Too much of this ingredient leads to autoimmune diseases, new research shows. Here's how to cut back.

Scientists are looking at how salt affects our cells, and they're finding more reasons to avoid htoo much of it.
For more than a century, doctors have warned that too much salt in your diet can lead to high blood pressure, heart disease and stroke - and many of the reasons for these effects are well known. But recently scientists have been looking deeper, into the cellular level, and they are finding additional reasons to minimize sodium intake; it is bad for immune cells, creating patterns of gene expression and activity seen in a variety of autoimmune diseases such as multiple sclerosis, lupus, rheumatoid arthritis, and type-1 diabetes.
Salt is a major part of the ocean from which life evolved on this planet. We carry that legacy in our blood, which tastes salty. It is an important element for conducting electrical signals along nerves and balancing water and metabolites transported throughout our bodies. We need to consume about 500 milligrams of salt each day to maintain these functions, more with exercise and heavy sweating as that is a major way the body loses salt. The problem is that most Americans eating a modern western diet consume about 3400 milligrams, 1.5 teaspoons per day.
Evidence has been accumulating over the last few years that elevated levels of sodium can be harmful to at least some types of immune cells. The first signal came in monocytes, which are immune cells that travel to various tissues in the body, where some of them turn into macrophages, a subset of white blood cells that can directly kill microorganisms and make chemical signals that bring other types of immune cells into play.
Two years ago, Dominik N. Müller from the Max-Delbrueck-Center in Berlin, Germany and Markus Kleinewietfeld, an immunologist at Hasselt University in Belgium, ran a study where they fed people pizza and then measured their immune cell function. “We saw that in any monocytes, metabolic function was down, even after a single salty meal,” Kleinewietfeld says. It seemed to be the cellular equivalent of the sluggish feeling we get after eating too much. The cells were able to recover but more research is needed to answer questions about what dose of sodium causes impairment, how long the damage lasts, and whether there is a cumulative effect of salt toxicity.
Kleinewietfeld and his colleagues have hypothesized that too much salt could be a significant factor in the increased number of autoimmune diseases and allergies over the last few generations.
The latest series of experiments focused on a type of T cell called T regulatory cells, or Tregs. Most T cells release inflammatory mediators to fight pathogens and, once that job is done, Tregs come along to calm down their hyperactive brethren. Failure to do so can result in continued inflammation and possibly autoimmune diseases.
In the lab, Kleinewietfeld and his large team of international collaborators saw that high levels of sodium had a huge effect on Tregs, upregulating 1250 genes and downregulating an additional 1380 genes so that they looked similar to patterns of gene expression seen in autoimmune diseases.
Digging deeper, they found that sodium affected mitochondria, the tiny organelles inside of cells that produce much of its energy. The sodium was interfering with how the mitochondria use oxygen, which resulted in increased levels of an unstable form of oxygen that can damage cell function. The researchers injected those damaged Tregs into mice and found that they impaired the animals' immune function, allowing the inflammation to continue rather than shutting it down.
That finding dovetailed nicely with a 2019 paper in Nature from Navdeep Chandel's lab at Northwestern University, which showed in mice that inhibiting the mitochondrial use of oxygen reduced the ability of Tregs to regulate other T cells. “Mitochondria were controlling directly the immunosuppressive program, they were this master regulator tuning the right amount of genes to give you proper immunosuppression,” Chandel said. “And if you lose that function, then you get autoimmunity.”
Kleinewietfeld's team studied the Treg cells of humans and found that sodium can similarly decrease mitochondrial use of oxygen and immunosuppressive activity. “I would have never predicted that myself,” Chandel says, but now researchers can look at the mitochondria of patients with autoimmune disease and see if their gene expression also changes under high salt conditions. He sees the link between the patterns of gene expression in Tregs generated by high salt exposure and those patterns seen in autoimmune diseases, but he is cautious about claiming a causal effect.
Kleinewietfeld and his colleagues have hypothesized that too much salt could be a significant factor in the increased number of autoimmune diseases and allergies over the last few generations. He says a high salt diet could also have an indirect effect on immune function through the way it affects the gut microbiome and the molecules made by microbes when they break down food. But the research results are too preliminary to say that for sure, much less parse out the role of salt compared with other possible factors. “It is still an exciting journey to try to understand this field,” he says.
Additionally, it is difficult to say precisely how this research in animals and human cell cultures will translate into a whole human body. Individual differences in genetics can affect how the body absorbs, transports, and gets rid of sodium, such that some people are more sensitive to salt than are others.
So how should people apply these research findings to daily life?
Salt is obvious when we sprinkle it on at the table or eat tasty things like potato chips, but we may be unaware of sodium hidden in packaged foods. That's because salt is an easy and cheap way to boost the flavor of foods. And if we do read the labeled salt content on a package, we focus on the number for a single serving, but then eat more than that.
Last September, the U.S. Food and Drug Administration (FDA) began a process to update labels on the content of food, including what is meant by the word “healthy” and how food manufacturers can use the term. Many in the food industry are resisting those proposed changes.
Chandel cautions against trying to counter the effects of salt by reaching for foods or supplements full of antioxidants, which, in theory, could reduce the harmful effects on mitochondria caused by a heavy hand with the salt shaker.
Until labels are updated, it would be prudent to try to reduce sodium intake by cutting down on packaged foods while making your own food at home, where you know just how much salt has been added. The Mayo Clinic offers guidance on how to become more aware of the sodium in your diet and eat less of it.
Chandel thinks many people will struggle with minimizing salt in their diets. It’s similar to the challenge of eating less sugar, in that the body craves both, and it is difficult to fight that. He cautions against trying to counter the effects of salt by reaching for foods or supplements full of antioxidants, which, in theory, could reduce the harmful effects on mitochondria caused by a heavy hand with the salt shaker. “Dietary antioxidants have failed in just about every clinical trial, yet the public continues to take them,” Chandel says. But he is optimistic that research will lead us to a better understanding of how Tregs function, and uncover new targets for treating autoimmune diseases.
New gene therapy helps patients with rare disease. One mother wouldn't have it any other way.
A biotech in Cambridge, Mass., is targeting a rare disease called cystinosis with gene therapy. It's been effective for five patients in a clinical trial that's still underway.
Three years ago, Jordan Janz of Consort, Alberta, knew his gene therapy treatment for cystinosis was working when his hair started to darken. Pigmentation or melanin production is just one part of the body damaged by cystinosis.
“When you have cystinosis, you’re either a redhead or a blonde, and you are very pale,” attests Janz, 23, who was diagnosed with the disease just eight months after he was born. “After I got my new stem cells, my hair came back dark, dirty blonde, then it lightened a little bit, but before it was white blonde, almost bleach blonde.”
According to Cystinosis United, about 500 to 600 people have the rare genetic disease in the U.S.; an estimated 20 new cases are diagnosed each year.
Located in Cambridge, Mass., AVROBIO is a gene therapy company that targets cystinosis and other lysosomal storage disorders, in which toxic materials build up in the cells. Janz is one of five patients in AVROBIO’s ongoing Phase 1/2 clinical trial of a gene therapy for cystinosis called AVR-RD-04.
Recently, AVROBIO compiled positive clinical data from this first and only gene therapy trial for the disease. The data show the potential of the therapy to genetically modify the patients’ own hematopoietic stem cells—a certain type of cell that’s capable of developing into all different types of blood cells—to express the functional protein they are deficient in. It stabilizes or reduces the impact of cystinosis on multiple tissues with a single dose.
Medical researchers have found that more than 80 different mutations to a gene called CTNS are responsible for causing cystinosis. The most common mutation results in a deficiency of the protein cystinosin. That protein functions as a transporter that regulates a lot metabolic processes in the cells.
“One of the first things we see in patients clinically is an accumulation of a particular amino acid called cystine, which grows toxic cystine crystals in the cells that cause serious complications,” explains Essra Rihda, chief medical officer for AVROBIO. “That happens in the cells across the tissues and organs of the body, so the disease affects many parts of the body.”

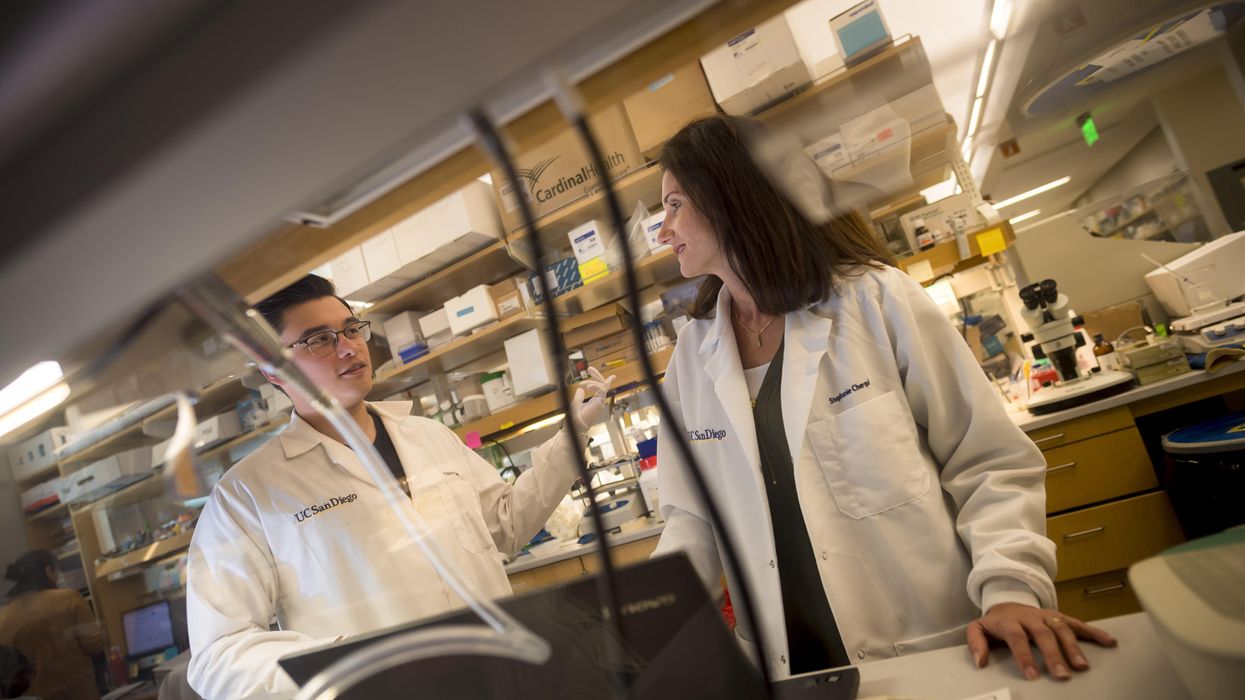
Jordan Janz, 23, meets Stephanie Cherqui, the principal investigator of his gene therapy trial, before the trial started in 2019.
Jordan Janz
According to Rihda, although cystinosis can occur in kids and adults, the most severe form of the disease affects infants and makes up about 95 percent of overall cases. Children typically appear healthy at birth, but around six to 18 months, they start to present for medical attention with failure to thrive.
Additionally, infants with cystinosis often urinate frequently, a sign of polyuria, and they are thirsty all the time, since the disease usually starts in the kidneys. Many develop chronic kidney disease that ultimately progresses to the point where the kidney no longer supports the body’s needs. At that stage, dialysis is required and then a transplant. From there the disease spreads to many other organs, including the eyes, muscles, heart, nervous system, etc.
“The gene for cystinosis is expressed in every single tissue we have, and the accumulation of this toxic buildup alters all of the organs of the patient, so little by little all of the organs start to fail,” says Stephanie Cherqui, principal investigator of Cherqui Lab, which is part of UC San Diego’s Department of Pediatrics.
Since the 1950s, a drug called cysteamine showed some therapeutic effect on cystinosis. It was approved by the FDA in 1994 to prevent damage that may be caused by the buildup of cystine crystals in organs. Prior to FDA approval, Cherqui says, children were dying of the disease before they were ten-years-old or after a kidney transplant. By taking oral cysteamine, they can live from 20 to 50 years longer. But it’s a challenging drug because it has to be taken every 6 or 12 hours, and there are serious gastric side effects such as nausea and diarrhea.
“With all of the complications they develop, the typical patient takes 40 to 60 pills a day around the clock,” Cherqui says. “They literally have a suitcase of medications they have to carry everywhere, and all of those medications don’t stop the progression of the disease, and they still die from it.”
Cherqui has been a proponent of gene therapy to treat children’s disorders since studying cystinosis while earning her doctorate in 2002. Today, her lab focuses on developing stem cell and gene therapy strategies for degenerative, hereditary disorders such as cystinosis that affect multiple systems of the body. “Because cystinosis expresses in every tissue in the body, I decided to use the blood-forming stem cells that we have in our bone marrow,” she explains. “These cells can migrate to anywhere in the body where the person has an injury from the disease.”
AVROBIO’s hematopoietic stem cell gene therapy approach collects stem cells from the patient’s bone marrow. They then genetically modify the stem cells to give the patient a copy of the healthy CTNS gene, which the person either doesn’t have or it’s defective.
The patient first undergoes apheresis, a medical procedure in which their blood is passed through an apparatus that separates out the diseased stem cells, and a process called conditioning is used to help eliminate the damaged cells so they can be replaced by the infusion of the patient’s genetically modified stem cells. Once they become engrafted into the patient’s bone marrow, they reproduce into a lot of daughter cells, and all of those daughter cells contain the CTNS gene. Those cells are able to express the healthy, functional, active protein throughout the body to correct the metabolic problem caused by cystinosis.
“What we’re seeing in the adult patients who have been dosed to date is the consistent and sustained engraftment of our genetically modified cells, 17 to 27 months post-gene therapy, so that’s very encouraging and positive,” says Rihda, the chief medical officer at AVROBIO.
When Janz was 11-years-old, his mother got him enrolled in the trial of a new form of cysteamine that would only need to be taken every 12 hours instead of every six. Two years later, she made sure he was the first person on the list for Cherqui’s current stem cell gene therapy trial.
AVROBIO researchers have also confirmed stabilization or improvement in motor coordination and visual perception in the trial participants, suggesting a potential impact on the neuropathology of the disease. Data from five dosed patients show strong safety and tolerability as well as reduced accumulation of cystine crystals in cells across multiple tissues in the first three patients. None of the five patients need to take oral cysteamine.
Janz’s mother, Barb Kulyk, whom he credits with always making him take his medications and keeping him hydrated, had been following Cherqui’s research since his early childhood. When Janz was 11-years-old, she got him enrolled in the trial of a new form of cysteamine that would only need to be taken every 12 hours instead of every six. When he was 17, the FDA approved that drug. Two years later, his mother made sure he was the first person on the list for Cherqui’s current stem cell gene therapy trial. He received his new stem cells on October 7th, 2019, went home in January 2020, and returned to working full time in February.

Jordan Janz, pictured here with his girlfriend, has a new lease on life, plus a new hair color.
Jordan Janz
He notes that his energy level is significantly better, and his mother has noticed much improvement in him and his daily functioning: He rarely vomits or gets nauseous in the morning, and he has more color in his face as well as his hair. Although he could finish his participation at any time, he recently decided to continue in the clinical trial.
Before the trial, Janz was taking 56 pills daily. He is completely off all of those medications and only takes pills to keep his kidneys working. Because of the damage caused by cystinosis over the course of his life, he’s down to about 20 percent kidney function and will eventually need a transplant.
“Some day, though, thanks to Dr. Cherqui’s team and AVROBIO’s work, when I get a new kidney, cystinosis won’t destroy it,” he concludes.
New study: Hotter nights, climate change, cause sleep loss with some affected more than others
According to a new study, sleep is impaired with temperatures over 50 degrees, and temps higher than 77 degrees reduce the chances of getting seven hours.
Data from the National Sleep Foundation finds that the optimal bedroom temperature for sleep is around 65 degrees Fahrenheit. But we may be getting fewer hours of "good sleepin’ weather" as the climate warms, according to a recent paper from researchers at the University of Copenhagen, Denmark.
Published in One Earth, the study finds that heat related to climate change could provide a “pathway” to sleep deprivation. The authors say the effect is “substantially larger” for those in lower-income countries. Hours of sleep decline when nighttime temperature exceeds 50 degrees, and temps higher than 77 reduce the chances of sleeping for seven hours by 3.5 percent. Even small losses associated with rising temperatures contribute significantly to people not getting enough sleep.
We’re affected by high temperatures at night because body temperature becomes more sensitive to the environment when slumbering. “Mechanisms that control for thermal regulation become more disordered during sleep,” explains Clete Kushida, a neurologist, professor of psychiatry at Stanford University and sleep medicine clinician.
The study finds that women and older adults are especially vulnerable. Worldwide, the elderly lost over twice as much sleep per degree of warming compared to younger people. This phenomenon was apparent between the ages of 60 and 70, and it increased beyond age 70. “The mechanism for balancing temperatures appears to be more affected with age,” Kushida adds.
Others disproportionately affected include those who live in regions with more greenhouse gas (GHG) emissions, which accelerate climate change, and people in hotter locales will lose more sleep per degree of warming, according to the study, with suboptimal temperatures potentially eroding 50 to 58 hours of sleep per person per year. One might think that those in warmer countries can adapt to the heat, but the researchers found no evidence for such adjustments. “We actually found those living in the warmest climate regions were impacted over twice as much as those in the coldest climate regions,” says the study's lead author, Kelton Minor, a Ph.D. candidate at the University of Copenhagen’s Center for Social Data Science.
Short sleep can reduce cognitive performance and productivity, increase absenteeism from work or school, and lead to a host of other physical and psychosocial problems. These issues include a compromised immune system, hypertension, depression, anger and suicide, say the study’s authors. According to a fact sheet by the U.S. Centers for Disease Control and Prevention, a third of U.S. adults already report sleeping fewer hours than the recommended amount, even though sufficient sleep “is not a luxury—it is something people need for good health.”
Equitable policy and planning are needed to ensure equal access to cooling technologies in a warming world.
Beyond global health, a sleep-deprived world will impact the economy as the climate warms. “Less productivity at work, associated with sleep loss or deprivation, would result in more sick days on a global scale, not just in individual countries,” Kushida says.
Unlike previous research that measured sleep patterns with self-reported surveys and controlled lab experiments, the study in One Earth offers a global analysis that relies on sleep-tracking wristbands that link more than seven million sleep records of 47,628 adults across 68 countries to local and daily meteorological data, offering new insight into the environmental impact on human sleep. Controlling for individual, seasonal and time-varying confounds, researchers found the main way that higher temperatures shorten slumber is by delaying sleep onset.
Heat effects on sleep were seen in industrialized countries including those with access to air conditioning, notes the study. Air conditioning may buffer high indoor temperatures, but they also increase GHG emissions and ambient heat displacement, thereby exacerbating the unequal burdens of global and local warming. Continued urbanization is expected to contribute to these problems.
Previous sleep studies have found an inverse U-shaped response to temperature in highly controlled settings, with subjects sleeping worse when room temperatures were either too cold or too warm. However, “people appear far better at adapting to colder outside temperatures than hotter conditions,” says Minor.
Although there are ways of countering the heat effect, some populations have more access to them. “Air conditioning can help with the effect of higher temperature, but not all individuals can afford air conditioners,” says Kushida. He points out that this could drive even greater inequity between higher- and lower-income countries.
Equitable policy and planning are needed to ensure equal access to cooling technologies in a warming world. “Clean and renewable energy systems and interventions will be needed to mitigate and adapt to ongoing climate warming,” Minor says. Future research should investigate “policy, planning and design innovation,” which could reduce the impact of sweltering temperatures on a good night’s sleep for the good of individuals, society and our planet, asserts the study.
Unabated and on its current trajectory, by 2099 suboptimal temperatures could shave 50 to 58 hours of sleep per person per year, predict the study authors. “Down the road, as technology develops, there might be ways of enabling people to adapt on a large scale to these higher temperatures,” says Kushida. “Right now, it’s not there.”