Scientists: Don’t Leave Religious Communities Out in the Cold

A star of David reflects the perspective of a Rabbi/M.D. on an important question about the future of society.
[Editor's Note: This essay is in response to our current Big Question series: "How can the religious and scientific communities work together to foster a culture that is equipped to face humanity's biggest challenges?"]
I humbly submit that the question should be rephrased: How can the religious and scientific communities NOT work together to face humanity's biggest challenges? The stakes are higher than ever before, and we simply cannot afford to go it alone.
I believe in evolution -- the evolution of the relationship of science and religion.
The future of the world depends on our collaboration. I believe in evolution -- the evolution of the relationship of science and religion. Science and religion have lived in alternately varying relationships ranging from peaceful coexistence to outright warfare. Today we have evolved and have begun to embrace the biological relationship of mutualism. This is in part due to the advances in medicine and science.
Previous scientific discoveries and paradigm shifts precipitated varying theological responses. With Copernicus, we grappled with the relationship of the earth to the universe. With Darwin, we re-evaluated the relationship of man to the other creatures on earth. However, as theologically complex as these debates were, they had no practical relevance to the common man. Indeed, it was possible for people to live their entire lives happily without pondering these issues.
In the 21st century, the microscope is honing in further, with discoveries relating to the understanding of the very nature and composition of the human being, both body and mind/soul. Thus, as opposed to the past, the implications of the latest scientific advances directly affect the common man. The religious implications are not left to the ivory tower theologians. Regular people are now confronted with practical religious questions previously unimagined.
For example, in the field of infertility, if a married woman undergoes donor insemination, is she considered an adulteress? If a woman of one faith gestates the child of another faith, to whose faith does the child belong? If your heart is failing, can you avail yourself of stem cells derived from human embryos, or would you be considered an accomplice to murder? Would it be preferable to use artificially derived stem cells if they are available?
The implications of our current debates are profound, and profoundly personal. Science is the great equalizer. Every living being can potentially benefit from medical advances. We are all consumers of the scientific advances, irrespective of race or religion. As such, we all deserve a say in their development.
If the development of the science is collaborative, surely the contemplation of its ethical/religious applications should likewise be.
With gene editing, uterus transplants, head transplants, artificial reproductive seed, and animal-human genetic combinations as daily headlines, we have myriad ethical dilemmas to ponder. What limits should we set for the uses of different technologies? How should they be financed? We must even confront the very definition of what it means to be human. A human could receive multiple artificial transplants, 3D printed organs, genetic derivatives, or organs grown in animals. When does a person become another person or lose his identity? Will a being produced entirely from synthetic DNA be human?
In the Middle Ages, it was possible for one person to master all of the known science, and even sometimes religion as well, such as the great Maimonides. In the pre-modern era, discoveries were almost always attributed to one individual: Jenner, Lister, Koch, Pasteur, and so on. Today, it is impossible for any one human being to master medicine, let alone ethics, religion, etc. Advances are made not usually by one person but by collaboration, often involving hundreds, if not thousands of people across the globe. We cite journal articles, not individuals. Furthermore, the magnitude and speed of development is staggering. Add artificial intelligence and it will continue to expand exponentially.
If the development of the science is collaborative, surely the contemplation of its ethical/religious applications should likewise be. The issues are so profound that we need all genes on deck. The religious community should have a prominent seat at the table. There is great wisdom in the religious traditions that can inform contemporary discussions. In addition, the religious communities are significant consumers of, not to mention contributors to, the medical technology.
An ongoing dialogue between the scientific and religious communities should be an institutionalized endeavor, not a sporadic event, reactive to a particular discovery. The National Institutes of Health or other national organizations could provide an online newsletter designed for the clergy with a summary of the latest developments and their potential applications. An annual meeting of scientists and religious leaders could provide a forum for the scientists to appreciate the religious ramifications of their research (which may be none as well) and for the clergy to appreciate the rapidly developing fields of science and the implications for their congregants. Theological seminaries must include basic scientific literacy as part of their curricula.
We need the proper medium of mutual respect and admiration, despite healthy disagreement.
How do we create a "culture"? Microbiological cultures take time and require the proper medium for maximal growth. If one of the variables is altered, the culture can be affected. To foster a culture of continued successful collaboration between scientists and religious communities, we likewise need the proper medium of mutual respect and admiration, despite healthy disagreement.
The only way we can navigate these unchartered waters is through constant, deep and meaningful collaboration every single step of the way. By cultivating a mutualistic relationship we can inform, caution and safeguard each other to maximize the benefits of emerging technologies.
[Ed. Note: Don't miss the other perspectives in this Big Question series, from a science scholar and a Reverend/molecular geneticist.]
Scientists have known about and studied heart rate variability, or HRV, for a long time and, in recent years, monitors have come to market that can measure HRV accurately.
This episode is about a health metric you may not have heard of before: heart rate variability, or HRV. This refers to the small changes in the length of time between each of your heart beats.
Scientists have known about and studied HRV for a long time. In recent years, though, new monitors have come to market that can measure HRV accurately whenever you want.
Five months ago, I got interested in HRV as a more scientific approach to finding the lifestyle changes that work best for me as an individual. It's at the convergence of some important trends in health right now, such as health tech, precision health and the holistic approach in systems biology, which recognizes how interactions among different parts of the body are key to health.
But HRV is just one of many numbers worth paying attention to. For this episode of Making Sense of Science, I spoke with psychologist Dr. Leah Lagos; Dr. Jessilyn Dunn, assistant professor in biomedical engineering at Duke; and Jason Moore, the CEO of Spren and an app called Elite HRV. We talked about what HRV is, research on its benefits, how to measure it, whether it can be used to make improvements in health, and what researchers still need to learn about HRV.
*Talk to your doctor before trying anything discussed in this episode related to HRV and lifestyle changes to raise it.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Show notes
Spren - https://www.spren.com/
Elite HRV - https://elitehrv.com/
Jason Moore's Twitter - https://twitter.com/jasonmooreme?lang=en
Dr. Jessilyn Dunn's Twitter - https://twitter.com/drjessilyn?lang=en
Dr. Dunn's study on HRV, flu and common cold - https://jamanetwork.com/journals/jamanetworkopen/f...
Dr. Leah Lagos - https://drleahlagos.com/
Dr. Lagos on Star Talk - https://www.youtube.com/watch?v=jC2Q10SonV8
Research on HRV and intermittent fasting - https://pubmed.ncbi.nlm.nih.gov/33859841/
Research on HRV and Mediterranean diet - https://medicalxpress.com/news/2010-06-twin-medite...:~:text=Using%20data%20from%20the%20Emory,eating%20a%20Western%2Dtype%20diet
Devices for HRV biofeedback - https://elitehrv.com/heart-variability-monitors-an...
Benefits of HRV biofeedback - https://pubmed.ncbi.nlm.nih.gov/32385728/
HRV and cognitive performance - https://www.frontiersin.org/articles/10.3389/fnins...
HRV and emotional regulation - https://pubmed.ncbi.nlm.nih.gov/36030986/
Fortune article on HRV - https://fortune.com/well/2022/12/26/heart-rate-var...
Peanut allergies affect about a million children in the U.S., and most never outgrow them. Luckily, some promising remedies are in the works.
Ever since he was a baby, Sharon Wong’s son Brandon suffered from rashes, prolonged respiratory issues and vomiting. In 2006, as a young child, he was diagnosed with a severe peanut allergy.
"My son had a history of reacting to traces of peanuts in the air or in food,” says Wong, a food allergy advocate who runs a blog focusing on nut free recipes, cooking techniques and food allergy awareness. “Any participation in school activities, social events, or travel with his peanut allergy required a lot of preparation.”
Peanut allergies affect around a million children in the U.S. Most never outgrow the condition. The problem occurs when the immune system mistakenly views the proteins in peanuts as a threat and releases chemicals to counteract it. This can lead to digestive problems, hives and shortness of breath. For some, like Wong’s son, even exposure to trace amounts of peanuts could be life threatening. They go into anaphylactic shock and need to take a shot of adrenaline as soon as possible.
Typically, people with peanut allergies try to completely avoid them and carry an adrenaline autoinjector like an EpiPen in case of emergencies. This constant vigilance is very stressful, particularly for parents with young children.
“The search for a peanut allergy ‘cure’ has been a vigorous one,” says Claudia Gray, a pediatrician and allergist at Vincent Pallotti Hospital in Cape Town, South Africa. The closest thing to a solution so far, she says, is the process of desensitization, which exposes the patient to gradually increasing doses of peanut allergen to build up a tolerance. The most common type of desensitization is oral immunotherapy, where patients ingest small quantities of peanut powder. It has been effective but there is a risk of anaphylaxis since it involves swallowing the allergen.
"By the end of the trial, my son tolerated approximately 1.5 peanuts," Sharon Wong says.
DBV Technologies, a company based in Montrouge, France has created a skin patch to address this problem. The Viaskin Patch contains a much lower amount of peanut allergen than oral immunotherapy and delivers it through the skin to slowly increase tolerance. This decreases the risk of anaphylaxis.
Wong heard about the peanut patch and wanted her son to take part in an early phase 2 trial for 4-to-11-year-olds.
“We felt that participating in DBV’s peanut patch trial would give him the best chance at desensitization or at least increase his tolerance from a speck of peanut to a peanut,” Wong says. “The daily routine was quite simple, remove the old patch and then apply a new one. By the end of the trial, he tolerated approximately 1.5 peanuts.”
How it works
For DBV Technologies, it all began when pediatric gastroenterologist Pierre-Henri Benhamou teamed up with fellow professor of gastroenterology Christopher Dupont and his brother, engineer Bertrand Dupont. Together they created a more effective skin patch to detect when babies have allergies to cow's milk. Then they realized that the patch could actually be used to treat allergies by promoting tolerance. They decided to focus on peanut allergies first as the more dangerous.
The Viaskin patch utilizes the fact that the skin can promote tolerance to external stimuli. The skin is the body’s first defense. Controlling the extent of the immune response is crucial for the skin. So it has defense mechanisms against external stimuli and can promote tolerance.
The patch consists of an adhesive foam ring with a plastic film on top. A small amount of peanut protein is placed in the center. The adhesive ring is attached to the back of the patient's body. The peanut protein sits above the skin but does not directly touch it. As the patient sweats, water droplets on the inside of the film dissolve the peanut protein, which is then absorbed into the skin.
The peanut protein is then captured by skin cells called Langerhans cells. They play an important role in getting the immune system to tolerate certain external stimuli. Langerhans cells take the peanut protein to lymph nodes which activate T regulatory cells. T regulatory cells suppress the allergic response.
A different patch is applied to the skin every day to increase tolerance. It’s both easy to use and convenient.
“The DBV approach uses much smaller amounts than oral immunotherapy and works through the skin significantly reducing the risk of allergic reactions,” says Edwin H. Kim, the division chief of Pediatric Allergy and Immunology at the University of North Carolina, U.S., and one of the principal investigators of Viaskin’s clinical trials. “By not going through the mouth, the patch also avoids the taste and texture issues. Finally, the ability to apply a patch and immediately go about your day may be very attractive to very busy patients and families.”
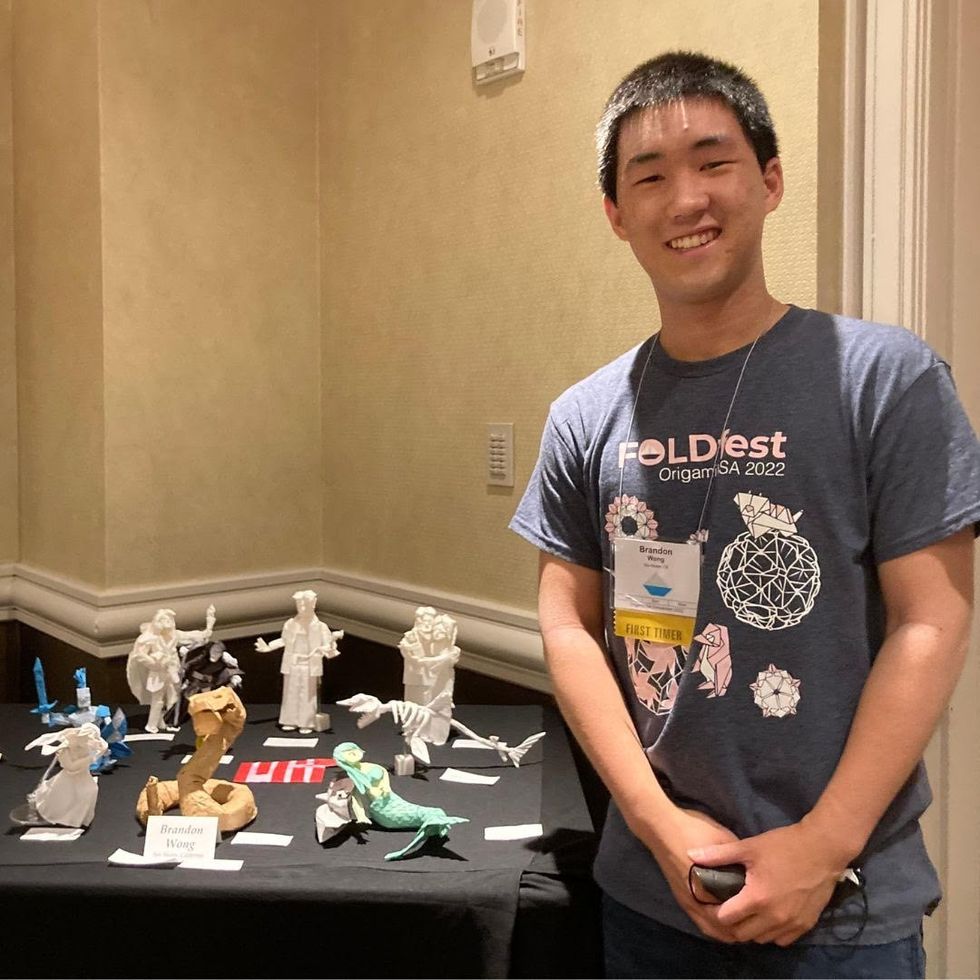
Brandon Wong displaying origami figures he folded at an Origami Convention in 2022
Sharon Wong
Clinical trials
Results from DBV's phase 3 trial in children ages 1 to 3 show its potential. For a positive result, patients who could not tolerate 10 milligrams or less of peanut protein had to be able to manage 300 mg or more after 12 months. Toddlers who could already tolerate more than 10 mg needed to be able to manage 1000 mg or more. In the end, 67 percent of subjects using the Viaskin patch met the target as compared to 33 percent of patients taking the placebo dose.
“The Viaskin peanut patch has been studied in several clinical trials to date with promising results,” says Suzanne M. Barshow, assistant professor of medicine in allergy and asthma research at Stanford University School of Medicine in the U.S. “The data shows that it is safe and well-tolerated. Compared to oral immunotherapy, treatment with the patch results in fewer side effects but appears to be less effective in achieving desensitization.”
The primary reason the patch is less potent is that oral immunotherapy uses a larger amount of the allergen. Additionally, absorption of the peanut protein into the skin could be erratic.
Gray also highlights that there is some tradeoff between risk and efficacy.
“The peanut patch is an exciting advance but not as effective as the oral route,” Gray says. “For those patients who are very sensitive to orally ingested peanut in oral immunotherapy or have an aversion to oral peanut, it has a use. So, essentially, the form of immunotherapy will have to be tailored to each patient.” Having different forms such as the Viaskin patch which is applied to the skin or pills that patients can swallow or dissolve under the tongue is helpful.
The hope is that the patch’s efficacy will increase over time. The team is currently running a follow-up trial, where the same patients continue using the patch.
“It is a very important study to show whether the benefit achieved after 12 months on the patch stays stable or hopefully continues to grow with longer duration,” says Kim, who is an investigator in this follow-up trial.
"My son now attends university in Massachusetts, lives on-campus, and eats dorm food. He has so much more freedom," Wong says.
The team is further ahead in the phase 3 follow-up trial for 4-to-11-year-olds. The initial phase 3 trial was not as successful as the trial for kids between one and three. The patch enabled patients to tolerate more peanuts but there was not a significant enough difference compared to the placebo group to be definitive. The follow-up trial showed greater potency. It suggests that the longer patients are on the patch, the stronger its effects.
They’re also testing if making the patch bigger, changing the shape and extending the minimum time it’s worn can improve its benefits in a trial for a new group of 4-to-11 year-olds.
The future
DBV Technologies is using the skin patch to treat cow’s milk allergies in children ages 1 to 17. They’re currently in phase 2 trials.
As for the peanut allergy trials in toddlers, the hope is to see more efficacy soon.
For Wong’s son who took part in the earlier phase 2 trial for 4-to-11-year-olds, the patch has transformed his life.
“My son continues to maintain his peanut tolerance and is not affected by peanut dust in the air or cross-contact,” Wong says. ”He attends university in Massachusetts, lives on-campus, and eats dorm food. He still carries an EpiPen but has so much more freedom than before his clinical trial. We will always be grateful.”

