23andMe Is Using Customers’ Genetic Data to Develop Drugs. Is This Brilliant or Dubious?

A woman does a DNA test with a cotton swab at home.
Leading direct-to-consumer (DTC) genetic testing companies are continuously unveiling novel ways to leverage their vast stores of genetic data.
"23andMe will tell you what diseases you have and then sell you the drugs to treat them."
As reported last week, 23andMe's latest concept is to develop and license new drugs using the data of consumers who have opted in to let their information be used for research. To date, over 10 million people have used the service and around 80 percent have opted in, making its database one of the largest in the world.
Culture researcher Dr. Julia Creet is one of the foremost experts on the DTC genetic testing industry, and in her forthcoming book, The Genealogical Sublime, she bluntly examines whether such companies' motives and interests are in sync with those of consumers.
Leapsmag caught up with Creet about the latest news and the wider industry's implications for health and privacy.
23andMe has just announced that it plans to license a newly developed anti-inflammatory drug, the first one created using its customers' genetic data, to Almirall, a pharma company in Spain. What's your take?
I think this development is the next step in the evolution of the company and its "double-sided" marketing model. In the past, as it enticed customers to give it their DNA, it sold the results and the medical information divulged by customers to other drug companies. Now it is positioning itself to reap the profits of a new model by developing treatments itself.
Given that there are many anti-inflammatory drugs on the market already, whatever Almirall produces might not have much of an impact. We might see this canny move as a "proof of concept," that 23andMe has learned how to "leverage" its genetic data without having to sell them to a third party. In a way, the privacy provisions will be much less complicated, and the company stands to attract investment as it turns itself into [a pseudo pharmaceutical company], a "pharma-psuedocal" company.
Emily Drabant Conley, the president of business development, has said that 23andMe is pursuing other drug compounds and may conduct their own clinical trials rather than licensing them out to their existing research partners. The end goal, it seems, is to make direct-to-consumer DNA testing to drug production and sales back to that same consumer base a seamless and lucrative circle. You have to admit it's a brilliant business model. 23andMe will tell you what diseases you have and then sell you the drugs to treat them.
In your new book, you describe how DTC genetic testing companies have capitalized on our innate human desire to connect with or ancestors and each other. I quote you: "This industry has taken that potent, spiritual, all-too-human need to belong... and monetized it in a particularly exploitative way." But others argue that DTC genetic testing companies are merely providing a service in exchange for fair-market compensation. So where does exploitation come into the picture?
Yes, the industry provides a fee for service, but that's only part of the story. The rest of the story reveals a pernicious industry that hides its business model behind the larger science project of health and heredity. All of the major testing companies play on the idea of "lack," that we can't know who we are unless we buy information about ourselves. When you really think about it, "Who do you think you are?" is a pernicious question that suggests that we don't or can't know who we or to whom we are related without advanced data searches and testing. This existential question used to be a philosophical question; now the answers are provided by databases that acquire more valuable information than they provide in the exchange.
"It's a brilliant business model that exploits consumer naiveté."
As you've said before, consumers are actually paying to be the product because the companies are likely to profit more from selling their genetic data. Could you elaborate?
The largest databases, AncestryDNA and 23andMe, have signed lucrative agreements with biotech companies that pay them for the de-identified data of their customers. What's so valuable is the DNA combined with the family relationships. Consumers provide the family relationships and the companies link and extrapolate the results to larger and larger family trees. Combined with the genetic markers for certain diseases, or increased susceptibility to certain diseases, these databases are very valuable for biotech research.
None of that value will ever be returned to consumers except in the form of for-profit drugs. Ancestry, in particular, has removed all information about its "research partners" from its website, making it very difficult to see how it is profiting from its third-party sales. 23andMe is more open about its "two-sided business model," but encourages consumers to donate their information to science. It's a brilliant business model that exploits consumer naiveté.
A WIRED journalist wrote that "23andMe has been sharing insights gleaned from consented customer data with GSK and at least six other pharmaceutical and biotechnology firms for the past three and a half years." Is this a consumer privacy risk?
I don't see that 23andMe did anything to which consumers didn't consent, albeit through arguably unreadable terms and conditions. The part that worries me more is the 300 phenotype data points that the company has collected on its consumers through longitudinal surveys designed, as Anne Wojcicki, CEO and Co-founder of 23andMe, put it, "to circumvent medical records and just self-report."
Everyone is focused on the DNA, but it's the combination of genetic samples, genealogical information and health records that is the most potent dataset, and 23andMe has figured out a way to extract all three from consumers.
Dr. May Edward Chinn, Kizzmekia Corbett, PhD., and Alice Ball, among others, have been behind some of the most important scientific work of the last century.
If you look back on the last century of scientific achievements, you might notice that most of the scientists we celebrate are overwhelmingly white, while scientists of color take a backseat. Since the Nobel Prize was introduced in 1901, for example, no black scientists have landed this prestigious award.
The work of black women scientists has gone unrecognized in particular. Their work uncredited and often stolen, black women have nevertheless contributed to some of the most important advancements of the last 100 years, from the polio vaccine to GPS.
Here are five black women who have changed science forever.
Dr. May Edward Chinn
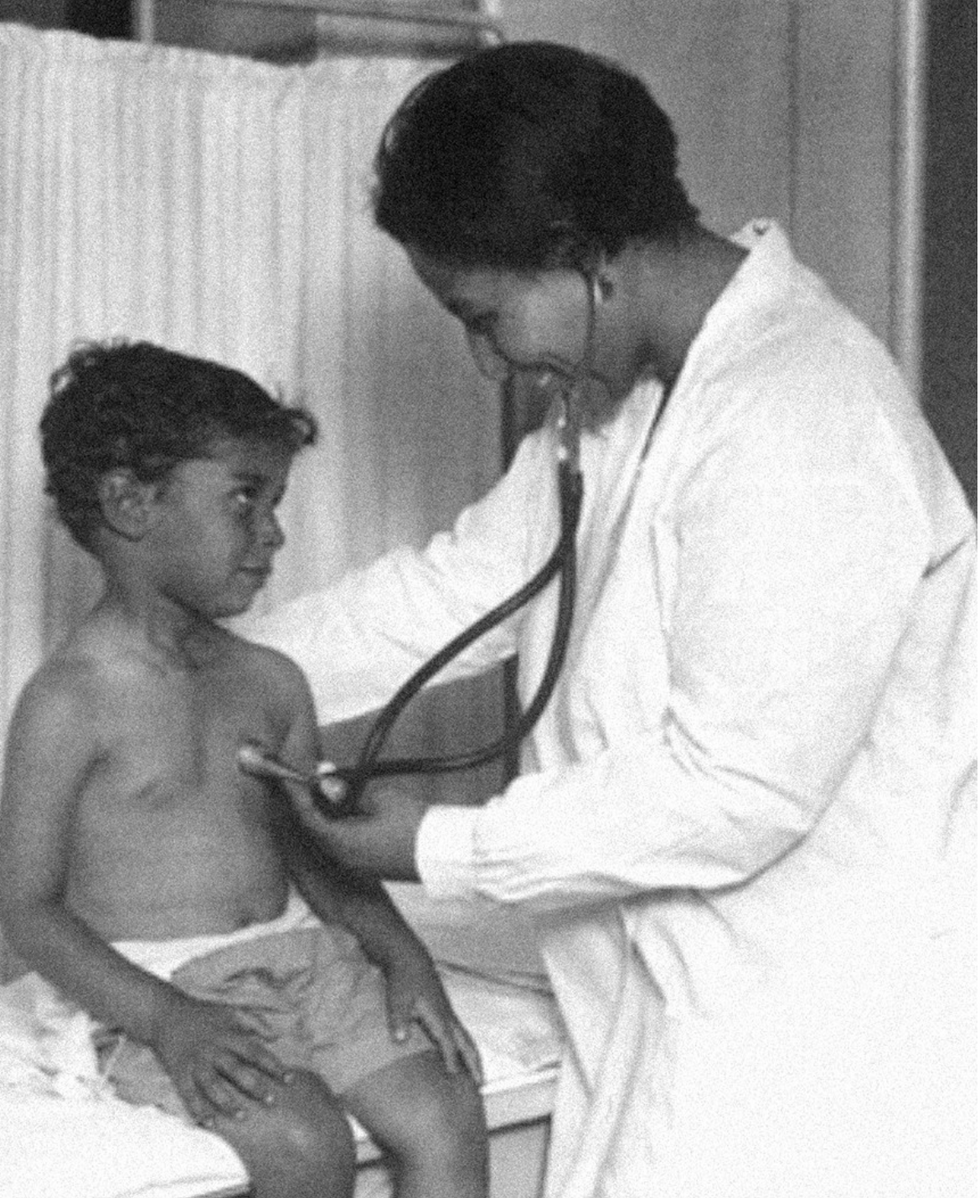
Dr. May Edward Chinn practicing medicine in Harlem
George B. Davis, PhD.
Chinn was born to poor parents in New York City just before the start of the 20th century. Although she showed great promise as a pianist, playing with the legendary musician Paul Robeson throughout the 1920s, she decided to study medicine instead. Chinn, like other black doctors of the time, were barred from studying or practicing in New York hospitals. So Chinn formed a private practice and made house calls, sometimes operating in patients’ living rooms, using an ironing board as a makeshift operating table.
Chinn worked among the city’s poor, and in doing this, started to notice her patients had late-stage cancers that often had gone undetected or untreated for years. To learn more about cancer and its prevention, Chinn begged information off white doctors who were willing to share with her, and even accompanied her patients to other clinic appointments in the city, claiming to be the family physician. Chinn took this information and integrated it into her own practice, creating guidelines for early cancer detection that were revolutionary at the time—for instance, checking patient health histories, checking family histories, performing routine pap smears, and screening patients for cancer even before they showed symptoms. For years, Chinn was the only black female doctor working in Harlem, and she continued to work closely with the poor and advocate for early cancer screenings until she retired at age 81.
Alice Ball

Pictorial Press Ltd/Alamy
Alice Ball was a chemist best known for her groundbreaking work on the development of the “Ball Method,” the first successful treatment for those suffering from leprosy during the early 20th century.
In 1916, while she was an undergraduate student at the University of Hawaii, Ball studied the effects of Chaulmoogra oil in treating leprosy. This oil was a well-established therapy in Asian countries, but it had such a foul taste and led to such unpleasant side effects that many patients refused to take it.
So Ball developed a method to isolate and extract the active compounds from Chaulmoogra oil to create an injectable medicine. This marked a significant breakthrough in leprosy treatment and became the standard of care for several decades afterward.
Unfortunately, Ball died before she could publish her results, and credit for this discovery was given to another scientist. One of her colleagues, however, was able to properly credit her in a publication in 1922.
Henrietta Lacks

onathan Newton/The Washington Post/Getty
The person who arguably contributed the most to scientific research in the last century, surprisingly, wasn’t even a scientist. Henrietta Lacks was a tobacco farmer and mother of five children who lived in Maryland during the 1940s. In 1951, Lacks visited Johns Hopkins Hospital where doctors found a cancerous tumor on her cervix. Before treating the tumor, the doctor who examined Lacks clipped two small samples of tissue from Lacks’ cervix without her knowledge or consent—something unthinkable today thanks to informed consent practices, but commonplace back then.
As Lacks underwent treatment for her cancer, her tissue samples made their way to the desk of George Otto Gey, a cancer researcher at Johns Hopkins. He noticed that unlike the other cell cultures that came into his lab, Lacks’ cells grew and multiplied instead of dying out. Lacks’ cells were “immortal,” meaning that because of a genetic defect, they were able to reproduce indefinitely as long as certain conditions were kept stable inside the lab.
Gey started shipping Lacks’ cells to other researchers across the globe, and scientists were thrilled to have an unlimited amount of sturdy human cells with which to experiment. Long after Lacks died of cervical cancer in 1951, her cells continued to multiply and scientists continued to use them to develop cancer treatments, to learn more about HIV/AIDS, to pioneer fertility treatments like in vitro fertilization, and to develop the polio vaccine. To this day, Lacks’ cells have saved an estimated 10 million lives, and her family is beginning to get the compensation and recognition that Henrietta deserved.
Dr. Gladys West

Andre West
Gladys West was a mathematician who helped invent something nearly everyone uses today. West started her career in the 1950s at the Naval Surface Warfare Center Dahlgren Division in Virginia, and took data from satellites to create a mathematical model of the Earth’s shape and gravitational field. This important work would lay the groundwork for the technology that would later become the Global Positioning System, or GPS. West’s work was not widely recognized until she was honored by the US Air Force in 2018.
Dr. Kizzmekia "Kizzy" Corbett

TIME Magazine
At just 35 years old, immunologist Kizzmekia “Kizzy” Corbett has already made history. A viral immunologist by training, Corbett studied coronaviruses at the National Institutes of Health (NIH) and researched possible vaccines for coronaviruses such as SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome).
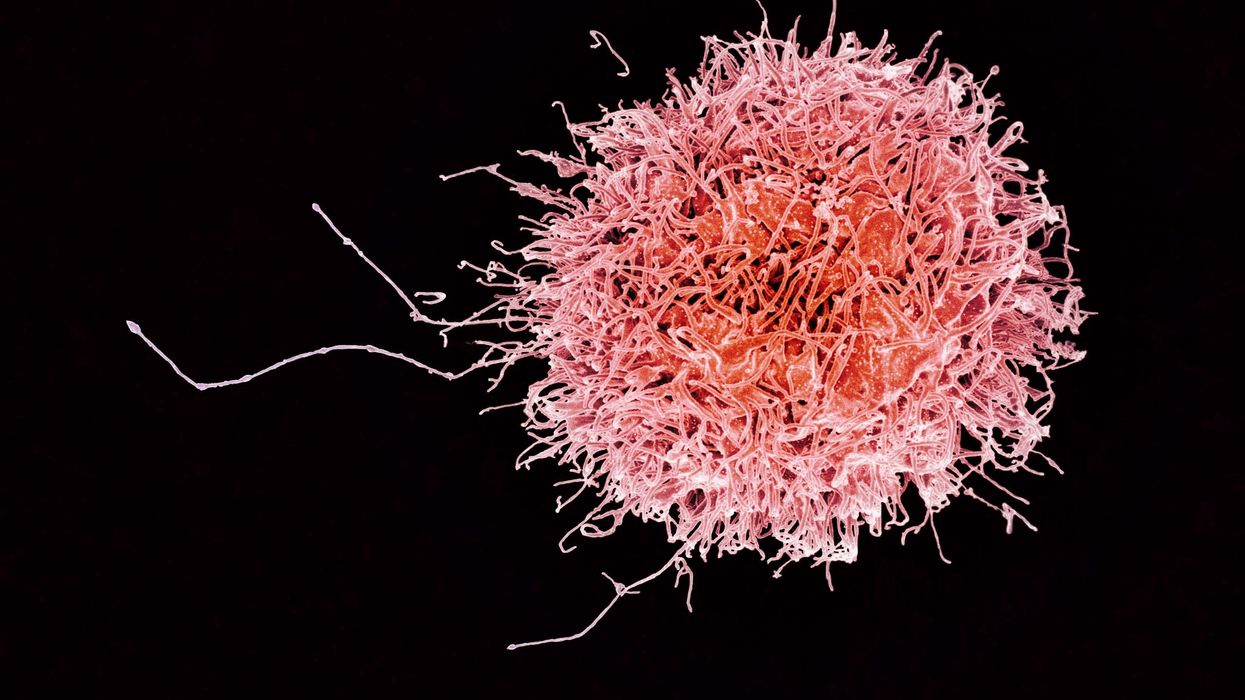
At the start of the COVID pandemic, Corbett and her team at the NIH partnered with pharmaceutical giant Moderna to develop an mRNA-based vaccine against the virus. Corbett’s previous work with mRNA and coronaviruses was vital in developing the vaccine, which became one of the first to be authorized for emergency use in the United States. The vaccine, along with others, is responsible for saving an estimated 14 million lives.On today’s episode of Making Sense of Science, I’m honored to be joined by Dr. Paul Song, a physician, oncologist, progressive activist and biotech chief medical officer. Through his company, NKGen Biotech, Dr. Song is leveraging the power of patients’ own immune systems by supercharging the body’s natural killer cells to make new treatments for Alzheimer’s and cancer.
Whereas other treatments for Alzheimer’s focus directly on reducing the build-up of proteins in the brain such as amyloid and tau in patients will mild cognitive impairment, NKGen is seeking to help patients that much of the rest of the medical community has written off as hopeless cases, those with late stage Alzheimer’s. And in small studies, NKGen has shown remarkable results, even improvement in the symptoms of people with these very progressed forms of Alzheimer’s, above and beyond slowing down the disease.
In the realm of cancer, Dr. Song is similarly setting his sights on another group of patients for whom treatment options are few and far between: people with solid tumors. Whereas some gradual progress has been made in treating blood cancers such as certain leukemias in past few decades, solid tumors have been even more of a challenge. But Dr. Song’s approach of using natural killer cells to treat solid tumors is promising. You may have heard of CAR-T, which uses genetic engineering to introduce cells into the body that have a particular function to help treat a disease. NKGen focuses on other means to enhance the 40 plus receptors of natural killer cells, making them more receptive and sensitive to picking out cancer cells.
Paul Y. Song, MD is currently CEO and Vice Chairman of NKGen Biotech. Dr. Song’s last clinical role was Asst. Professor at the Samuel Oschin Cancer Center at Cedars Sinai Medical Center.
Dr. Song served as the very first visiting fellow on healthcare policy in the California Department of Insurance in 2013. He is currently on the advisory board of the Pritzker School of Molecular Engineering at the University of Chicago and a board member of Mercy Corps, The Center for Health and Democracy, and Gideon’s Promise.
Dr. Song graduated with honors from the University of Chicago and received his MD from George Washington University. He completed his residency in radiation oncology at the University of Chicago where he served as Chief Resident and did a brachytherapy fellowship at the Institute Gustave Roussy in Villejuif, France. He was also awarded an ASTRO research fellowship in 1995 for his research in radiation inducible gene therapy.
With Dr. Song’s leadership, NKGen Biotech’s work on natural killer cells represents cutting-edge science leading to key findings and important pieces of the puzzle for treating two of humanity’s most intractable diseases.
Show links
- Paul Song LinkedIn
- NKGen Biotech on Twitter - @NKGenBiotech
- NKGen Website: https://nkgenbiotech.com/
- NKGen appoints Paul Song
- Patient Story: https://pix11.com/news/local-news/long-island/promising-new-treatment-for-advanced-alzheimers-patients/
- FDA Clearance: https://nkgenbiotech.com/nkgen-biotech-receives-ind-clearance-from-fda-for-snk02-allogeneic-natural-killer-cell-therapy-for-solid-tumors/Q3 earnings data: https://www.nasdaq.com/press-release/nkgen-biotech-inc.-reports-third-quarter-2023-financial-results-and-business