Scientists Attempt to Make Human Cells Resistant to Coronaviruses and Ebola
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.

Scientists are experimenting with turning certain genes on and off to make cells better fight viral infection.
Under the electronic microscope, the Ebola particles looked like tiny round bubbles floating inside human cells. Except these Ebola particles couldn't get free from their confinement.
They were trapped inside their bubbles, unable to release their RNA into the human cells to start replicating. These cells stopped the Ebola infection. And they did it on their own, without any medications, albeit in a petri dish of immunologist Adam Lacy-Hulbert. He studies how cells fight infections at the Benaroya Research Institute in Seattle, Washington.
These weren't just any ordinary human cells. They had a specific gene turned on—namely CD74, which typically wouldn't be on. Lacy-Hulbert's team was experimenting with turning various genes on and off to see what made cells fight viral infections better. One particular form of the CD74 gene did the trick. Normally, the Ebola particles would use the cells' own proteases—enzymes that are often called "molecular scissors" because they slice proteins—to cut the bubbles open. But CD74 produced a protein that blocked the scissors from cutting the bubbles, leaving Ebola trapped.
"When that gene turns on, it makes the protein that interferes with Ebola replication," Lacy-Hulbert says. "The protein binds to those molecular scissors and stops them from working." Even better, the protein interfered with coronaviruses too, including SARS-CoV-2, as the team published in the journal Science.
This begs the question: If one can turn on cells' viral resistance in a lab, can this be done in a human body so we that we can better fight Ebola, coronaviruses and other viral scourges?
Recent research indeed shows that our ability to fight viral infections is written in our genes. Genetic variability is at least one reason why some coronavirus-infected people don't develop symptoms while others stay on ventilators for weeks—often due to the aberrant response of their immune system, which went on overdrive to kill the pathogen. But if cells activate certain genes early in the infection, they might successfully stop viruses from replicating before the immune system spirals out of control.
"If my father who is 70 years old tests positive, I would recommend he takes interferon as early as possible."
When we talk about fighting infections, we tend to think in terms of highly specialized immune system cells—B-cells that release antibodies and T-cells that stimulate inflammatory responses, says Lacy-Hulbert. But all other cells in the body have the ability to fight infections too via different means. When cells detect the presence of a pathogen, they release interferons—small protein molecules named so because they set off a genetic chain reaction that interferes with viral replication. These molecules work as alarm signals to other cells around them. The neighboring cells transduce these signals inside themselves and turn on genes responsible for cellular defenses.
"There are at least 300 to 400 genes that are stimulated by type I interferons," says professor Jean-Laurent Casanova at Rockefeller University.
Scientists don't yet know exactly what all of these genes do, but they change the molecular behavior of the cells. "The cells go into a dramatic change and start producing hundreds of proteins that interfere with viral replication on the inside," explains Qian Zhang, a researcher at Casanova's lab. "Some block the proteins the virus needs and some physically tether the virus."
Some cells produce only small amount of interferon, enough to alert their neighbors. Others, such microphages and monocytes, whose jobs are to detect foreign invaders, produce a lot, injecting interferons into the blood to sound the alarm throughout the body. "They are professional cells so their jobs [are] to detect a viral or bacterial infection," Zhang explains.
People with impaired interferon responses are more vulnerable to infections, including influenza and coronaviruses. In two recent studies published in the journal Science, Casanova, Zhang and their colleagues found that patients who lacked a certain type of interferon had more severe Covid-19 symptoms and some died from it. The team ran a genetic comparison of blood samples from patients hospitalized with severe coronavirus cases against those with the asymptomatic infections.
They found that people with severe disease had rare variants in the 13 genes responsible for interferon production. More than three percent of them had a genetic mutation resulting in non-functioning genes. And over ten percent had an autoimmune condition, in which misguided antibodies neutralized their interferons, dampening their bodies' defenses—and these patients were predominantly men. These discoveries help explain why some young and seemingly healthy individuals require life support, while others have mild symptoms or none. The findings also offer ways of stimulating cellular resistance.
A New Frontier in the Making
The idea of making human cells genetically resistant to infections—and possibly other stressors like cancer or aging—has been considered before. It is the concept behind the Genome Project-write or GP-write project, which aims to create "ultra-safe" versions of human cells that resist a variety of pathogens by way of "recoding" or rewriting the cells' genes.
To build proteins, cells use combinations of three DNA bases called codons to represent amino acids—the proteins' building blocks. But biologists find that many of the codons are redundant so if they were removed from all genes, the human cells would still make all their proteins. However, the viruses, whose genes would still include these eliminated redundant codons, would no longer successfully be able to replicate inside human cells.
In 2016, the GP-Write team successfully reduced the number of Escherichia coli's codons from 64 to 57. Recoding genes in all human cells would be harder, but some recoded cells may be transplanted into the body, says Harvard Medical School geneticist George Church, the GP-Write core founding member.
"You can recode a subset of the body, such as all of your blood," he says. "You can also grow an organ inside a recoded pig and transplant it."
Church adds that these methods are still in stages that are too early to help us with this pandemic.
LeapsMag exclusively interviewed Church in 2019 about his latest progress with DNA recoding:
The Push for Clinical Trials
In the meantime, interferons may prove an easier medicine. Lacy-Hulbert thinks that interferon gamma might play a role in activating the CD74 gene, which gums up the molecular scissors. There also may be other ways to activate that gene. "So we are now thinking, can we develop a drug that mimics that actual activity?" he says.
Some interferons are already manufactured and used for treating certain diseases, including multiple sclerosis. Theoretically, nothing prevents doctors from prescribing interferons to Covid patients, but it must be done in the early stages of infection—to stimulate genes that trigger cellular defenses before the virus invades too many cells and before the immune systems mobilizes its big guns.
"If my father who is 70 years old tests positive, I would recommend he takes interferon as early as possible," says Zhang. But to make it a mainstream practice, doctors need clear prescription guidelines. "What would really help doctors make these decisions is clinical trials," says Casanova, so that such guidelines can be established. "We are now starting to push for clinical trials," he adds.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.
A robot server, controlled remotely by a disabled worker, delivers drinks to patrons at the DAWN cafe in Tokyo.
A sleek, four-foot tall white robot glides across a cafe storefront in Tokyo’s Nihonbashi district, holding a two-tiered serving tray full of tea sandwiches and pastries. The cafe’s patrons smile and say thanks as they take the tray—but it’s not the robot they’re thanking. Instead, the patrons are talking to the person controlling the robot—a restaurant employee who operates the avatar from the comfort of their home.
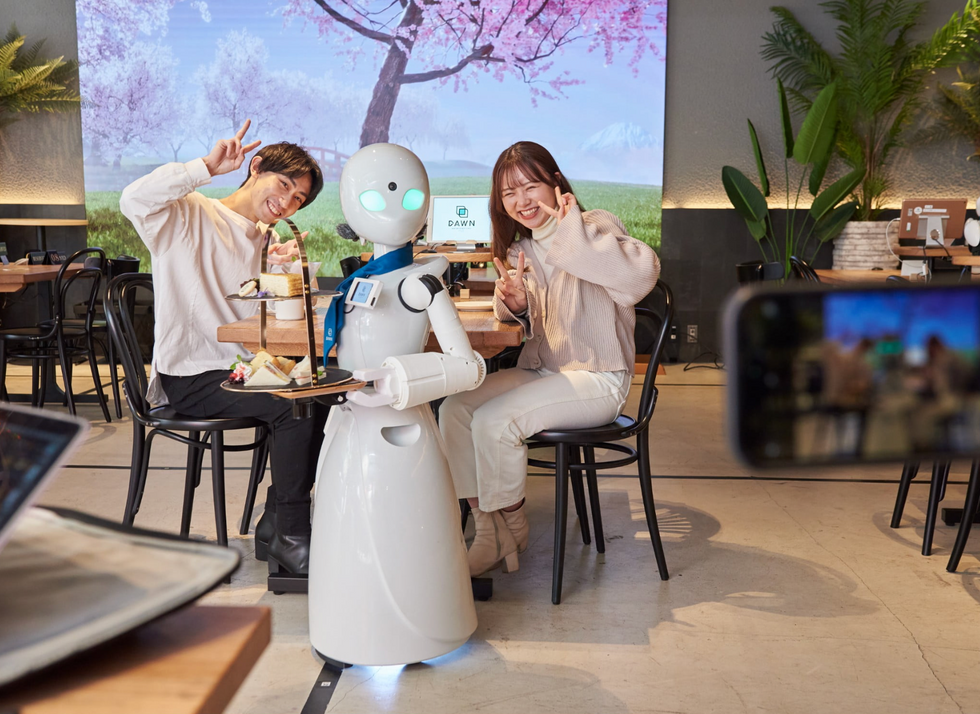
It’s a typical scene at DAWN, short for Diverse Avatar Working Network—a cafe that launched in Tokyo six years ago as an experimental pop-up and quickly became an overnight success. Today, the cafe is a permanent fixture in Nihonbashi, staffing roughly 60 remote workers who control the robots remotely and communicate to customers via a built-in microphone.
More than just a creative idea, however, DAWN is being hailed as a life-changing opportunity. The workers who control the robots remotely (known as “pilots”) all have disabilities that limit their ability to move around freely and travel outside their homes. Worldwide, an estimated 16 percent of the global population lives with a significant disability—and according to the World Health Organization, these disabilities give rise to other problems, such as exclusion from education, unemployment, and poverty.
These are all problems that Kentaro Yoshifuji, founder and CEO of Ory Laboratory, which supplies the robot servers at DAWN, is looking to correct. Yoshifuji, who was bedridden for several years in high school due to an undisclosed health problem, launched the company to help enable people who are house-bound or bedridden to more fully participate in society, as well as end the loneliness, isolation, and feelings of worthlessness that can sometimes go hand-in-hand with being disabled.
“It’s heartbreaking to think that [people with disabilities] feel they are a burden to society, or that they fear their families suffer by caring for them,” said Yoshifuji in an interview in 2020. “We are dedicating ourselves to providing workable, technology-based solutions. That is our purpose.”

Shota, Kuwahara, a DAWN employee with muscular dystrophy, agrees. "There are many difficulties in my daily life, but I believe my life has a purpose and is not being wasted," he says. "Being useful, able to help other people, even feeling needed by others, is so motivational."
A woman receives a mammogram, which can detect the presence of tumors in a patient's breast.
When a patient is diagnosed with early-stage breast cancer, having surgery to remove the tumor is considered the standard of care. But what happens when a patient can’t have surgery?
Whether it’s due to high blood pressure, advanced age, heart issues, or other reasons, some breast cancer patients don’t qualify for a lumpectomy—one of the most common treatment options for early-stage breast cancer. A lumpectomy surgically removes the tumor while keeping the patient’s breast intact, while a mastectomy removes the entire breast and nearby lymph nodes.
Fortunately, a new technique called cryoablation is now available for breast cancer patients who either aren’t candidates for surgery or don’t feel comfortable undergoing a surgical procedure. With cryoablation, doctors use an ultrasound or CT scan to locate any tumors inside the patient’s breast. They then insert small, needle-like probes into the patient's breast which create an “ice ball” that surrounds the tumor and kills the cancer cells.
Cryoablation has been used for decades to treat cancers of the kidneys and liver—but only in the past few years have doctors been able to use the procedure to treat breast cancer patients. And while clinical trials have shown that cryoablation works for tumors smaller than 1.5 centimeters, a recent clinical trial at Memorial Sloan Kettering Cancer Center in New York has shown that it can work for larger tumors, too.
In this study, doctors performed cryoablation on patients whose tumors were, on average, 2.5 centimeters. The cryoablation procedure lasted for about 30 minutes, and patients were able to go home on the same day following treatment. Doctors then followed up with the patients after 16 months. In the follow-up, doctors found the recurrence rate for tumors after using cryoablation was only 10 percent.
For patients who don’t qualify for surgery, radiation and hormonal therapy is typically used to treat tumors. However, said Yolanda Brice, M.D., an interventional radiologist at Memorial Sloan Kettering Cancer Center, “when treated with only radiation and hormonal therapy, the tumors will eventually return.” Cryotherapy, Brice said, could be a more effective way to treat cancer for patients who can’t have surgery.
“The fact that we only saw a 10 percent recurrence rate in our study is incredibly promising,” she said.

