The Top 8 Things to Know About Anti-Aging Research Right Now
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

A birthday celebration in the future for someone reaching 150 years old.
Dr. Michael West has a storied legacy in the world of aging research. Twenty years ago, the company he started, Geron, hit upon a major breakthrough when his scientists isolated the active component for the gene that confers immortality to cells, called telomerase.
In the twenty years since, a new field has emerged: the science of extending the human "healthspan."
He was in the lab when scientists for the first time artificially turned on the gene in some skin cells donated by Dr. Leonard Hayflick, the man who had discovered back in 1965 that human cells age over time. Sure enough, with Geron's intervention, Hayflick's skin cells became immortal in the dish, and the landmark paper was published in Science in 1998.
In the twenty years since, a new field has emerged: the science of extending the human "healthspan" – the length of time people can live free of diseases related to aging. A substantial amount of preclinical and some clinical research is now underway, backed by heavy investments from some of the world's largest companies.
Today, Dr. West is the CEO of AgeX Therapeutics, a biotech company that is developing novel therapeutics to target human aging and age-related degenerative diseases using pluripotent stem cells. Dr. West recently shared some key insights with Editor-in-Chief Kira Peikoff about what's happening in this exciting space.
1) Pluripotent stem cells have opened the door for the first time in human history to manufacturing young cells and young tissue of any kind.
These are the body's master cells: They are self-replicating, and they can potentially give rise to any cell or tissue the body needs to repair itself. This year marks the 20th anniversary since their isolation for the first time in a lab.
"People in biotech say that the time from lab to discovery in products is about 20 years," West says. "But the good news is we're at that 20-year mark now, so you're seeing an explosive growth of applications. We can now make all cell types of the human body in a scalable manner."
2) Early human development could hold the key to unlocking the mystery of aging.
West believes that two things occur when the body forms in utero: telomerase, the immortalizing gene, gets turned off very early in development in the body cells like skin, liver, and nerves. Additionally, he thinks that a second genetic switch gets turned off that holds the potential for regeneration after injury.
"These insights open the door to intervention by the transfer of telomerase into the cells of the body."
"Very early when the body is first forming, if you cut the skin, it will not respond by scarring, but will regenerate scarlessly," he says. "But that potential gets turned off once the body is formed, about 8 weeks after fertilization. Then, you accumulate damage over a lifetime. Not only do cells have a finite capacity to replicate, but you have tissue damage."
However, there are animals in nature whose telomerase is never turned off, or whose regenerative ability is never turned off. The flatworm, for example, can regenerate its own head if it gets cut off, and it also shows no detectable aging. Lobsters are believed to be similar. (That's not to say it can't get caught and eaten for dinner.)
"These insights open the door to intervention by the transfer of telomerase into the cells of the body, or understanding how regeneration gets turned off, and then turning it back on," West says. "That's well within the power of modern medical research to understand."
3) Companies are investing tremendous resources into the anti-aging gold rush.
Devising interventions is the mission of AgeX, a subsidiary of BioTime, as well as a number of other companies.
"We're seeing a mad rush," West says. There's Google's Calico, which recently announced, with AbbVie Inc., another $1 billion into research for age-related diseases, on top of the previous $1.5 billion investment.
Other notable players include Unity Biotechnology, Samumed, Human Longevity Inc., RestorBio, Rejuvenate Bio,and Juvenescence (which is also an investor in AgeX).
"These are products in development by our company and others that the baby boomers can reasonably anticipate being available within their lifetimes."
4) The majority of clinical applications are still years away.
"What we've learned about turning back on this regenerative state, called induced tissue regeneration, is that the majority of the clinical implications are years away and will require years of clinical trials before potential FDA approval and marketing to the public," West says. "But we have found some potential near-term applications that we think may have a much faster track to commercialization. As you can imagine, we are all over those."
BioTime, Inc., AgeX's parent, has a regenerative medicine product in clinical trials for age-related macular degeneration, the leading cause of blindness in an aging population. While not yet approved by the FDA, BioTime has reported continued progress in the clinical development of the product now in Phase II trials.
Citi recently issued a major report, Disruptive Innovations VI, that included "Anti-Aging Medicines" as the number two innovation for investors to keep an eye on, and predicted that the first anti-aging therapies could receive regulatory approval by 2023.
5) Few, if any, medical interventions are available today that are proven to markedly slow aging - yet. But the Baby Boomers are not necessarily out of luck.
Buyer beware of any claims in the marketplace that a given skin cream or stem cell product will extend your life. More than likely, they won't.
"There are a lot of people trying to cash in on the aging baby boom population," West warns.
"When you hear claims of stem cell products that you can get now, it's important to understand that they are likely not based on pluripotent stem cell technology. Also, they are usually not products approved by the FDA, having gone through clinical trials to demonstrate safety and efficacy."
However, an array of young pluripotent stem cell-derived therapies are on a development track for future approvals.
One example is another program at AgeX: the manufacture of brown fat cells; these cells burn calories rather than store them. They burn circulating fat like triglycerides and sugar in the blood and generate heat.
"You lose brown fat in aging, and animal models suggest that if you restore that tissue, you can restore a metabolic balance to be more like what you had when you were young," says West. "When I was 18, I could drink milkshakes all day long and not gain an ounce. But at 50 or 60, most of us would rapidly put on weight. Why? We believe that one important factor is that with age, you lose this brown fat tissue. The loss throws your metabolism off balance. So the solution is conceptually simple, we plan to make young brown fat cells for transplantation to reset the balance, potentially to treat Type II diabetes or even obesity.
"These are products in development by our company and others that the baby boomers can reasonably anticipate being available within their lifetimes."
6) There is an ethical debate about how far to apply this new science.
Some people are speculating about whether genetic engineering might one day be used to program longer lifespans into humans at the earliest stages of development. (Note: it is against the law across the Western world to edit human embryos intended for reproduction, although just last week, Chinese scientists used CRISPR to repair a disease-causing mutation in viable human embryos.)
West sounds a cautionary note about such interventions meant to lengthen life. "For people who think not just about the science, but the ethics, safety is a major concern. It's entirely possible to genetically engineer babies, but when you make such modifications, it's an experiment, not just in human cells in a dish, but in a human being. I have a great reticence to put any human at risk unless it's a case where the person is suffering with a life-threatening disease, and the potential therapy is their last best hope."
"I have no doubt, zero doubt, that in the foreseeable future, we'll hear of a person who has lived to about 150."
7) The biggest challenge of intervening in human aging is cultural denial.
"The prospect of intervening in a profound way in human aging is still not seen as credible by the vast majority of thoughtful people around the world," West laments.
"Aging is a universal phenomenon, it's mankind's greatest enemy, but as a species we've adapted to the realities of finite lifespans and death. We have a whole infrastructure of belief systems around this, and many people see it as inevitable."
8) The lifespan for healthy children born today could surpass anything humanity has ever seen.
"It is at least 150 years of age," West predicts. "I have no doubt, zero doubt, that in the foreseeable future, we'll hear of a person who has lived to about 150. We know now it's possible. I've never said that publicly before, but I am comfortable now with the prediction. And, of course, if some people now living could live to 150 years of age, we have the prospect of them living to see even more powerful therapies. So, the question now is, what kind of a world are we going to make for future generations?"
[Editor's Note: Check out our latest video, which was inspired by Dr. West's exclusive prediction to leapsmag.]
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Researchers claimed they built a breakthrough superconductor. Social media shot it down almost instantly.
In July, South Korean scientists posted a paper finding they had achieved superconductivity - a claim that was debunked within days.
Harsh Mathur was a graduate physics student at Yale University in late 1989 when faculty announced they had failed to replicate claims made by scientists at the University of Utah and the University of Wolverhampton in England.
Such work is routine. Replicating or attempting to replicate the contraptions, calculations and conclusions crafted by colleagues is foundational to the scientific method. But in this instance, Yale’s findings were reported globally.
“I had a ringside view, and it was crazy,” recalls Mathur, now a professor of physics at Case Western Reserve University in Ohio.
Yale’s findings drew so much attention because initial experiments by Stanley Pons of Utah and Martin Fleischmann of Wolverhampton led to a startling claim: They were able to fuse atoms at room temperature – a scientific El Dorado known as “cold fusion.”
Nuclear fusion powers the stars in the universe. However, star cores must be at least 23.4 million degrees Fahrenheit and under extraordinary pressure to achieve fusion. Pons and Fleischmann claimed they had created an almost limitless source of power achievable at any temperature.
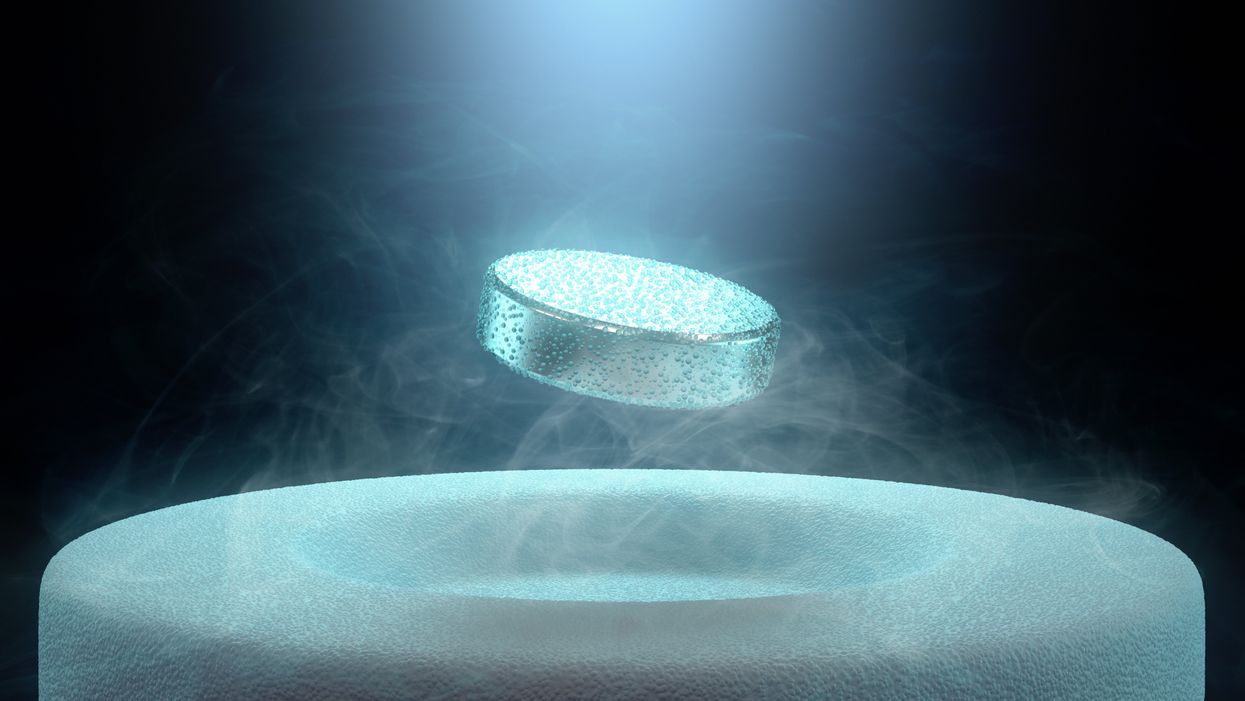
Like fusion, superconductivity can only be achieved in mostly impractical circumstances.
But about six months after they made their startling announcement, the pair’s findings were discredited by researchers at Yale and the California Institute of Technology. It was one of the first instances of a major scientific debunking covered by mass media.
Some scholars say the media attention for cold fusion stemmed partly from a dazzling announcement made three years prior in 1986: Scientists had created the first “superconductor” – material that could transmit electrical current with little or no resistance. It drew global headlines – and whetted the public’s appetite for announcements of scientific breakthroughs that could cause economic transformations.
But like fusion, superconductivity can only be achieved in mostly impractical circumstances: It must operate either at temperatures of at least negative 100 degrees Fahrenheit, or under pressures of around 150,000 pounds per square inch. Superconductivity that functions in closer to a normal environment would cut energy costs dramatically while also opening infinite possibilities for computing, space travel and other applications.
In July, a group of South Korean scientists posted material claiming they had created an iron crystalline substance called LK-99 that could achieve superconductivity at slightly above room temperature and at ambient pressure. The group partners with the Quantum Energy Research Centre, a privately-held enterprise in Seoul, and their claims drew global headlines.
Their work was also debunked. But in the age of internet and social media, the process was compressed from half-a-year into days. And it did not require researchers at world-class universities.
One of the most compelling critiques came from Derrick VanGennep. Although he works in finance, he holds a Ph.D. in physics and held a postdoctoral position at Harvard. The South Korean researchers had posted a video of a nugget of LK-99 in what they claimed was the throes of the Meissner effect – an expulsion of the substance’s magnetic field that would cause it to levitate above a magnet. Unless Hollywood magic is involved, only superconducting material can hover in this manner.
That claim made VanGennep skeptical, particularly since LK-99’s levitation appeared unenthusiastic at best. In fact, a corner of the material still adhered to the magnet near its center. He thought the video demonstrated ferromagnetism – two magnets repulsing one another. He mixed powdered graphite with super glue, stuck iron filings to its surface and mimicked the behavior of LK-99 in his own video, which was posted alongside the researchers’ video.
VanGennep believes the boldness of the South Korean claim was what led to him and others in the scientific community questioning it so quickly.
“The swift replication attempts stemmed from the combination of the extreme claim, the fact that the synthesis for this material is very straightforward and fast, and the amount of attention that this story was getting on social media,” he says.
But practicing scientists were suspicious of the data as well. Michael Norman, director of the Argonne Quantum Institute at the Argonne National Laboratory just outside of Chicago, had doubts immediately.
Will this saga hurt or even affect the careers of the South Korean researchers? Possibly not, if the previous fusion example is any indication.
“It wasn’t a very polished paper,” Norman says of the Korean scientists’ work. That opinion was reinforced, he adds, when it turned out the paper had been posted online by one of the researchers prior to seeking publication in a peer-reviewed journal. Although Norman and Mathur say that is routine with scientific research these days, Norman notes it was posted by one of the junior researchers over the doubts of two more senior scientists on the project.
Norman also raises doubts about the data reported. Among other issues, he observes that the samples created by the South Korean researchers contained traces of copper sulfide that could inadvertently amplify findings of conductivity.
The lack of the Meissner effect also caught Mathur’s attention. “Ferromagnets tend to be unstable when they levitate,” he says, adding that the video “just made me feel unconvinced. And it made me feel like they hadn't made a very good case for themselves.”
Will this saga hurt or even affect the careers of the South Korean researchers? Possibly not, if the previous fusion example is any indication. Despite being debunked, cold fusion claimants Pons and Fleischmann didn’t disappear. They moved their research to automaker Toyota’s IMRA laboratory in France, which along with the Japanese government spent tens of millions of dollars on their work before finally pulling the plug in 1998.
Fusion has since been created in laboratories, but being unable to reproduce the density of a star’s core would require excruciatingly high temperatures to achieve – about 160 million degrees Fahrenheit. A recently released Government Accountability Office report concludes practical fusion likely remains at least decades away.
However, like Pons and Fleischman, the South Korean researchers are not going anywhere. They claim that LK-99’s Meissner effect is being obscured by the fact the substance is both ferromagnetic and diamagnetic. They have filed for a patent in their country. But for now, those claims remain chimerical.
In the meantime, the consensus as to when a room temperature superconductor will be achieved is mixed. VenGennep – who studied the issue during his graduate and postgraduate work – puts the chance of creating such a superconductor by 2050 at perhaps 50-50. Mathur believes it could happen sooner, but adds that research on the topic has been going on for nearly a century, and that it has seen many plateaus.
“There's always this possibility that there's going to be something out there that we're going to discover unexpectedly,” Norman notes. The only certainty in this age of social media is that it will be put through the rigors of replication instantly.
Scientists implant brain cells to counter Parkinson's disease
In a recent research trial, patients with Parkinson's disease reported that their symptoms had improved after stem cells were implanted into their brains. Martin Taylor, far right, was diagnosed at age 32.
Martin Taylor was only 32 when he was diagnosed with Parkinson's, a disease that causes tremors, stiff muscles and slow physical movement - symptoms that steadily get worse as time goes on.
“It's horrible having Parkinson's,” says Taylor, a data analyst, now 41. “It limits my ability to be the dad and husband that I want to be in many cruel and debilitating ways.”
Today, more than 10 million people worldwide live with Parkinson's. Most are diagnosed when they're considerably older than Taylor, after age 60. Although recent research has called into question certain aspects of the disease’s origins, Parkinson’s eventually kills the nerve cells in the brain that produce dopamine, a signaling chemical that carries messages around the body to control movement. Many patients have lost 60 to 80 percent of these cells by the time they are diagnosed.
For years, there's been little improvement in the standard treatment. Patients are typically given the drug levodopa, a chemical that's absorbed by the brain’s nerve cells, or neurons, and converted into dopamine. This drug addresses the symptoms but has no impact on the course of the disease as patients continue to lose dopamine producing neurons. Eventually, the treatment stops working effectively.
BlueRock Therapeutics, a cell therapy company based in Massachusetts, is taking a different approach by focusing on the use of stem cells, which can divide into and generate new specialized cells. The company makes the dopamine-producing cells that patients have lost and inserts these cells into patients' brains. “We have a disease with a high unmet need,” says Ahmed Enayetallah, the senior vice president and head of development at BlueRock. “We know [which] cells…are lost to the disease, and we can make them. So it really came together to use stem cells in Parkinson's.”
In a phase 1 research trial announced late last month, patients reported that their symptoms had improved after a year of treatment. Brain scans also showed an increased number of neurons generating dopamine in patients’ brains.
Increases in dopamine signals
The recent phase 1 trial focused on deploying BlueRock’s cell therapy, called bemdaneprocel, to treat 12 patients suffering from Parkinson’s. The team developed the new nerve cells and implanted them into specific locations on each side of the patient's brain through two small holes in the skull made by a neurosurgeon. “We implant cells into the places in the brain where we think they have the potential to reform the neural networks that are lost to Parkinson's disease,” Enayetallah says. The goal is to restore motor function to patients over the long-term.
Five patients were given a relatively low dose of cells while seven got higher doses. Specialized brain scans showed evidence that the transplanted cells had survived, increasing the overall number of dopamine producing cells. The team compared the baseline number of these cells before surgery to the levels one year later. “The scans tell us there is evidence of increased dopamine signals in the part of the brain affected by Parkinson's,” Enayetallah says. “Normally you’d expect the signal to go down in untreated Parkinson’s patients.”
"I think it has a real chance to reverse motor symptoms, essentially replacing a missing part," says Tilo Kunath, a professor of regenerative neurobiology at the University of Edinburgh.
The team also asked patients to use a specific type of home diary to log the times when symptoms were well controlled and when they prevented normal activity. After a year of treatment, patients taking the higher dose reported symptoms were under control for an average of 2.16 hours per day above their baselines. At the smaller dose, these improvements were significantly lower, 0.72 hours per day. The higher-dose patients reported a corresponding decrease in the amount of time when symptoms were uncontrolled, by an average of 1.91 hours, compared to 0.75 hours for the lower dose. The trial was safe, and patients tolerated the year of immunosuppression needed to make sure their bodies could handle the foreign cells.
Claire Bale, the associate director of research at Parkinson's U.K., sees the promise of BlueRock's approach, while noting the need for more research on a possible placebo effect. The trial participants knew they were getting the active treatment, and placebo effects are known to be a potential factor in Parkinson’s research. Even so, “The results indicate that this therapy produces improvements in symptoms for Parkinson's, which is very encouraging,” Bale says.
Tilo Kunath, a professor of regenerative neurobiology at the University of Edinburgh, also finds the results intriguing. “I think it's excellent,” he says. “I think it has a real chance to reverse motor symptoms, essentially replacing a missing part.” However, it could take time for this therapy to become widely available, Kunath says, and patients in the late stages of the disease may not benefit as much. “Data from cell transplantation with fetal tissue in the 1980s and 90s show that cells did not survive well and release dopamine in these [late-stage] patients.”
Searching for the right approach
There's a long history of using cell therapy as a treatment for Parkinson's. About four decades ago, scientists at the University of Lund in Sweden developed a method in which they transferred parts of fetal brain tissue to patients with Parkinson's so that their nerve cells would produce dopamine. Many benefited, and some were able to stop their medication. However, the use of fetal tissue was highly controversial at that time, and the tissues were difficult to obtain. Later trials in the U.S. showed that people benefited only if a significant amount of the tissue was used, and several patients experienced side effects. Eventually, the work lost momentum.
“Like many in the community, I'm aware of the long history of cell therapy,” says Taylor, the patient living with Parkinson's. “They've long had that cure over the horizon.”
In 2000, Lorenz Studer led a team at the Memorial Sloan Kettering Centre, in New York, to find the chemical signals needed to get stem cells to differentiate into cells that release dopamine. Back then, the team managed to make cells that produced some dopamine, but they led to only limited improvements in animals. About a decade later, in 2011, Studer and his team found the specific signals needed to guide embryonic cells to become the right kind of dopamine producing cells. Their experiments in mice, rats and monkeys showed that their implanted cells had a significant impact, restoring lost movement.
Studer then co-founded BlueRock Therapeutics in 2016. Forming the most effective stem cells has been one of the biggest challenges, says Enayetallah, the BlueRock VP. “It's taken a lot of effort and investment to manufacture and make the cells at the right scale under the right conditions.” The team is now using cells that were first isolated in 1998 at the University of Wisconsin, a major advantage because they’re available in a virtually unlimited supply.
Other efforts underway
In the past several years, University of Lund researchers have begun to collaborate with the University of Cambridge on a project to use embryonic stem cells, similar to BlueRock’s approach. They began clinical trials this year.
A company in Japan called Sumitomo is using a different strategy; instead of stem cells from embryos, they’re reprogramming adults' blood or skin cells into induced pluripotent stem cells - meaning they can turn into any cell type - and then directing them into dopamine producing neurons. Although Sumitomo started clinical trials earlier than BlueRock, they haven’t yet revealed any results.
“It's a rapidly evolving field,” says Emma Lane, a pharmacologist at the University of Cardiff who researches clinical interventions for Parkinson’s. “But BlueRock’s trial is the first full phase 1 trial to report such positive findings with stem cell based therapies.” The company’s upcoming phase 2 research will be critical to show how effectively the therapy can improve disease symptoms, she added.
The cure over the horizon
BlueRock will continue to look at data from patients in the phase 1 trial to monitor the treatment’s effects over a two-year period. Meanwhile, the team is planning the phase 2 trial with more participants, including a placebo group.
For patients with Parkinson’s like Martin Taylor, the therapy offers some hope, though Taylor recognizes that more research is needed.

BlueRock Therapeutics
“Like many in the community, I'm aware of the long history of cell therapy,” he says. “They've long had that cure over the horizon.” His expectations are somewhat guarded, he says, but, “it's certainly positive to see…movement in the field again.”
"If we can demonstrate what we’re seeing today in a more robust study, that would be great,” Enayetallah says. “At the end of the day, we want to address that unmet need in a field that's been waiting for a long time.”
Editor's note: The company featured in this piece, BlueRock Therapeutics, is a portfolio company of Leaps by Bayer, which is a sponsor of Leaps.org. BlueRock was acquired by Bayer Pharmaceuticals in 2019. Leaps by Bayer and other sponsors have never exerted influence over Leaps.org content or contributors.