Should Genetic Information About Mental Health Affect Civil Court Cases?

A rendering of DNA with a judge's gavel.
Imagine this scenario: A couple is involved in a heated custody dispute over their only child. As part of the effort to make the case of being a better guardian, one parent goes on a "genetic fishing expedition": this parent obtains a DNA sample from the other parent with the hope that such data will identify some genetic predisposition to a psychiatric condition (e.g., schizophrenia) and tilt the judge's custody decision in his or her favor.
As knowledge of psychiatric genetics is growing, it is likely to be introduced in civil cases, such as child custody disputes and education-related cases, raising a tangle of ethical and legal questions.
This is an example of how "behavioral genetic evidence" -- an umbrella term for information gathered from family history and genetic testing about pathological behaviors, including psychiatric conditions—may in the future be brought by litigants in court proceedings. Such evidence has been discussed primarily when criminal defendants sought to introduce it to make the claim that they are not responsible for their behavior or to justify their request for reduced sentencing and more lenient punishment.
However, civil cases are an emerging frontier for behavioral genetic evidence. It has already been introduced in tort litigation, such as personal injury claims, and as knowledge of psychiatric genetics is growing, it is further likely to be introduced in other civil cases, such as child custody disputes and education-related cases. But the introduction of such evidence raises a tangle of ethical and legal questions that civil courts will need to address. For example: how should such data be obtained? Who should get to present it and under what circumstances? And does the use of such evidence fit with the purposes of administering justice?
How Did We Get Here?
That behavioral genetic evidence is entering courts is unsurprising. Scientific evidence is a common feature of judicial proceedings, and genetic information may reveal relevant findings. For example, genetic evidence may elucidate whether a child's medical condition is due to genetic causes or medical malpractice, and it has been routinely used to identify alleged offenders or putative fathers. But behavioral genetic evidence is different from such other genetic data – it is shades of gray, instead of black and white.
Although efforts to understand the nature and origins of human behavior are ongoing, existing and likely future knowledge about behavioral genetics is limited. Behavioral disorders are highly complex and diverse. They commonly involve not one but multiple genes, each with a relatively small effect. They are impacted by many, yet unknown, interactions between genes, familial, and environmental factors such as poverty and childhood adversity.
And a specific gene variant may be associated with more than one behavioral disorder and be manifested with significantly different symptoms. Thus, biomarkers about "predispositions" for behavioral disorders cannot generally provide a diagnosis or an accurate estimate of whether, when, and at what severity a behavioral disorder will occur. And, unlike genetic testing that can confirm litigants' identity with 99.99% probability, behavioral genetic evidence is far more speculative.
Genetic theft raises questions about whose behavioral data are being obtained, by whom, and with what authority.
Whether judges, jurors, and other experts understand the nuances of behavioral genetics is unclear. Many people over-estimate the deterministic nature of genetics, and under-estimate the role of environments, especially with regards to mental health status. The U.S. individualistic culture of self-reliance and independence may further tilt the judicial scales because litigants in civil courts may be unjustly blamed for their "bad genes" while structural and societal determinants that lead to poor behavioral outcomes are ignored.
These concerns were recently captured in the Netflix series "13 Reasons Why," depicting a negligence lawsuit against a school brought by parents of a high-school student there (Hannah) who committed suicide. The legal tides shifted from the school's negligence in tolerating a culture of bullying to parental responsibility once cross-examination of Hannah's mother revealed a family history of anxiety, and the possibility that Hannah had a predisposition for mental illness, which (arguably) required therapy even in the absence of clear symptoms.
Where Is This Going?
The concerns are exacerbated given the ways in which behavioral genetic evidence may come to court in the future. One way is through "genetic theft," where genetic evidence is obtained from deserted property, such as soft-drink cans. This method is often used for identification purposes such as criminal and paternity proceedings, and it will likely expand to behavioral genetic data once available through "home kits" that are offered by direct-to-consumer companies.
Genetic theft raises questions about whose behavioral data are being obtained, by whom, and with what authority. In the scenario of child-custody dispute, for example, the sequencing of the other parent's DNA will necessarily intrude on the privacy of that parent, even as the scientific value of such information is limited. A parent on a "genetic fishing expedition" can also secretly sequence their child for psychiatric genetic predispositions, arguably, in order to take preventative measures to reduce the child's risk for developing a behavioral disorder. But should a parent be allowed to sequence the child without the other parent's consent, or regardless of whether the results will provide medical benefits to the child?
Similarly, although schools are required, and may be held accountable for failing to identify children with behavioral disabilities and to evaluate their educational needs, some parents may decline their child's evaluation by mental health professionals. Should schools secretly obtain a sample and sequence children for behavioral disorders, regardless of parental consent? My study of parents found that the overwhelming majority opposed imposed genetic testing by school authorities. But should parental preference or the child's best interests be the determinative factor? Alternatively, could schools use secretly obtained genetic data as a defense that they are fulfilling the child-find requirement under the law?
The stigma associated with behavioral disorders may intimidate some people enough that they back down from just claims.
In general, samples obtained through genetic theft may not meet the legal requirements for admissible evidence, and as these examples suggest, they also involve privacy infringement that may be unjustified in civil litigation. But their introduction in courts may influence judicial proceedings. It is hard to disregard such evidence even if decision-makers are told to ignore it.
The costs associated with genetic testing may further intensify power differences among litigants. Because not everyone can pay for DNA sequencing, there is a risk that those with more resources will be "better off" in court proceedings. Simultaneously, the stigma associated with behavioral disorders may intimidate some people enough that they back down from just claims. For example, a good parent may give up a custody claim to avoid disclosure of his or her genetic predispositions for psychiatric conditions. Regulating this area of law is necessary to prevent misuses of scientific technologies and to ensure that powerful actors do not have an unfair advantage over weaker litigants.
Behavioral genetic evidence may also enter the courts through subpoena of data obtained in clinical, research or other commercial genomic settings such as ancestry testing (similar to the genealogy database recently used to identify the Golden State Killer). Although court orders to testify or present evidence are common, their use for obtaining behavioral genetic evidence raises concerns.
One worry is that it may be over-intrusive. Because behavioral genetics are heritable, such data may reveal information not only about the individual litigant but also about other family members who may subsequently be stigmatized as well. And, even if we assume that many people may be willing for their data in genomic databases to be used to identify relatives who committed crimes (e.g., a rapist or a murderer), we can't assume the same for civil litigation, where the public interest in disclosure is far weaker.
Another worry is that it may deter people from participating in activities that society has an interest in advancing, including medical treatment involving genetic testing and genomic research. To address this concern, existing policy provides expanded privacy protections for NIH-funded genomic research by automatically issuing a Certificate of Confidentiality that prohibits disclosure of identifiable information in any Federal, State, or local civil, criminal, and other legal proceedings.
But this policy has limitations. It applies only to specific research settings and does not cover non-NIH funded research or clinical testing. The Certificate's protections can also be waived under certain circumstances. People who volunteer to participate in non-NIH-funded genomic research for the public good may thus find themselves worse-off if embroiled in legal proceedings.
Consider the following: if a parent in a child custody dispute had participated in a genetic study on schizophrenia years earlier, should the genetic results be subpoenaed by the court – and weaponized by the other parent? Public policy should aim to reduce the risks for such individuals. The end of obtaining behavioral genetic evidence cannot, and should not, always justify the means.
Scientists have known about and studied heart rate variability, or HRV, for a long time and, in recent years, monitors have come to market that can measure HRV accurately.
This episode is about a health metric you may not have heard of before: heart rate variability, or HRV. This refers to the small changes in the length of time between each of your heart beats.
Scientists have known about and studied HRV for a long time. In recent years, though, new monitors have come to market that can measure HRV accurately whenever you want.
Five months ago, I got interested in HRV as a more scientific approach to finding the lifestyle changes that work best for me as an individual. It's at the convergence of some important trends in health right now, such as health tech, precision health and the holistic approach in systems biology, which recognizes how interactions among different parts of the body are key to health.
But HRV is just one of many numbers worth paying attention to. For this episode of Making Sense of Science, I spoke with psychologist Dr. Leah Lagos; Dr. Jessilyn Dunn, assistant professor in biomedical engineering at Duke; and Jason Moore, the CEO of Spren and an app called Elite HRV. We talked about what HRV is, research on its benefits, how to measure it, whether it can be used to make improvements in health, and what researchers still need to learn about HRV.
*Talk to your doctor before trying anything discussed in this episode related to HRV and lifestyle changes to raise it.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Show notes
Spren - https://www.spren.com/
Elite HRV - https://elitehrv.com/
Jason Moore's Twitter - https://twitter.com/jasonmooreme?lang=en
Dr. Jessilyn Dunn's Twitter - https://twitter.com/drjessilyn?lang=en
Dr. Dunn's study on HRV, flu and common cold - https://jamanetwork.com/journals/jamanetworkopen/f...
Dr. Leah Lagos - https://drleahlagos.com/
Dr. Lagos on Star Talk - https://www.youtube.com/watch?v=jC2Q10SonV8
Research on HRV and intermittent fasting - https://pubmed.ncbi.nlm.nih.gov/33859841/
Research on HRV and Mediterranean diet - https://medicalxpress.com/news/2010-06-twin-medite...:~:text=Using%20data%20from%20the%20Emory,eating%20a%20Western%2Dtype%20diet
Devices for HRV biofeedback - https://elitehrv.com/heart-variability-monitors-an...
Benefits of HRV biofeedback - https://pubmed.ncbi.nlm.nih.gov/32385728/
HRV and cognitive performance - https://www.frontiersin.org/articles/10.3389/fnins...
HRV and emotional regulation - https://pubmed.ncbi.nlm.nih.gov/36030986/
Fortune article on HRV - https://fortune.com/well/2022/12/26/heart-rate-var...
Peanut allergies affect about a million children in the U.S., and most never outgrow them. Luckily, some promising remedies are in the works.
Ever since he was a baby, Sharon Wong’s son Brandon suffered from rashes, prolonged respiratory issues and vomiting. In 2006, as a young child, he was diagnosed with a severe peanut allergy.
"My son had a history of reacting to traces of peanuts in the air or in food,” says Wong, a food allergy advocate who runs a blog focusing on nut free recipes, cooking techniques and food allergy awareness. “Any participation in school activities, social events, or travel with his peanut allergy required a lot of preparation.”
Peanut allergies affect around a million children in the U.S. Most never outgrow the condition. The problem occurs when the immune system mistakenly views the proteins in peanuts as a threat and releases chemicals to counteract it. This can lead to digestive problems, hives and shortness of breath. For some, like Wong’s son, even exposure to trace amounts of peanuts could be life threatening. They go into anaphylactic shock and need to take a shot of adrenaline as soon as possible.
Typically, people with peanut allergies try to completely avoid them and carry an adrenaline autoinjector like an EpiPen in case of emergencies. This constant vigilance is very stressful, particularly for parents with young children.
“The search for a peanut allergy ‘cure’ has been a vigorous one,” says Claudia Gray, a pediatrician and allergist at Vincent Pallotti Hospital in Cape Town, South Africa. The closest thing to a solution so far, she says, is the process of desensitization, which exposes the patient to gradually increasing doses of peanut allergen to build up a tolerance. The most common type of desensitization is oral immunotherapy, where patients ingest small quantities of peanut powder. It has been effective but there is a risk of anaphylaxis since it involves swallowing the allergen.
"By the end of the trial, my son tolerated approximately 1.5 peanuts," Sharon Wong says.
DBV Technologies, a company based in Montrouge, France has created a skin patch to address this problem. The Viaskin Patch contains a much lower amount of peanut allergen than oral immunotherapy and delivers it through the skin to slowly increase tolerance. This decreases the risk of anaphylaxis.
Wong heard about the peanut patch and wanted her son to take part in an early phase 2 trial for 4-to-11-year-olds.
“We felt that participating in DBV’s peanut patch trial would give him the best chance at desensitization or at least increase his tolerance from a speck of peanut to a peanut,” Wong says. “The daily routine was quite simple, remove the old patch and then apply a new one. By the end of the trial, he tolerated approximately 1.5 peanuts.”
How it works
For DBV Technologies, it all began when pediatric gastroenterologist Pierre-Henri Benhamou teamed up with fellow professor of gastroenterology Christopher Dupont and his brother, engineer Bertrand Dupont. Together they created a more effective skin patch to detect when babies have allergies to cow's milk. Then they realized that the patch could actually be used to treat allergies by promoting tolerance. They decided to focus on peanut allergies first as the more dangerous.
The Viaskin patch utilizes the fact that the skin can promote tolerance to external stimuli. The skin is the body’s first defense. Controlling the extent of the immune response is crucial for the skin. So it has defense mechanisms against external stimuli and can promote tolerance.
The patch consists of an adhesive foam ring with a plastic film on top. A small amount of peanut protein is placed in the center. The adhesive ring is attached to the back of the patient's body. The peanut protein sits above the skin but does not directly touch it. As the patient sweats, water droplets on the inside of the film dissolve the peanut protein, which is then absorbed into the skin.
The peanut protein is then captured by skin cells called Langerhans cells. They play an important role in getting the immune system to tolerate certain external stimuli. Langerhans cells take the peanut protein to lymph nodes which activate T regulatory cells. T regulatory cells suppress the allergic response.
A different patch is applied to the skin every day to increase tolerance. It’s both easy to use and convenient.
“The DBV approach uses much smaller amounts than oral immunotherapy and works through the skin significantly reducing the risk of allergic reactions,” says Edwin H. Kim, the division chief of Pediatric Allergy and Immunology at the University of North Carolina, U.S., and one of the principal investigators of Viaskin’s clinical trials. “By not going through the mouth, the patch also avoids the taste and texture issues. Finally, the ability to apply a patch and immediately go about your day may be very attractive to very busy patients and families.”
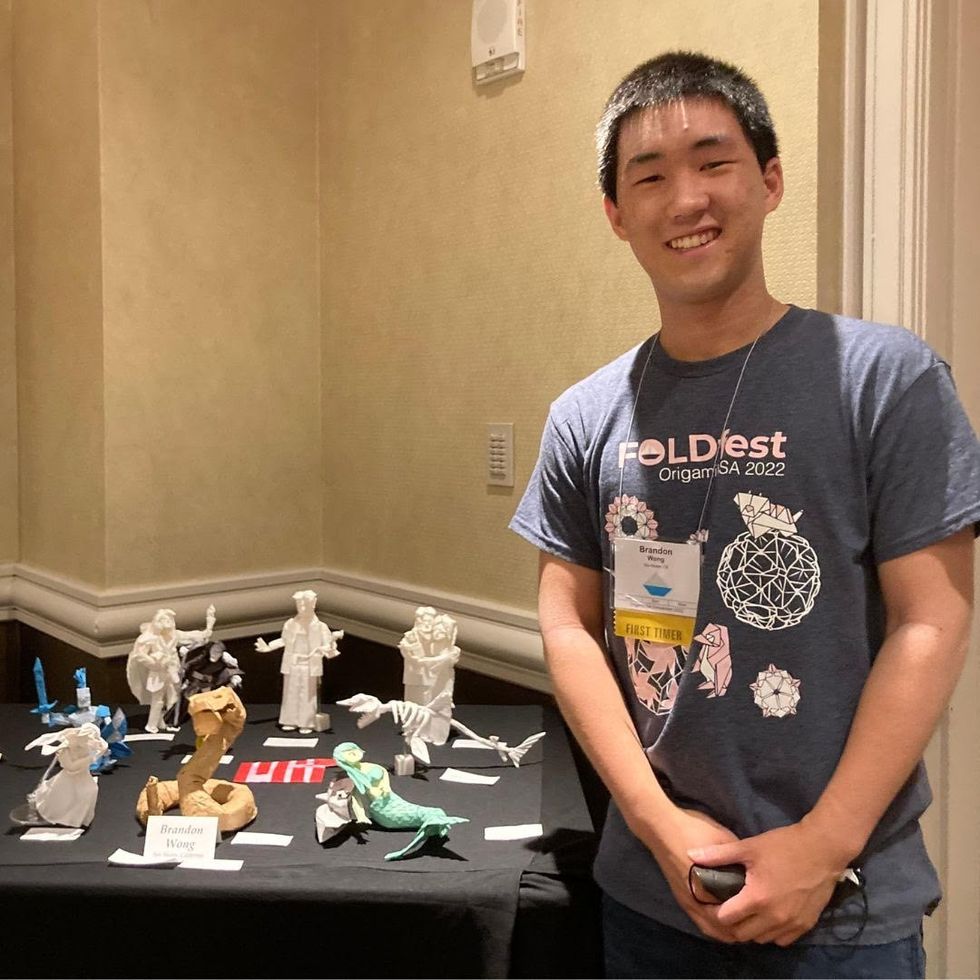
Brandon Wong displaying origami figures he folded at an Origami Convention in 2022
Sharon Wong
Clinical trials
Results from DBV's phase 3 trial in children ages 1 to 3 show its potential. For a positive result, patients who could not tolerate 10 milligrams or less of peanut protein had to be able to manage 300 mg or more after 12 months. Toddlers who could already tolerate more than 10 mg needed to be able to manage 1000 mg or more. In the end, 67 percent of subjects using the Viaskin patch met the target as compared to 33 percent of patients taking the placebo dose.
“The Viaskin peanut patch has been studied in several clinical trials to date with promising results,” says Suzanne M. Barshow, assistant professor of medicine in allergy and asthma research at Stanford University School of Medicine in the U.S. “The data shows that it is safe and well-tolerated. Compared to oral immunotherapy, treatment with the patch results in fewer side effects but appears to be less effective in achieving desensitization.”
The primary reason the patch is less potent is that oral immunotherapy uses a larger amount of the allergen. Additionally, absorption of the peanut protein into the skin could be erratic.
Gray also highlights that there is some tradeoff between risk and efficacy.
“The peanut patch is an exciting advance but not as effective as the oral route,” Gray says. “For those patients who are very sensitive to orally ingested peanut in oral immunotherapy or have an aversion to oral peanut, it has a use. So, essentially, the form of immunotherapy will have to be tailored to each patient.” Having different forms such as the Viaskin patch which is applied to the skin or pills that patients can swallow or dissolve under the tongue is helpful.
The hope is that the patch’s efficacy will increase over time. The team is currently running a follow-up trial, where the same patients continue using the patch.
“It is a very important study to show whether the benefit achieved after 12 months on the patch stays stable or hopefully continues to grow with longer duration,” says Kim, who is an investigator in this follow-up trial.
"My son now attends university in Massachusetts, lives on-campus, and eats dorm food. He has so much more freedom," Wong says.
The team is further ahead in the phase 3 follow-up trial for 4-to-11-year-olds. The initial phase 3 trial was not as successful as the trial for kids between one and three. The patch enabled patients to tolerate more peanuts but there was not a significant enough difference compared to the placebo group to be definitive. The follow-up trial showed greater potency. It suggests that the longer patients are on the patch, the stronger its effects.
They’re also testing if making the patch bigger, changing the shape and extending the minimum time it’s worn can improve its benefits in a trial for a new group of 4-to-11 year-olds.
The future
DBV Technologies is using the skin patch to treat cow’s milk allergies in children ages 1 to 17. They’re currently in phase 2 trials.
As for the peanut allergy trials in toddlers, the hope is to see more efficacy soon.
For Wong’s son who took part in the earlier phase 2 trial for 4-to-11-year-olds, the patch has transformed his life.
“My son continues to maintain his peanut tolerance and is not affected by peanut dust in the air or cross-contact,” Wong says. ”He attends university in Massachusetts, lives on-campus, and eats dorm food. He still carries an EpiPen but has so much more freedom than before his clinical trial. We will always be grateful.”

