The Stunning Comeback of a Top Transplant Surgeon Who Got a New Heart at His Own Hospital

Dr. Robert Montgomery, almost one year post-transplant, at a vineyard in Casablanca, Chile, August 2019.
Having spent my working life as a transplant surgeon, it is the ultimate irony that I have now become a heart transplant patient. I knew this was a possibility since 1987, when I was 27 years old and I received a phone call from my sister-in-law telling me that my 35-year-old brother, Rich, had just died suddenly while water skiing.
Living from one heartbeat to the next I knew I had to get it right and nail my life—and in that regard my disease was a blessing.
After his autopsy, dots were connected and it was clear that the mysterious heart disease my father had died from when I was 15 years old was genetic. I was evaluated and it was clear that I too had inherited cardiomyopathy, a progressive weakening condition of the heart muscle that often leads to dangerous rhythm disturbances and sudden death. My doctors urged me to have a newly developed device called an implantable cardioverter-defibrillator (ICD) surgically placed in my abdomen and chest to monitor and shock my heart back into normal rhythm should I have a sudden cardiac arrest.
They also told me I was the first surgeon in the world to undergo an ICD implant and that having one of these devices would not be compatible with the life of a surgeon and I should change careers to something less rigorous. With the support of a mentor and armed with what the British refer to as my "bloody-mindedness," I refused to give up this dream of becoming a transplant surgeon. I completed my surgical training and embarked on my career.
What followed were periods of stability punctuated by near-death experiences. I had a family, was productive in my work, and got on with life, knowing that this was a fragile situation that could turn on its head in a moment. In a way, it made my decisions about how to spend my time and focus my efforts more deliberate and purposeful. Living from one heartbeat to the next I knew I had to get it right and nail my life—and in that regard my disease was a blessing.
In 2017 while pursuing my passion for the outdoors in a remote part of Patagonia, I collapsed from bacterial pneumonia and sepsis. Unknowingly, I had brought in my lungs one of those super-bugs that you read about from the hospital where I worked. Several days into the trip, the bacteria entered my blood stream and brought me as close to death as a human can get.
I lay for nearly 3 weeks in a coma on a stretcher in a tiny hospital in Argentina, septic and in cardiogenic shock before stabilizing enough to be evaced to NYU Langone Hospital, where I was on staff. I awoke helpless, unable to walk, talk, or swallow food or drink. It was a long shot but I managed to recover completely from this episode; after 3 months, I returned to work and the operating room. My heart rebounded, but never back to where it had been.
Then, on the eve of my mother's funeral, I arrested while watching a Broadway show, and this time my ICD failed to revive me. There was prolonged CPR that broke my ribs and spine and a final shock that recaptured my heart. It was literally a show stopper and I awoke to a standing ovation from the New York theatre audience who were stunned by my modern recreation of the biblical story of Lazarus, or for the more hip among them, my real-life rendition of the resurrection of Jon Snow at the end of season 5 of Game of Thrones.
Against the advice of my doctors, I attended my mom's funeral and again tried to regain some sense of normalcy. We discussed a transplant at this point but, believe it or not, there is such a scarcity of organs I was not yet "sick enough" to get enough priority to receive a heart. I had more surgery to supercharge my ICD so it would be more likely to save my life the next time -- and there would be a next time, I knew.
As a transplant surgeon, I have been involved in some important innovations to expand the number of organs available for transplantation.
Months later in Matera, Italy, where I was attending a medical meeting, I developed what is referred to as ventricular tachycardia storm. I had 4 cardiac arrests over a 3-hour period. With the first one, I fell on to a stone floor and split my forehead open. When I arrived at the small hospital it seemed like Patagonia all over again. One of the first people I met was a Catholic priest who gave me the Last Rights.
I knew now was the moment and so with the help of one of my colleagues who was at the meeting with me and the compassion of the Italian doctors who supplied my friend with resuscitation medications and left my IV in place, I signed out of the hospital against medical advice and boarded a commercial flight back to New York. I was admitted to the NYU intensive care unit and received a heart transplant 3 weeks later.
Now, what I haven't said is that as a transplant surgeon, I have been involved in some important innovations to expand the number of organs available for transplantation. I came to NYU in 2016 to start a new Transplant Institute which included inaugurating a heart transplant program. We hired heart transplant surgeons, cardiologists, and put together a team that unbeknownst to me at the time, would save my life a year later.
It gets even more interesting. One of the innovations that I had been involved in from its inception in the 1990s was using organs from donors at risk for transmitting viruses like HIV and Hepatitis C (Hep C). We popularized new ways to detect these viruses in donors and ensure that the risk was minimized as much as possible so patients in need of a life-saving transplant could utilize these organs.
When the opioid crisis hit hard about four years ago, there were suddenly a lot of potential donors who were IV drug users and 25 percent of them were known to be infected with Hep C (which is spread by needles). In 2018, 49,000 people died in the U.S. from drug overdoses. There were many more donors with Hep C than potential recipients who had previously been exposed to Hep C, and so more than half of these otherwise perfectly good organs were being discarded. At the same time, a new class of drugs was being tested that could cure Hep C.
I was at Johns Hopkins at the time and our team developed a protocol for using these Hep C positive organs for Hep C negative recipients who were willing to take them, even knowing that they were likely to become infected with the virus. We would then treat them after the transplant with this new class of drugs and in all likelihood, cure them. I brought this protocol with me to NYU.
When my own time came, I accepted a Hep C heart from a donor who overdosed on heroin. I became infected with Hep C and it was then eliminated from my body with 2 months of anti-viral therapy. All along this unlikely journey, I was seemingly making decisions that would converge upon that moment in time when I would arise to catch the heart that was meant for me.

Dr. Montgomery with his wife Denyce Graves, September 2019.
(Courtesy Montgomery)
Today, I am almost exactly one year post-transplant, back to work, operating, traveling, enjoying the outdoors, and giving lectures. My heart disease is gone; gone when my heart was removed. Gone also is my ICD. I am no longer at risk for a sudden cardiac death. I traded all that for the life of a transplant patient, which has its own set of challenges, but I clearly traded up. It is cliché, I know, but I enjoy every moment of every day. It is a miracle I am still here.
Thanks to safety cautions from the COVID-19 pandemic, a strain of influenza has been completely eliminated.
If you were one of the millions who masked up, washed your hands thoroughly and socially distanced, pat yourself on the back—you may have helped change the course of human history.
Scientists say that thanks to these safety precautions, which were introduced in early 2020 as a way to stop transmission of the novel COVID-19 virus, a strain of influenza has been completely eliminated. This marks the first time in human history that a virus has been wiped out through non-pharmaceutical interventions, such as vaccines.
The flu shot, explained
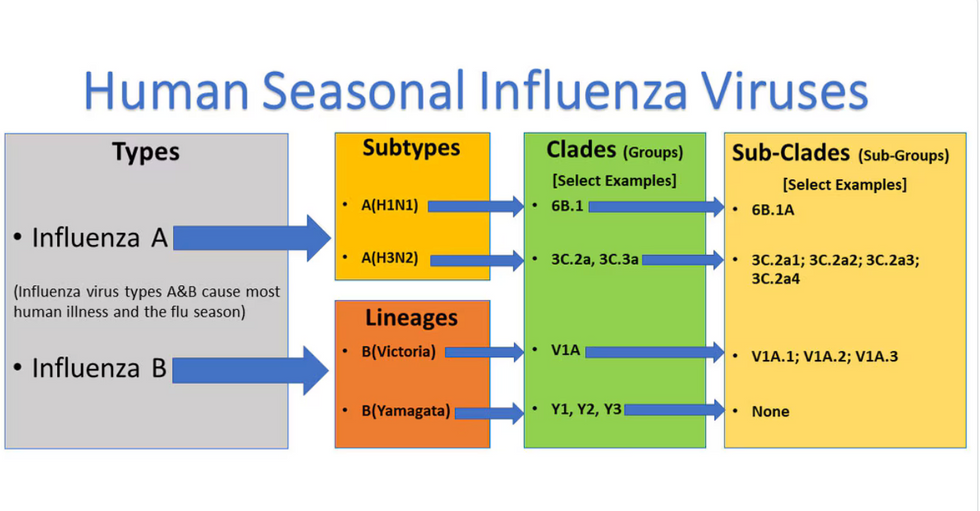
Influenza viruses type A and B are responsible for the majority of human illnesses and the flu season.
Centers for Disease Control
For more than a decade, flu shots have protected against two types of the influenza virus–type A and type B. While there are four different strains of influenza in existence (A, B, C, and D), only strains A, B, and C are capable of infecting humans, and only A and B cause pandemics. In other words, if you catch the flu during flu season, you’re most likely sick with flu type A or B.
Flu vaccines contain inactivated—or dead—influenza virus. These inactivated viruses can’t cause sickness in humans, but when administered as part of a vaccine, they teach a person’s immune system to recognize and kill those viruses when they’re encountered in the wild.
Each spring, a panel of experts gives a recommendation to the US Food and Drug Administration on which strains of each flu type to include in that year’s flu vaccine, depending on what surveillance data says is circulating and what they believe is likely to cause the most illness during the upcoming flu season. For the past decade, Americans have had access to vaccines that provide protection against two strains of influenza A and two lineages of influenza B, known as the Victoria lineage and the Yamagata lineage. But this year, the seasonal flu shot won’t include the Yamagata strain, because the Yamagata strain is no longer circulating among humans.
How Yamagata Disappeared

Flu surveillance data from the Global Initiative on Sharing All Influenza Data (GISAID) shows that the Yamagata lineage of flu type B has not been sequenced since April 2020.
Nature
Experts believe that the Yamagata lineage had already been in decline before the pandemic hit, likely because the strain was naturally less capable of infecting large numbers of people compared to the other strains. When the COVID-19 pandemic hit, the resulting safety precautions such as social distancing, isolating, hand-washing, and masking were enough to drive the virus into extinction completely.
Because the strain hasn’t been circulating since 2020, the FDA elected to remove the Yamagata strain from the seasonal flu vaccine. This will mark the first time since 2012 that the annual flu shot will be trivalent (three-component) rather than quadrivalent (four-component).
Should I still get the flu shot?
The flu shot will protect against fewer strains this year—but that doesn’t mean we should skip it. Influenza places a substantial health burden on the United States every year, responsible for hundreds of thousands of hospitalizations and tens of thousands of deaths. The flu shot has been shown to prevent millions of illnesses each year (more than six million during the 2022-2023 season). And while it’s still possible to catch the flu after getting the flu shot, studies show that people are far less likely to be hospitalized or die when they’re vaccinated.
Another unexpected benefit of dropping the Yamagata strain from the seasonal vaccine? This will possibly make production of the flu vaccine faster, and enable manufacturers to make more vaccines, helping countries who have a flu vaccine shortage and potentially saving millions more lives.
After his grandmother’s dementia diagnosis, one man invented a snack to keep her healthy and hydrated.
Founder Lewis Hornby and his grandmother Pat, sampling Jelly Drops—an edible gummy containing water and life-saving electrolytes.
On a visit to his grandmother’s nursing home in 2016, college student Lewis Hornby made a shocking discovery: Dehydration is a common (and dangerous) problem among seniors—especially those that are diagnosed with dementia.
Hornby’s grandmother, Pat, had always had difficulty keeping up her water intake as she got older, a common issue with seniors. As we age, our body composition changes, and we naturally hold less water than younger adults or children, so it’s easier to become dehydrated quickly if those fluids aren’t replenished. What’s more, our thirst signals diminish naturally as we age as well—meaning our body is not as good as it once was in letting us know that we need to rehydrate. This often creates a perfect storm that commonly leads to dehydration. In Pat’s case, her dehydration was so severe she nearly died.
When Lewis Hornby visited his grandmother at her nursing home afterward, he learned that dehydration especially affects people with dementia, as they often don’t feel thirst cues at all, or may not recognize how to use cups correctly. But while dementia patients often don’t remember to drink water, it seemed to Hornby that they had less problem remembering to eat, particularly candy.

Hornby wanted to create a solution for elderly people who struggled keeping their fluid intake up. He spent the next eighteen months researching and designing a solution and securing funding for his project. In 2019, Hornby won a sizable grant from the Alzheimer’s Society, a UK-based care and research charity for people with dementia and their caregivers. Together, through the charity’s Accelerator Program, they created a bite-sized, sugar-free, edible jelly drop that looked and tasted like candy. The candy, called Jelly Drops, contained 95% water and electrolytes—important minerals that are often lost during dehydration. The final product launched in 2020—and was an immediate success. The drops were able to provide extra hydration to the elderly, as well as help keep dementia patients safe, since dehydration commonly leads to confusion, hospitalization, and sometimes even death.
Not only did Jelly Drops quickly become a favorite snack among dementia patients in the UK, but they were able to provide an additional boost of hydration to hospital workers during the pandemic. In NHS coronavirus hospital wards, patients infected with the virus were regularly given Jelly Drops to keep their fluid levels normal—and staff members snacked on them as well, since long shifts and personal protective equipment (PPE) they were required to wear often left them feeling parched.
In April 2022, Jelly Drops launched in the United States. The company continues to donate 1% of its profits to help fund Alzheimer’s research.

