This Mom Donated Her Lost Baby’s Tissue to Research
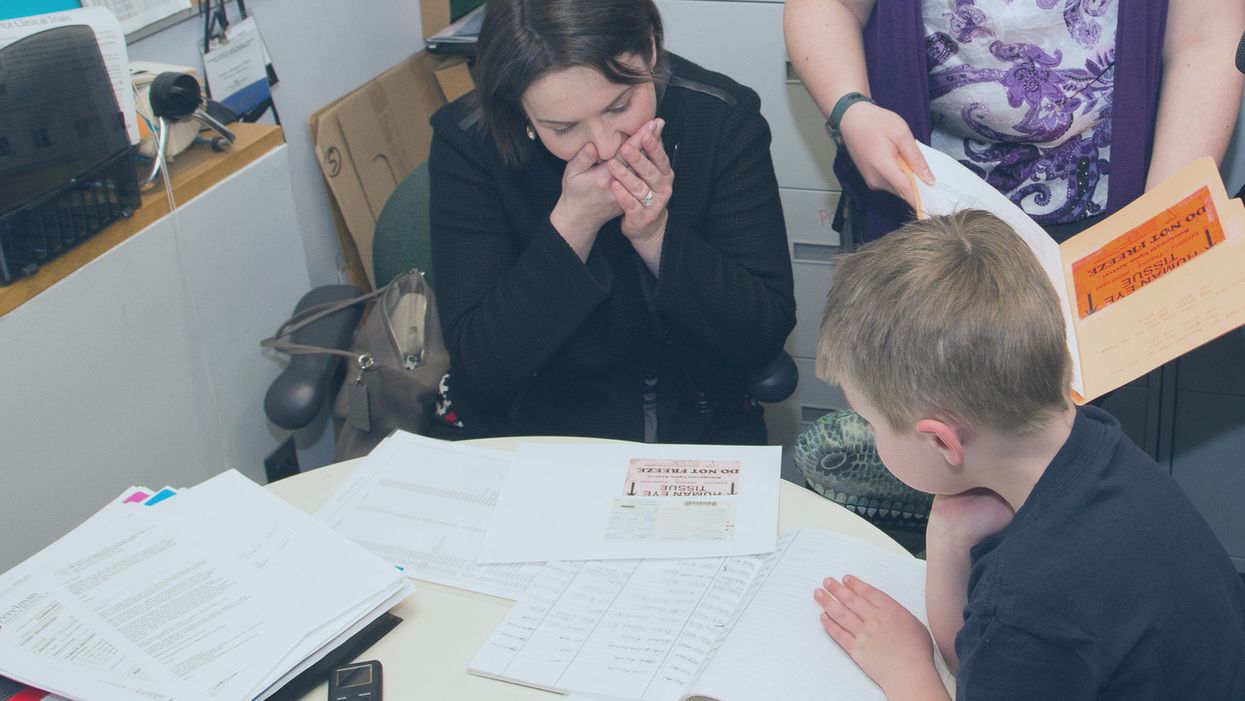
Sarah Gray views data about the use of her deceased son Thomas' retinal tissue in research for retinoblastoma, a cancer of the eye, at the University of Pennsylvania, while her son Callum looks on.
The twin boys growing within her womb filled Sarah Gray with both awe and dread. The sonogram showed that one, Callum, seemed to be the healthy child she and husband Ross had long sought; the other, Thomas, had anencephaly, a fatal developmental disorder of the skull and brain that likely would limit his life to hours. The options were to carry the boys to term or terminate both.
The decision to donate Thomas' tissue to research comforted Sarah. It brought a sense of purpose and meaning to her son's anticipated few breaths.
Sarah learned that researchers prize tissue as essential to better understanding and eventually treating the rare disorder that afflicted her son. And that other tissue from the developing infant might prove useful for transplant or basic research.
Animal models have been useful in figuring out some of the basics of genetics and how the body responds to disease. But a mouse is not a man. The new tools of precision medicine that measure gene expression, proteins and metabolites – the various chemical products and signals that fluctuate in health and illness – are most relevant when studying human tissue directly rather than in animals.
The decision to donate Thomas' tissue to research comforted Sarah. It brought a sense of purpose and meaning to her son's anticipated few breaths.

Thomas Gray
(Photo credit: Mark Walpole)
Later Sarah would track down where some of the donated tissues had been sent and how they were being used. It was a rare initiative that just may spark a new kind of relationship between donor families and researchers who use human tissue.
Organ donation for transplant gets all the attention. That process is simple, direct, life saving, the stories are easy to understand and play out regularly in the media. Reimbursement fully covers costs.
Tissue donation for research is murkier. Seldom is there a direct one-to-one correlation between individual donation and discovery; often hundreds, sometimes thousands of samples are needed to tease out the basic mechanisms of a disease, even more to develop a treatment or cure. The research process can be agonizingly slow. And somebody has to pay for collecting, processing, and getting donations into the hands of appropriate researchers. That story rarely is told, so most people are not even aware it is possible, let alone vital to research.
Gray set out on a quest to follow where Thomas' tissue had gone and how it was being used to advance research and care.
The dichotomy between transplant and research became real for Sarah several months after the birth of her twins, and Thomas' brief life, at a meeting for families of transplant donors. Many of the participants had found closure to their grieving through contact with grateful recipients of a heart, liver, or kidney who had gained a new lease on life. But there was no similar process for those who donated for research. Sarah felt a bit, well, jealous. She wanted that type of connection too.
Gray set out on a quest to follow where Thomas' tissue had gone and how it was being used to advance research and care. Those encounters were as novel for the researchers as they were for Sarah. The experience turned her into an advocate for public education and financial and operational changes to put tissue donation for research on par with donations for transplant.
Thomas' retina had been collected and processed by the National Disease Research Interchange (NDRI), a nonprofit that performs such services for researchers on a cost recovery basis with support from the National Institutes of Health. The tissue was passed on to Arupa Ganguly, who is studying retinoblastoma, a cancer of the eye, at the University of Pennsylvania.
Ganguly was surprised and apprehensive months later when NDRI emailed her saying the mother of donated tissue wanted to learn more about how the retina was being used. That was unusual because research donations generally are anonymous.
The geneticist waited a day or two, then wrote an explanation of her work and forwarded it back through NDRI. Soon the researcher and mother were talking by phone and Sarah would visit the lab. Even then, Ganguly felt very uncomfortable. "Something very bad happened to your son Thomas but it was a benefit for me, so I'm feeling very bad," she told Sarah.
"And Sarah said, Arupa, you were the only ones who wanted his retinas. If you didn't request them, they would be buried in the ground. It gives me a sense of fulfillment to know that they were of some use," Ganguly recalls. And her apprehension melted away. The two became friends and have visited several times.

Sarah Gray visits Dr. Arupa Ganguly at the University of Pennsylvania's Genetic Diagnostic Laboratory.
(Photo credit: Daniel Burke)
Reading Sarah Gray's story led Gregory Grossman to reach out to the young mother and to create Hope and Healing, a program that brings donors and researchers together. Grossman is director of research programs at Eversight, a large network of eye banks that stretches from the Midwest to the East Coast. It supplies tissue for transplant and ocular research.
"Research seems a cold and distant thing," Grossman says, "we need to educate the general public on the importance and need for tissue donations for research, which can help us better understand disease and find treatments."
"Our own internal culture needs to be shifted too," he adds. "Researchers and surgeons can forget that these are precious gifts, they're not a commodity, they're not manufactured. Without people's generosity this doesn't exist."
The initial Hope and Healing meetings between researchers and donor families have gone well and Grossman hopes to increase them to three a year with support from the Lions Club. He sees it as a crucial element in trying to reverse the decline in ocular donations even while research needs continue to grow.
What people hear about is "Tuskegee, Henrietta Lacks, they hear about the scandals, they don't hear about the good news. I would like to change that."
Since writing about her experience in the 2016 book "A Life Everlasting," Gray has come to believe that potential donor families, and even people who administer donation programs, often are unaware of the possibility of donating for research.
And roadblocks are common for those who seek to do so. Just like her, many families have had to be persistent in their quest to donate, and even educate their medical providers. But Sarah believes the internet is facilitating creation of a grassroots movement of empowered donors who are pushing procurement systems to be more responsive to their desires to donate for research. A lot of it comes through anecdote, stories, and people asking, if they have done it in Virginia, or Ohio, why can't we do it here?

Callum Gray and Dr. Arupa Ganguly hug during his family's visit to the lab.
(Photo credit: Daniel Burke)
Gray has spoken at medical and research facilities and at conferences. Some researchers are curious to have contact with the families of donors, but she believes the research system fosters the belief that "you don't want to open that can of worms." And lurking in the background may be a fear of liability issues somehow arising.
"I believe that 99 percent of what happens in research is very positive, and those stories would come out if the connections could be made," says Sarah Gray. But what they hear about is "Tuskegee, Henrietta Lacks, they hear about the scandals, they don't hear about the good news. I would like to change that."
This man spent over 70 years in an iron lung. What he was able to accomplish is amazing.
Paul Alexander spent more than 70 years confined to an iron lung after a polio infection left him paralyzed at age 6. Here, Alexander uses a mirror attached to the top of his iron lung to view his surroundings.
It’s a sight we don’t normally see these days: A man lying prone in a big, metal tube with his head sticking out of one end. But it wasn’t so long ago that this sight was unfortunately much more common.
In the first half of the 20th century, tens of thousands of people each year were infected by polio—a highly contagious virus that attacks nerves in the spinal cord and brainstem. Many people survived polio, but a small percentage of people who did were left permanently paralyzed from the virus, requiring support to help them breathe. This support, known as an “iron lung,” manually pulled oxygen in and out of a person’s lungs by changing the pressure inside the machine.
Paul Alexander was one of several thousand who were infected and paralyzed by polio in 1952. That year, a polio epidemic swept the United States, forcing businesses to close and polio wards in hospitals all over the country to fill up with sick children. When Paul caught polio in the summer of 1952, doctors urged his parents to let him rest and recover at home, since the hospital in his home suburb of Dallas, Texas was already overrun with polio patients.
Paul rested in bed for a few days with aching limbs and a fever. But his condition quickly got worse. Within a week, Paul could no longer speak or swallow, and his parents rushed him to the local hospital where the doctors performed an emergency procedure to help him breathe. Paul woke from the surgery three days later, and found himself unable to move and lying inside an iron lung in the polio ward, surrounded by rows of other paralyzed children.

But against all odds, Paul lived. And with help from a physical therapist, Paul was able to thrive—sometimes for small periods outside the iron lung.
The way Paul did this was to practice glossopharyngeal breathing (or as Paul called it, “frog breathing”), where he would trap air in his mouth and force it down his throat and into his lungs by flattening his tongue. This breathing technique, taught to him by his physical therapist, would allow Paul to leave the iron lung for increasing periods of time.
With help from his iron lung (and for small periods of time without it), Paul managed to live a full, happy, and sometimes record-breaking life. At 21, Paul became the first person in Dallas, Texas to graduate high school without attending class in person, owing his success to memorization rather than taking notes. After high school, Paul received a scholarship to Southern Methodist University and pursued his dream of becoming a trial lawyer and successfully represented clients in court.

Throughout his long life, Paul was also able to fly on a plane, visit the beach, adopt a dog, fall in love, and write a memoir using a plastic stick to tap out a draft on a keyboard. In recent years, Paul joined TikTok and became a viral sensation with more than 330,000 followers. In one of his first videos, Paul advocated for vaccination and warned against another polio epidemic.
Paul was reportedly hospitalized with COVID-19 at the end of February and died on March 11th, 2024. He currently holds the Guiness World Record for longest survival inside an iron lung—71 years.
Polio thankfully no longer circulates in the United States, or in most of the world, thanks to vaccines. But Paul continues to serve as a reminder of the importance of vaccination—and the power of the human spirit.
““I’ve got some big dreams. I’m not going to accept from anybody their limitations,” he said in a 2022 interview with CNN. “My life is incredible.”
When doctors couldn’t stop her daughter’s seizures, this mom earned a PhD and found a treatment herself.
Savannah Salazar (left) and her mother, Tracy Dixon-Salazaar, who earned a PhD in neurobiology in the quest for a treatment of her daughter's seizure disorder.
Twenty-eight years ago, Tracy Dixon-Salazaar woke to the sound of her daughter, two-year-old Savannah, in the midst of a medical emergency.
“I entered [Savannah’s room] to see her tiny little body jerking about violently in her bed,” Tracy said in an interview. “I thought she was choking.” When she and her husband frantically called 911, the paramedic told them it was likely that Savannah had had a seizure—a term neither Tracy nor her husband had ever heard before.
Over the next several years, Savannah’s seizures continued and worsened. By age five Savannah was having seizures dozens of times each day, and her parents noticed significant developmental delays. Savannah was unable to use the restroom and functioned more like a toddler than a five-year-old.
Doctors were mystified: Tracy and her husband had no family history of seizures, and there was no event—such as an injury or infection—that could have caused them. Doctors were also confused as to why Savannah’s seizures were happening so frequently despite trying different seizure medications.
Doctors eventually diagnosed Savannah with Lennox-Gaustaut Syndrome, or LGS, an epilepsy disorder with no cure and a poor prognosis. People with LGS are often resistant to several kinds of anti-seizure medications, and often suffer from developmental delays and behavioral problems. People with LGS also have a higher chance of injury as well as a higher chance of sudden unexpected death (SUDEP) due to the frequent seizures. In about 70 percent of cases, LGS has an identifiable cause such as a brain injury or genetic syndrome. In about 30 percent of cases, however, the cause is unknown.
Watching her daughter struggle through repeated seizures was devastating to Tracy and the rest of the family.
“This disease, it comes into your life. It’s uninvited. It’s unannounced and it takes over every aspect of your daily life,” said Tracy in an interview with Today.com. “Plus it’s attacking the thing that is most precious to you—your kid.”
Desperate to find some answers, Tracy began combing the medical literature for information about epilepsy and LGS. She enrolled in college courses to better understand the papers she was reading.
“Ironically, I thought I needed to go to college to take English classes to understand these papers—but soon learned it wasn’t English classes I needed, It was science,” Tracy said. When she took her first college science course, Tracy says, she “fell in love with the subject.”
Tracy was now a caregiver to Savannah, who continued to have hundreds of seizures a month, as well as a full-time student, studying late into the night and while her kids were at school, using classwork as “an outlet for the pain.”
“I couldn’t help my daughter,” Tracy said. “Studying was something I could do.”
Twelve years later, Tracy had earned a PhD in neurobiology.
After her post-doctoral training, Tracy started working at a lab that explored the genetics of epilepsy. Savannah’s doctors hadn’t found a genetic cause for her seizures, so Tracy decided to sequence her genome again to check for other abnormalities—and what she found was life-changing.
Tracy discovered that Savannah had a calcium channel mutation, meaning that too much calcium was passing through Savannah’s neural pathways, leading to seizures. The information made sense to Tracy: Anti-seizure medications often leech calcium from a person’s bones. When doctors had prescribed Savannah calcium supplements in the past to counteract these effects, her seizures had gotten worse every time she took the medication. Tracy took her discovery to Savannah’s doctor, who agreed to prescribe her a calcium blocker.
The change in Savannah was almost immediate.
Within two weeks, Savannah’s seizures had decreased by 95 percent. Once on a daily seven-drug regimen, she was soon weaned to just four, and then three. Amazingly, Tracy started to notice changes in Savannah’s personality and development, too.
“She just exploded in her personality and her talking and her walking and her potty training and oh my gosh she is just so sassy,” Tracy said in an interview.
Since starting the calcium blocker eleven years ago, Savannah has continued to make enormous strides. Though still unable to read or write, Savannah enjoys puzzles and social media. She’s “obsessed” with boys, says Tracy. And while Tracy suspects she’ll never be able to live independently, she and her daughter can now share more “normal” moments—something she never anticipated at the start of Savannah’s journey with LGS. While preparing for an event, Savannah helped Tracy get ready.
“We picked out a dress and it was the first time in our lives that we did something normal as a mother and a daughter,” she said. “It was pretty cool.”

