and complementing clinical care with health coaching. V1C also replaces some in-person exams with ongoing monitoring, using sensors for more ‘whole person’ care.
Amidst all this momentum, we have the opportunity to rethink the goals of healthcare innovation, but that means bringing together key stakeholders to demonstrate that sustainable V1C can redefine healthcare.
Established V1C healthcare providers such as Omada, Headspace, and Heartbeat Health, as well as emerging market entrants like Oshi, Visana, and Wellinks, work with a variety of patients who have complicated long-term conditions such as diabetes, heart failure, gastrointestinal illness, endometriosis, and COPD. V1C is comprehensive in ways that are lacking in digital health and its other predecessors: it has the potential to integrate multiple data streams, incorporate more frequent touches and check-ins over time, and manage a much wider range of chronic health conditions, improving lives and reducing disease burden now and in the future.
Recognizing the pandemic-driven interest in virtual care, significant energy and resources are already flowing fast toward V1C. Some of the world’s largest innovators jumped into V1C early on: Verily, Alphabet’s Life Sciences Company, launched Onduo in 2016 to disrupt the diabetes healthcare market, and is now well positioned to scale its solutions. Major insurers like Aetna and United now offer virtual-first plans to members, responding as organizations expand virtual options for employees. Amidst all this momentum, we have the opportunity to rethink the goals of healthcare innovation, but that means bringing together key stakeholders to demonstrate that sustainable V1C can redefine healthcare.
That was the immediate impetus for IMPACT, a consortium of V1C companies, investors, payers and patients founded last year to ensure access to high-quality, evidence-based V1C. Developed by our team at the Digital Medicine Society (DiMe) in collaboration with the American Telemedicine Association (ATA), IMPACT has begun to explore key issues that include giving patients more integrated experiences when accessing both virtual and brick-and-mortar care.
Digital Medicine Society
V1C is not, nor should it be, virtual-only care. In this new era of hybrid healthcare, success will be defined by how well providers help patients navigate the transitions. How do we smoothly hand a patient off from an onsite primary care physician to, say, a virtual cardiologist? How do we get information from a brick-and-mortar to a digital portal? How do you manage dataflow while still staying HIPAA compliant? There are many complex regulatory implications for these new models, as well as an evolving landscape in terms of privacy, security and interoperability. It will be no small task for groups like IMPACT to determine the best path forward.
None of these factors matter unless the industry can recruit and retain clinicians. Our field is facing an unprecedented workforce crisis. Traditional healthcare is making clinicians miserable, and COVID has only accelerated the trend of overworked, disenchanted healthcare workers leaving in droves. Clinicians want more interactions with patients, and fewer with computer screens – call it “More face time, less FaceTime.” No new model will succeed unless the industry can more efficiently deploy its talent – arguably its most scarce and precious resource. V1C can help with alleviating the increasing burden and frustration borne by individual physicians in today’s status quo.
In healthcare, new technological approaches inevitably provoke no shortage of skepticism. Past lessons from Silicon Valley-driven fixes have led to understandable cynicism. But V1C is a different breed of animal. By building healthcare around the patient, not the clinic, V1C can make healthcare work better for patients, payers and providers. We’re at a fork in the road: we can revert back to a broken sick-care system, or dig in and do the hard work of figuring out how this future-forward healthcare system gets financed, organized and executed. As a field, we must find the courage and summon the energy to embrace this moment, and make it a moment of change.
Podcast: The future of brain health with Percy Griffin
Percy Griffin, director of scientific engagement for the Alzheimer’s Association, joins Leaps.org to discuss the present and future of the fight against dementia.
Today's guest is Percy Griffin, director of scientific engagement for the Alzheimer’s Association, a nonprofit that’s focused on speeding up research, finding better ways to detect Alzheimer’s earlier and other approaches for reducing risk. Percy has a doctorate in molecular cell biology from Washington University, he’s led important research on Alzheimer’s, and you can find the link to his full bio in the show notes, below.
Our topic for this conversation is the present and future of the fight against dementia. Billions of dollars have been spent by the National Institutes of Health and biotechs to research new treatments for Alzheimer's and other forms of dementia, but so far there's been little to show for it. Last year, Aduhelm became the first drug to be approved by the FDA for Alzheimer’s in 20 years, but it's received a raft of bad publicity, with red flags about its effectiveness, side effects and cost.
Meanwhile, 6.5 million Americans have Alzheimer's, and this number could increase to 13 million in 2050. Listen to this conversation if you’re concerned about your own brain health, that of family members getting older, or if you’re just concerned about the future of this country with experts predicting the number people over 65 will increase dramatically in the very near future.
Listen to the Episode
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
4:40 - We talk about the parts of Percy’s life that led to him to concentrate on working in this important area.
6:20 - He defines Alzheimer's and dementia, and discusses the key elements of communicating science.
10:20 - Percy explains why the Alzheimer’s Association has been supportive of Aduhelm, even as others have been critical.
17:58 - We talk about therapeutics under development, which ones to be excited about, and how they could be tailored to a person's own biology.
24:25 - Percy discusses funding and tradeoffs between investing more money into Alzheimer’s research compared to other intractable diseases like cancer, and new opportunities to accelerate progress, such as ARPA-H, President Biden’s proposed agency to speed up health breakthroughs.
27:24 - We talk about the social determinants of brain health. What are the pros/cons of continuing to spend massive sums of money to develop new drugs like Aduhelm versus refocusing on expanding policies to address social determinants - like better education, nutritious food and safe drinking water - that have enabled some groups more than others to enjoy improved cognition late in life.
34:18 - Percy describes his top lifestyle recommendations for protecting your mind.
37:33 - Is napping bad for the brain?
39:39 - Circadian rhythm and Alzheimer's.
42:34 - What tests can people take to check their brain health today, and which biomarkers are we making progress on?
47:25 - Percy highlights important programs run by the Alzheimer’s Association to support advances.
Show links:
** After this episode was recorded, the Centers for Medicare and Medicaid Services affirmed its decision from last June to limit coverage of Aduhelm. More here.
- Percy Griffin's bio: https://www.alz.org/manh/events/alztalks/upcoming-...
- The Alzheimer's Association's Part the Cloud program: https://alz.org/partthecloud/about-us.asp
- The paradox of dementia rates decreasing: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7455342/
- The argument for focusing more resources on improving institutions and social processes for brain health: https://www.statnews.com/2021/09/23/the-brain-heal...
- Recent research on napping: https://www.ocregister.com/2022/03/25/alzheimers-s...
- The Alzheimer's Association helpline: https://www.alz.org/help-support/resources/helpline
- ALZConnected, a free online community for people affected by dementia https://www.alzconnected.org/
- TrialMatch for people with dementia and healthy volunteers to find clinical trials for Alzheimer's and other dementia: https://www.alz.org/alzheimers-dementia/research_p...

