The Troubling Reason I Obsessively Researched My Pregnancy

A pregnant woman in her third trimester.
At the end of my second trimester of pregnancy, I answered a call from an unknown number.
To be pregnant is to exist on a never-ending receiving line of advice, whether we want it or not.
"I know your due date is approaching," said a stranger at the other end of the line, completely freaking me out. She identified herself as being from Natera, a company that my doctor had used for genetic testing I had consented to months ago.
"Excuse me?" I said.
"Have you considered cord-blood banking?" she said.
"No, I'm not doing that," I said. I had read enough about cord-blood banking, the process of saving stem cell-containing blood from your baby's umbilical cord, to understand that my family was in the vast majority of those that would with extremely high likelihood derive no medical benefit from it. Of course, in the societally sanctioned spending spree that accompanies new parenthood, plenty of companies are happy to charge anyone hundreds if not thousands of dollars plus annual storage fees to collect and manage your cord blood.
"Why not? Have you considered all the bene—"
"I'm not doing it and I don't want to explain my decision," I said before hanging up. I would later learn I neglected to check a miniscule box on my testing consent forms at the doctor to opt out of solicitations. Still, I was angry that I was being telemarketed unnecessary and costly medical services by someone who had been trained to immediately call my judgment into question. I was annoyed that my doctor's office would allow such intrusions at all. When I asked my OB about it at my next visit, she told me there's no way Natera would have gotten my information from them. Apparently even she didn't realize what was on those forms.
The incident with Natera did nothing to heighten my trust of the medical establishment during my pregnancy. I was hardly alone. Almost every mom I knew had expressed a similar sentiment.
"I don't trust doctors," read the text of a loved one when I told her I would probably get an epidural after my doctor recommended getting one because, she said, it can help relax the pelvic muscles during labor. But this friend, a highly educated woman who had had done her research and had two unmedicated births, believed firmly otherwise. "Look it up," she said. Thus commenced more of the furious Googling I found myself doing multiple times a day since deciding I wanted to become pregnant.
To be pregnant is to exist on a never-ending receiving line of advice, whether we want it or not. Information presents to us from Google's never-out-of-reach search bar, friends and family eager to use our pregnancies as an excuse to recall their own, and the doctor's office, where the wisdom of medical professionals neatly comingles with brochures and free samples from myriad companies that would really, really like our business as new moms. Separating the "good" advice from the rest is a Herculean task that many pregnant women manage only with vigorous fact-finding missions of their own.
The medical community in America is poorly equipped to help women navigate the enormous pressures that come with birth and transitioning to motherhood.
Doing my research during pregnancy felt like a defense against the scary unknowns, overabundance of opinions, and disturbing marketing schemes that come with entering parenthood. The medical community in America is poorly equipped to help women navigate the enormous emotional and societal pressures that come with birth and transitioning to motherhood. Too much of what pregnant women experience at the doctor has to do with dated ideas about our care, mandated by tradition or a fear of being sued rather than medical necessity. These practices, like weigh-ins at every appointment or medically unnecessary C-sections (which are estimated to account, horrifically, for almost 50 percent of all C-sections performed in the U.S.), only heighten anxiety.
Meanwhile, things that might alleviate stress – like having thorough discussions about the kinds of interventions we might be asked to accept at the hospital during labor and delivery – are left to outside educators and doulas that insurance plans typically don't cover. The net effect isn't better health outcomes for mom and baby, but rather a normalized sense of distrust many American women feel toward their OBGYNs, and the burden of going to every appointment and the delivery room on the defensive. Instead of being wed to dated medical practices and tangled in America's new motherhood industrial complex, shouldn't our doctors, of all people, be our biggest advocates?
As soon as I found out I was pregnant, I devoured Expecting Better, by Emily Oster, an economist who embarked on her own fact-finding mission during her first pregnancy, predicated on the belief that the advice OBGYNs have been giving pregnant women for decades is out of date and unnecessarily restrictive. The book includes controversial stances, like that having small amounts of alcohol while pregnant is OK. (More recent research has called this view into question.) Oster writes that for the vast majority of pregnant women, it's perfectly fine to lie on your back, do sit-ups, and eat Brie — all things I was relieved to learn I wouldn't have to give up for nine months, despite the traditional advice, which my doctor also gave to me.
Oster recommends hiring a doula, based both on research and personal experience. It's a worthwhile investment for those who can afford it: according to one study, 20.4 percent of laboring women with doulas had C-sections compared with 34.2 percent of women without them. A doula can do many things for a pregnant client, including helping her write a birth plan, massaging her back in labor, and cheering her on, which is especially useful for women who plan to labor without pain medication. Use of doulas is on the rise; according to DONA International, the world's largest and oldest doula association, the number of doulas who have been certified to date is over 12,000, up from 2,000 in 2002.
But the most significant role a doula plays is that of patient advocate in the hospital. This is a profound commentary on the way the medical establishment handles childbirth, a medical event that 86 percent of women aged 40 to 44 had gone through as of 2016. Recognizing the maternal mortality crisis in the U.S., where women are far more likely to die as a result of childbirth than anywhere else in the developed world and black women are three times more likely to die in childbirth than white women, a few states now allow Medicaid to cover doulas. Can you imagine feeling the need to hire an independent non-medical care provider to help you run interference with your doctors and nurses for something like an appendectomy?
I wouldn't have been aware of all the imminent interventions during my labor if my doula hadn't told me about them. Things happen fast in the hospital and doctors and nurses may rush patients to consent before proceeding with things like breaking their water or hooking them up to an IV of Pitocin. Only because my husband and I had spent six hours in birth class — a suggestion by my doula — did I realize that I was empowered to say "no" to such procedures.
Expecting more trustworthy advice to come from my doctor than books or Google or even a doula hardly seems unreasonable.
Of course, we all feel immense pressure to become good parents, and questioning conventional medical wisdom is a natural response to that pressure. "Looking around at the world and saying, who am I as a parent? What is important to me? Who are the wise people? What do I think wisdom is? What is a good decision? If you're a certain type of introspective person, if you're really asking those questions, that's going to include like taking a second look at things that doctors, for example, say," says Koyuki Smith, a doula and birth educator.
Expecting more trustworthy advice to come from my doctor than books or Google or even a doula hardly seems unreasonable. Yet my doctor's office seemed more concerned with checking off a list of boxes rather than providing me with personalized care that might have relieved my understandable anxiety about my first birth. When I still hadn't gone into labor around the time of my due date, my doctor encouraged me to be induced because my baby appeared to be large. I declined but scheduled an induction to "hold my spot" around the 42-week mark.
When I asked what medication would be used for an induction if I had one and she said Cytotec, I told her I had read that drug could cause serious complications, but she dismissed my concerns after I told her they stemmed from a book I read on natural childbirth. The FDA's page on Cytotec isn't exactly reassuring.
The nurse who took me in triage after I went into labor a week past my due date practically scolded me for waiting to go into labor naturally instead of opting for induction sooner. My doula told her while I was struggling to speak through labor pains to get off my case about it. I hadn't even become a mom and I was already doing so many things "wrong." Because I had done my own reading, I felt confident that my choices weren't harming my baby or me.
Becoming a mom would be less daunting if the medical community found a way to help women navigate the pressures of motherhood instead of adding to them. "Our culture at large doesn't support women enough in the complicated emotions that are a part of this process," said Alexandra Saks, a reproductive psychologist and author of What No One Tells You: A Guide to Your Emotions From Pregnancy to Motherhood. "I hope that every practitioner that works with women around reproductive health prioritizes her emotions around her experience."
For many of us, that will mean doctors who help us understand the pros and cons of conventional advice, don't use their offices as marketing channels, and don't pressure women into medically unnecessary inductions. Moms should also receive more attention after delivery both in the hospital and after they get home; a single, quick postpartum visit at six weeks is not an adequate way to care for women recovering from the trauma of childbirth, nor is it an adequate way to ensure women are emotionally supported during the transition. While several people interrogated me about my mental health at the hospital and my doctor's office just before and after birth, if I had been concerned about postpartum depression, I can't imagine feeling comfortable enough in those moments to tell strangers filling out obligatory worksheets.
It also means figuring out how to talk to patients who are prone to Googling their pregnancies with gusto every single day. It would be impossible for many women to shun independent research during pregnancy altogether. But it would also be nice if our doctors didn't add to our impulse to do it.
Scientists Are Working to Decipher the Puzzle of ‘Broken Heart Syndrome’
Elaine Kamil had just returned home after a few days of business meetings in 2013 when she started having chest pains. At first Kamil, then 66, wasn't worried—she had had some chest pain before and recently went to a cardiologist to do a stress test, which was normal.
"I can't be having a heart attack because I just got checked," she thought, attributing the discomfort to stress and high demands of her job. A pediatric nephrologist at Cedars-Sinai Hospital in Los Angeles, she takes care of critically ill children who are on dialysis or are kidney transplant patients. Supporting families through difficult times and answering calls at odd hours is part of her daily routine, and often leaves her exhausted.
She figured the pain would go away. But instead, it intensified that night. Kamil's husband drove her to the Cedars-Sinai hospital, where she was admitted to the coronary care unit. It turned out she wasn't having a heart attack after all. Instead, she was diagnosed with a much less common but nonetheless dangerous heart condition called takotsubo syndrome, or broken heart syndrome.
A heart attack happens when blood flow to the heart is obstructed—such as when an artery is blocked—causing heart muscle tissue to die. In takotsubo syndrome, the blood flow isn't blocked, but the heart doesn't pump it properly. The heart changes its shape and starts to resemble a Japanese fishing device called tako-tsubo, a clay pot with a wider body and narrower mouth, used to catch octopus.
"The heart muscle is stunned and doesn't function properly anywhere from three days to three weeks," explains Noel Bairey Merz, the cardiologist at Cedar Sinai who Kamil went to see after she was discharged.
"The heart muscle is stunned and doesn't function properly anywhere from three days to three weeks."
But even though the heart isn't permanently damaged, mortality rates due to takotsubo syndrome are comparable to those of a heart attack, Merz notes—about 4-5 percent of patients die from the attack, and 20 percent within the next five years. "It's as bad as a heart attack," Merz says—only it's much less known, even to doctors. The condition affects only about 1 percent of people, and there are around 15,000 new cases annually. It's diagnosed using a cardiac ventriculogram, an imaging test that allows doctors to see how the heart pumps blood.
Scientists don't fully understand what causes Takotsubo syndrome, but it usually occurs after extreme emotional or physical stress. Doctors think it's triggered by a so-called catecholamine storm, a phenomenon in which the body releases too much catecholamines—hormones involved in the fight-or-flight response. Evolutionarily, when early humans lived in savannas or forests and had to either fight off predators or flee from them, these hormones gave our ancestors the needed strength and stamina to take either action. Released by nerve endings and by the adrenal glands that sit on top of the kidneys, these hormones still flood our bodies in moments of stress, but an overabundance of them could sometimes be damaging.

Elaine Kamil
A study by scientists at Harvard Medical School linked increased risk of takotsubo to higher activity in the amygdala, a brain region responsible for emotions that's involved in responses to stress. The scientists believe that chronic stress makes people more susceptible to the syndrome. Notably, one small study suggested that the number of Takotsubo cases increased during the COVID-19 pandemic.
There are no specific drugs to treat takotsubo, so doctors rely on supportive therapies, which include medications typically used for high blood pressure and heart failure. In most cases, the heart returns to its normal shape within a few weeks. "It's a spontaneous recovery—the catecholamine storm is resolved, the injury trigger is removed and the heart heals itself because our bodies have an amazing healing capacity," Merz says. It also helps that tissues remain intact. 'The heart cells don't die, they just aren't functioning properly for some time."
That's the good news. The bad news is that takotsubo is likely to strike again—in 5-20 percent of patients the condition comes back, sometimes more severe than before.
That's exactly what happened to Kamil. After getting her diagnosis in 2013, she realized that she actually had a previous takotsubo episode. In 2010, she experienced similar symptoms after her son died. "The night after he died, I was having severe chest pain at night, but I was too overwhelmed with grief to do anything about it," she recalls. After a while, the pain subsided and didn't return until three years later.
For weeks after her second attack, she felt exhausted, listless and anxious. "You lose confidence in your body," she says. "You have these little twinges on your chest, or if you start having arrhythmia, and you wonder if this is another episode coming up. It's really unnerving because you don't know how to read these cues." And that's very typical, Merz says. Even when the heart muscle appears to recover, patients don't return to normal right away. They have shortens of breath, they can't exercise, and they stay anxious and worried for a while.
Women over the age of 50 are diagnosed with takotsubo more often than other demographics. However, it happens in men too, although it typically strikes after physical stress, such as a triathlon or an exhausting day of cycling. Young people can also get takotsubo. Older patients are hospitalized more often, but younger people tend to have more severe complications. It could be because an older person may go for a jog while younger one may run a marathon, which would take a stronger toll on the body of a person who's predisposed to the condition.
Notably, the emotional stressors don't always have to be negative—the heart muscle can get out of shape from good emotions, too. "There have been case reports of takotsubo at weddings," Merz says. Moreover, one out of three or four takotsubo patients experience no apparent stress, she adds. "So it could be that it's not so much the catecholamine storm itself, but the body's reaction to it—the physiological reaction deeply embedded into out physiology," she explains.
Merz and her team are working to understand what makes people predisposed to takotsubo. They think a person's genetics play a role, but they haven't yet pinpointed genes that seem to be responsible. Genes code for proteins, which affect how the body metabolizes various compounds, which, in turn, affect the body's response to stress. Pinning down the protein involved in takotsubo susceptibility would allow doctors to develop screening tests and identify those prone to severe repeating attacks. It will also help develop medications that can either prevent it or treat it better than just waiting for the body to heal itself.
Researchers at the Imperial College London found that elevated levels of certain types of microRNAs—molecules involved in protein production—increase the chances of developing takotsubo.
In one study, researchers tried treating takotsubo in mice with a drug called suberanilohydroxamic acid, or SAHA, typically used for cancer treatment. The drug improved cardiac health and reversed the broken heart in rodents. It remains to be seen if the drug would have a similar effect on humans. But identifying a drug that shows promise is progress, Merz says. "I'm glad that there's research in this area."
This article was originally published by Leaps.org on July 28, 2021.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.
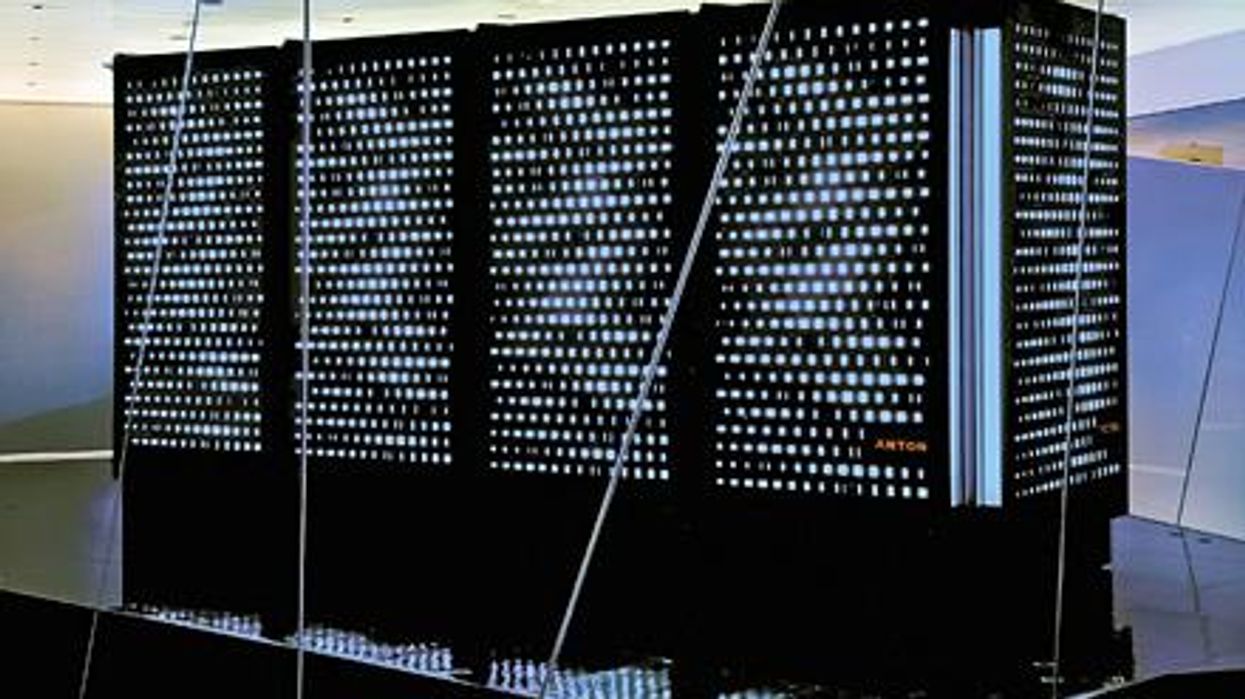
Did Anton the AI find a new treatment for a deadly cancer?
Researchers used a supercomputer to learn about the subtle movement of a cancer-causing molecule, and then they found the precise drug that can recognize that motion.
Bile duct cancer is a rare and aggressive form of cancer that is often difficult to diagnose. Patients with advanced forms of the disease have an average life expectancy of less than two years.
Many patients who get cancer in their bile ducts – the tubes that carry digestive fluid from the liver to the small intestine – have mutations in the protein FGFR2, which leads cells to grow uncontrollably. One treatment option is chemotherapy, but it’s toxic to both cancer cells and healthy cells, failing to distinguish between the two. Increasingly, cancer researchers are focusing on biomarker directed therapy, or making drugs that target a particular molecule that causes the disease – FGFR2, in the case of bile duct cancer.
A problem is that in targeting FGFR2, these drugs inadvertently inhibit the FGFR1 protein, which looks almost identical. This causes elevated phosphate levels, which is a sign of kidney damage, so doses are often limited to prevent complications.
In recent years, though, a company called Relay has taken a unique approach to picking out FGFR2, using a powerful supercomputer to simulate how proteins move and change shape. The team, leveraging this AI capability, discovered that FGFR2 and FGFR1 move differently, which enabled them to create a more precise drug.
Preliminary studies have shown robust activity of this drug, called RLY-4008, in FGFR2 altered tumors, especially in bile duct cancer. The drug did not inhibit FGFR1 or cause significant side effects. “RLY-4008 is a prime example of a precision oncology therapeutic with its highly selective and potent targeting of FGFR2 genetic alterations and resistance mutations,” says Lipika Goyal, assistant professor of medicine at Harvard Medical School. She is a principal investigator of Relay’s phase 1-2 clinical trial.
Boosts from AI and a billionaire
Traditional drug design has been very much a case of trial and error, as scientists investigate many molecules to see which ones bind to the intended target and bind less to other targets.
“It’s being done almost blindly, without really being guided by structure, so it fails very often,” says Olivier Elemento, associate director of the Institute for Computational Biomedicine at Cornell. “The issue is that they are not sampling enough molecules to cover some of the chemical space that would be specific to the target of interest and not specific to others.”
Relay’s unique hardware and software allow simulations that could never be achieved through traditional experiments, Elemento says.
Some scientists have tried to use X-rays of crystallized proteins to look at the structure of proteins and design better drugs. But they have failed to account for an important factor: proteins are moving and constantly folding into different shapes.
David Shaw, a hedge fund billionaire, wanted to help improve drug discovery and understood that a key obstacle was that computer models of molecular dynamics were limited; they simulated motion for less than 10 millionths of a second.
In 2001, Shaw set up his own research facility, D.E. Shaw Research, to create a supercomputer that would be specifically designed to simulate protein motion. Seven years later, he succeeded in firing up a supercomputer that can now conduct high speed simulations roughly 100 times faster than others. Called Anton, it has special computer chips to enable this speed, and its software is powered by AI to conduct many simulations.
After creating the supercomputer, Shaw teamed up with leading scientists who were interested in molecular motion, and they founded Relay Therapeutics.
Elemento believes that Relay’s approach is highly beneficial in designing a better drug for bile duct cancer. “Relay Therapeutics has a cutting-edge approach for molecular dynamics that I don’t believe any other companies have, at least not as advanced.” Relay’s unique hardware and software allow simulations that could never be achieved through traditional experiments, Elemento says.
How it works
Relay used both experimental and computational approaches to design RLY-4008. The team started out by taking X-rays of crystallized versions of both their intended target, FGFR2, and the almost identical FGFR1. This enabled them to get a 3D snapshot of each of their structures. They then fed the X-rays into the Anton supercomputer to simulate how the proteins were likely to move.
Anton’s simulations showed that the FGFR1 protein had a flap that moved more frequently than FGFR2. Based on this distinct motion, the team tried to design a compound that would recognize this flap shifting around and bind to FGFR2 while steering away from its more active lookalike.
For that, they went back Anton, using the supercomputer to simulate the behavior of thousands of potential molecules for over a year, looking at what made a particular molecule selective to the target versus another molecule that wasn’t. These insights led them to determine the best compounds to make and test in the lab and, ultimately, they found that RLY-4008 was the most effective.
Promising results so far
Relay began phase 1-2 trials in 2020 and will continue until 2024. Preliminary results showed that, in the 17 patients taking a 70 mg dose of RLY-4008, the drug worked to shrink tumors in 88 percent of patients. This was a significant increase compared to other FGFR inhibitors. For instance, Futibatinib, which recently got FDA approval, had a response rate of only 42 percent.
Across all dose levels, RLY-4008 shrank tumors by 63 percent in 38 patients. In more good news, the drug didn’t elevate their phosphate levels, which suggests that it could be taken without increasing patients’ risk for kidney disease.
“Objectively, this is pretty remarkable,” says Elemento. “In a small patient study, you have a molecule that is able to shrink tumors in such a high fraction of patients. It is unusual to see such good results in a phase 1-2 trial.”
A simulated future
The research team is continuing to use molecular dynamic simulations to develop other new drug, such as one that is being studied in patients with solid tumors and breast cancer.
As for their bile duct cancer drug, RLY-4008, Relay plans by 2024 to have tested it in around 440 patients. “The mature results of the phase 1-2 trial are highly anticipated,” says Goyal, the principal investigator of the trial.
Sameek Roychowdhury, an oncologist and associate professor of internal medicine at Ohio State University, highlights the need for caution. “This has early signs of benefit, but we will look forward to seeing longer term results for benefit and side effect profiles. We need to think a few more steps ahead - these treatments are like the ’Whack-a-Mole game’ where cancer finds a way to become resistant to each subsequent drug.”
“I think the issue is going to be how durable are the responses to the drug and what are the mechanisms of resistance,” says Raymond Wadlow, an oncologist at the Inova Medical Group who specializes in gastrointestinal and haematological cancer. “But the results look promising. It is a much more selective inhibitor of the FGFR protein and less toxic. It’s been an exciting development.”