Would You Eat These Futuristic Foods?
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

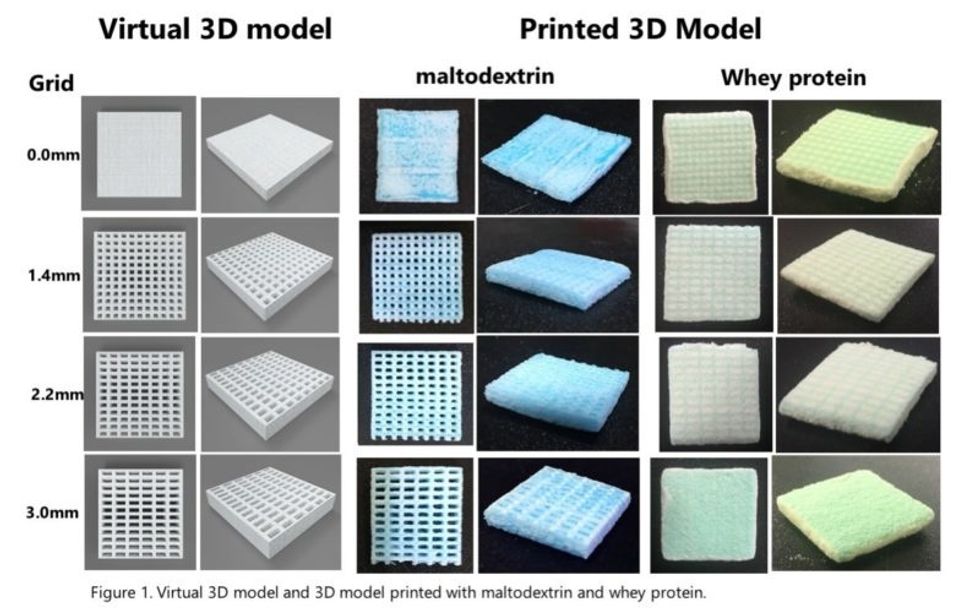
A rendering of a 3D-printed burger.
Imagine it's 2050. You wake up and make breakfast: fluffy scrambled eggs that didn't come from a chicken, but that taste identical to the ones you remember eating as a kid. You would never know that the egg protein on your plate, ovalbumin, was developed in an industrial bioreactor using fungi.
"We have this freedom to operate, freedom to engineer way beyond what we have now with livestock or plants."
For lunch, you head to your kitchen's 3D printer and pop in a cartridge, select your preferred texture and flavor, then stand back while your meal is chemically assembled. Afterward, for dessert, you snack on some chocolate that tastes more delicious than the truffles of the past. That's because these cocoa beans were gene-edited to improve their flavor.
2050 is not a random year –it's when the United Nations estimates that the world population will have ballooned to nearly 10 billion people. That's a staggering number of mouths to feed. So, scientists are already working on ways to make new food products that are unlike anything we consume today, but that could offer new, potentially improved nutritional choices and sustainable options for the masses. To whet your appetite, here are three futuristic types of food that are currently in development around the world:
1) Cellular Agriculture
Researchers at VTT Technical Research Centre of Finland, a leading R&D organization in Europe, are on the cutting-edge of developing a whole new ecosystem of food with novel ingredients and novel functionality.
In the high-tech world of cellular agriculture, single-cell organisms can be used in contained environments to produce food ingredients that are identical to traditionally sourced ingredients. For example, whey protein can be developed inside a bioreactor that is functionally the same as the kind in cow's milk.
Ditto for eggs without a chicken – so the world will finally know which came first.

The steel tank bioreactors in VTT´s piloting facility are used to grow larger amounts of plant cells or to brew dairy and egg proteins with microbes.
(VTT)
"We take the gene from a chicken genome, and place that in a microbe, and then the microbe can, with those instructions, make exactly the same protein," explains Lauri Reuter, a Senior Specialist at VTT who holds a doctorate in biotechnology. "It will swim in this bioreactor and kick out the protein, and we get this liquid that can be purified. Then you would cook or bake with it, and the food you would eat tastes and looks like food you would eat right now."
But why settle for what chickens can do? With this technology, it's possible, for example, to modify the ovalbumin protein to decrease its allergenicity.
"This is the power of what we can do with modern tools of genetic engineering," says Christopher Landowski,a Research Team Leader of the Protein Production Team. And the innovative potential doesn't stop there.
"We have this freedom to operate, freedom to engineer way beyond what we have now with livestock or plants," Reuter says. Future foods sourced from cells could include meat analogues, sugar substitutes, dairy substitutes, nutritious veggies that don't taste bitter, personalized nutrition – ingredients designed for individual needs; the list goes on. It could even be used one day to produce food on Mars.
The researchers emphasize the advantages of this method: their living cell factories are efficient – no care of complex animals is required; they can scale up or down in reaction to demand; their environments are contained and don't require antibiotics; and they provide an alternative to using animals.
But the researchers also readily admit that the biggest obstacle is consumer acceptance, which is why they seek to engage with people along the way to alleviate any concerns and to educate them about the technology. Novel foods of this sort have already been eaten in research settings, but it may take another three to five years before the egg and milk proteins hit the market, probably first in the United States before Europe.
Eventually, the researchers anticipate widespread adoption.
Emilia Nordlund, who directs the Food Solutions team, predicts, "Cellular agriculture will revolutionize the food industry as dramatically as the Internet revolutionized many other industries."

Jams made of culture cells of various plants: strawberry, scurvy grass, arctic bramble, tobacco, cloudberry and lingonberry.
(VTT/Lauri Reuter)
2) 3D-printed foods
In South Korea, researchers are developing 3D-printed foods to help solve a problem caused by aging. Elderly people often rely on soft foods which are easier to chew, but aren't always healthy, like Jello and pudding.
With 3D printing, foods of softer textures can be created with the same nutritional value as firmer food, via a processing method that breaks down the food into tiny nutrients by grinding it at a very low temperature with liquid nitrogen.
"The goal is that someone at home can print out food with whatever flavor and texture they want."
The micro-sized food materials are then reconstructed in layers to form what looks like a Lego block. "The cartridges are all textures, some soft and some stiff," explains Jin-Kyu Rhee, associate professor at Ewha Womans University, whose project has been funded for the last three years by the South Korean government. "We are developing a library of food textures, so that people can combine them to simulate a real type of food."
Users could then add powdered versions of various ingredients to create customized food. Flavor, of course, is of prime importance too, so the cartridges have flavors like barbecue to help simulate the experience of eating "real" food.
"The goal is that someone at home can print out food with whatever flavor and texture they want," Rhee says. "They can order their own cartridge and digital recipes to generate their own food, ready to cook with a microwave oven." It could also be used for space travel.
Rhee expects the prototype of the printer to be completed by the end of this year and will then seek out a commercial partner. If all goes well, you might be able to set up your 3D printer next to your coffee pot by 2025.
3) CRISPR-edited foods
You may not know that the cocoa plant is having a tough time out there in nature. It's plagued by fungal disease; on farms, about 30 to 40 percent of the potential cocoa beans are lost every year. For all the chocolate lovers of the world, this means less to go around.
Conventional plant breeding is very slow for trees, so researchers like Mark Guiltinan at Penn State University are devising ways to increase the plants' chances for survival – without moving any genes between species, as in genetically modified organisms (GMOs).
"Because society hasn't really embraced [GMOs] very much, we're trying to develop ways that don't use transgenic plants and speed up breeding," Guiltinan says.
He and his colleagues are using CRISPR-cas9, the precise method of editing DNA, to imbue cocoa plants with immunity to fungal disease.
How does it work? Similar to humans, the plants have an immune system. Part of it functions like brakes, repressing the whole system so it's only working when it needs to.
"Like when you get a fever, your immune system is working full blast, but your body shuts it down when it doesn't need it," he explains. "Plants do exactly the same thing. One idea is if we can reduce or eliminate that brake on the immune system, we could make plants that have a very high immunity."

A CRISPR-edited npr3 mutant cacao plantlet, not too much to see yet, but soon it will become a happy plant in the greenhouse.
(Photo credit: Mark Guiltinan)
The CRISPR-cas9 system allows "a really amazing little protein" to go into the cocoa plant cell, find a specific gene, and shut it off to put the whole immune system into overdrive. This confers the necessary immunity, and though the plant burns through a lot of energy, as if it has a fever all the time, this method would allow for more plants to fend off the fungal attacks every year. Which means more chocolate. It could also greatly reduce the need for pesticides.
"Replacing chemicals with genetics is one part of our goal," Guiltinan says. "And it's totally safe." Another goal of his project is to improve the cocoa beans' quality and flavor profile through gene editing.
Yum. Is your mouth watering yet?
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
A new type of cancer therapy is shrinking deadly brain tumors with just one treatment
MRI scans after a new kind of immunotherapy for brain cancer show remarkable progress in one patient just days after the first treatment.
Few cancers are deadlier than glioblastomas—aggressive and lethal tumors that originate in the brain or spinal cord. Five years after diagnosis, less than five percent of glioblastoma patients are still alive—and more often, glioblastoma patients live just 14 months on average after receiving a diagnosis.
But an ongoing clinical trial at Mass General Cancer Center is giving new hope to glioblastoma patients and their families. The trial, called INCIPIENT, is meant to evaluate the effects of a special type of immune cell, called CAR-T cells, on patients with recurrent glioblastoma.
How CAR-T cell therapy works
CAR-T cell therapy is a type of cancer treatment called immunotherapy, where doctors modify a patient’s own immune system specifically to find and destroy cancer cells. In CAR-T cell therapy, doctors extract the patient’s T-cells, which are immune system cells that help fight off disease—particularly cancer. These T-cells are harvested from the patient and then genetically modified in a lab to produce proteins on their surface called chimeric antigen receptors (thus becoming CAR-T cells), which makes them able to bind to a specific protein on the patient’s cancer cells. Once modified, these CAR-T cells are grown in the lab for several weeks so that they can multiply into an army of millions. When enough cells have been grown, these super-charged T-cells are infused back into the patient where they can then seek out cancer cells, bind to them, and destroy them. CAR-T cell therapies have been approved by the US Food and Drug Administration (FDA) to treat certain types of lymphomas and leukemias, as well as multiple myeloma, but haven’t been approved to treat glioblastomas—yet.
CAR-T cell therapies don’t always work against solid tumors, such as glioblastomas. Because solid tumors contain different kinds of cancer cells, some cells can evade the immune system’s detection even after CAR-T cell therapy, according to a press release from Massachusetts General Hospital. For the INCIPIENT trial, researchers modified the CAR-T cells even further in hopes of making them more effective against solid tumors. These second-generation CAR-T cells (called CARv3-TEAM-E T cells) contain special antibodies that attack EFGR, a protein expressed in the majority of glioblastoma tumors. Unlike other CAR-T cell therapies, these particular CAR-T cells were designed to be directly injected into the patient’s brain.
The INCIPIENT trial results
The INCIPIENT trial involved three patients who were enrolled in the study between March and July 2023. All three patients—a 72-year-old man, a 74-year-old man, and a 57-year-old woman—were treated with chemo and radiation and enrolled in the trial with CAR-T cells after their glioblastoma tumors came back.
The results, which were published earlier this year in the New England Journal of Medicine (NEJM), were called “rapid” and “dramatic” by doctors involved in the trial. After just a single infusion of the CAR-T cells, each patient experienced a significant reduction in their tumor sizes. Just two days after receiving the infusion, the glioblastoma tumor of the 72-year-old man decreased by nearly twenty percent. Just two months later the tumor had shrunk by an astonishing 60 percent, and the change was maintained for more than six months. The most dramatic result was in the 57-year-old female patient, whose tumor shrank nearly completely after just one infusion of the CAR-T cells.
The results of the INCIPIENT trial were unexpected and astonishing—but unfortunately, they were also temporary. For all three patients, the tumors eventually began to grow back regardless of the CAR-T cell infusions. According to the press release from MGH, the medical team is now considering treating each patient with multiple infusions or prefacing each treatment with chemotherapy to prolong the response.
While there is still “more to do,” says co-author of the study neuro-oncologist Dr. Elizabeth Gerstner, the results are still promising. If nothing else, these second-generation CAR-T cell infusions may someday be able to give patients more time than traditional treatments would allow.
“These results are exciting but they are also just the beginning,” says Dr. Marcela Maus, a doctor and professor of medicine at Mass General who was involved in the clinical trial. “They tell us that we are on the right track in pursuing a therapy that has the potential to change the outlook for this intractable disease.”
A recent study in The Lancet Oncology showed that AI found 20 percent more cancers on mammogram screens than radiologists alone.
Since the early 2000s, AI systems have eliminated more than 1.7 million jobs, and that number will only increase as AI improves. Some research estimates that by 2025, AI will eliminate more than 85 million jobs.
But for all the talk about job security, AI is also proving to be a powerful tool in healthcare—specifically, cancer detection. One recently published study has shown that, remarkably, artificial intelligence was able to detect 20 percent more cancers in imaging scans than radiologists alone.
Published in The Lancet Oncology, the study analyzed the scans of 80,000 Swedish women with a moderate hereditary risk of breast cancer who had undergone a mammogram between April 2021 and July 2022. Half of these scans were read by AI and then a radiologist to double-check the findings. The second group of scans was read by two researchers without the help of AI. (Currently, the standard of care across Europe is to have two radiologists analyze a scan before diagnosing a patient with breast cancer.)
The study showed that the AI group detected cancer in 6 out of every 1,000 scans, while the radiologists detected cancer in 5 per 1,000 scans. In other words, AI found 20 percent more cancers than the highly-trained radiologists.

But even though the AI was better able to pinpoint cancer on an image, it doesn’t mean radiologists will soon be out of a job. Dr. Laura Heacock, a breast radiologist at NYU, said in an interview with CNN that radiologists do much more than simply screening mammograms, and that even well-trained technology can make errors. “These tools work best when paired with highly-trained radiologists who make the final call on your mammogram. Think of it as a tool like a stethoscope for a cardiologist.”
AI is still an emerging technology, but more and more doctors are using them to detect different cancers. For example, researchers at MIT have developed a program called MIRAI, which looks at patterns in patient mammograms across a series of scans and uses an algorithm to model a patient's risk of developing breast cancer over time. The program was "trained" with more than 200,000 breast imaging scans from Massachusetts General Hospital and has been tested on over 100,000 women in different hospitals across the world. According to MIT, MIRAI "has been shown to be more accurate in predicting the risk for developing breast cancer in the short term (over a 3-year period) compared to traditional tools." It has also been able to detect breast cancer up to five years before a patient receives a diagnosis.
The challenges for cancer-detecting AI tools now is not just accuracy. AI tools are also being challenged to perform consistently well across different ages, races, and breast density profiles, particularly given the increased risks that different women face. For example, Black women are 42 percent more likely than white women to die from breast cancer, despite having nearly the same rates of breast cancer as white women. Recently, an FDA-approved AI device for screening breast cancer has come under fire for wrongly detecting cancer in Black patients significantly more often than white patients.
As AI technology improves, radiologists will be able to accurately scan a more diverse set of patients at a larger volume than ever before, potentially saving more lives than ever.

