A Surprising Breakthrough Will Allow Tiny Implants to Fix—and Even Upgrade—Your Body

The medical implants of the future will prompt lively discussion around the boundaries between treatment and enhancement.
Imagine it's the year 2040 and you're due for your regular health checkup. Time to schedule your next colonoscopy, Pap smear if you're a woman, and prostate screen if you're a man.
"The evolution of the biological ion transistor technology is a game changer."
But wait, you no longer need any of those, since you recently got one of the new biomed implants – a device that integrates seamlessly with body tissues, because of a watershed breakthrough that happened in the early 2020s. It's an improved biological transistor driven by electrically charged particles that move in and out of your own cells. Like insulin pumps and cardiac pacemakers, the medical implants of the future will go where they are needed, on or inside the body.
But unlike current implants, biological transistors will have a remarkable range of applications. Currently small enough to fit between a patient's hair follicles, the devices could one day enable correction of problems ranging from damaged heart muscle to failing retinas to deficiencies of hormones and enzymes.
Their usefulness raises the prospect of overcorrection to the point of human enhancement, as in the bionic parts that were imagined on the ABC television series The Six Million Dollar Man, which aired in the 1970s.
"The evolution of the biological ion transistor technology is a game changer," says Zoltan Istvan, who ran as a U.S. Presidential candidate in 2016 for the Transhumanist Party and later ran for California governor. Istvan envisions humans becoming faster, stronger, and increasingly more capable by way of technological innovations, especially in the biotechnology realm. "It's a big step forward on how we can improve and upgrade the human body."
How It Works
The new transistors are more like the soft, organic machines that biology has evolved than like traditional transistors built of semiconductors and metal, according to electric engineering expert Dion Khodagholy, one of the leaders of the team at Columbia University that developed the technology.
The key to the advance, notes Khodagholy, is that the transistors will interface seamlessly with tissue, because the electricity will be of the biological type -- transmitted via the flow of ions through liquid, rather than electrons through metal. This will boost the sensitivity of detection and decoding of biological change.
Naturally, such a paradigm change in the world of medical devices raises potential societal and ethical dilemmas.
Known as an ion-gated transistor (IGT), the new class of technology effectively melds electronics with molecules of human skin. That's the current prototype, but ultimately, biological devices will be able to go anywhere in the body. "IGT-based devices hold great promise for development of fully implantable bioelectronic devices that can address key clinical issues for patients with neuropsychiatric disease," says Khodagholy, based on the expectation that future devices could fuse with, measure, and modulate cells of the human nervous system.
Ethical Implications
Naturally, such a paradigm change in the world of medical devices raises potential societal and ethical dilemmas, starting with who receives the new technology and who pays for it. But, according clinical ethicist and health care attorney David Hoffman, we can gain insight from past experience, such as how society reacted to the invention of kidney dialysis in the mid 20th century.
"Kidney dialysis has been federally funded for all these decades, largely because the who-gets-the-technology question was an issue when the technology entered clinical medicine," says Hoffman, who teaches bioethics at Columbia's College of Physicians and Surgeons as well as at the law school and medical school of Yeshiva University. Just as dialysis became a necessity for many patients, he suggests that the emerging bio-transistors may also become critical life-sustaining devices, prompting discussions about federal coverage.
But unlike dialysis, biological transistors could allow some users to become "better than well," making it more similar to medication for ADHD (attention deficit hyperactivity disorder): People who don't require it can still use it to improve their baseline normal functioning. This raises the classic question: Should society draw a line between treatment and enhancement? And who gets to decide the answer?
If it's strictly a medical use of the technology, should everyone who needs it get to use it, regardless of ability to pay, relying on federal or private insurance coverage? On the other hand, if it's used voluntarily for enhancement, should that option also be available to everyone -- but at an upfront cost?
From a transhumanist viewpoint, getting wrapped up with concerns about the evolution of devices from therapy to enhancement is not worth the trouble.
It seems safe to say that some lively debates and growing pains are on the horizon.
"Even if [the biological ion transistor] is developed only for medical devices that compensate for losses and deficiencies similar to that of a cardiac pacemaker, it will be hard to stop its eventual evolution from compensation to enhancement," says Istvan. "If you use it in a bionic eye to restore vision to the blind, how do you draw the line between replacement of normal function and provision of enhanced function? Do you pass a law placing limits on visual capabilities of a synthetic eye? Transhumanists would oppose such laws, and any restrictions in one country or another would allow another country to gain an advantage by creating their own real-life super human cyborg citizens."
In the same breath though, Istvan admits that biotechnology on a bionic scale is bound to complicate a range of international phenomena, from economic growth and military confrontations to sporting events like the Olympic Games.
The technology is already here, and it's just a matter of time before we see clinically viable, implantable devices. As for how society will react, it seems safe to say that some lively debates and growing pains are on the horizon.
The Friday Five: How to exercise for cancer prevention
How to exercise for cancer prevention. Plus, a device that brings relief to back pain, ingredients for reducing Alzheimer's risk, the world's oldest disease could make you young again, and more.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Here are the promising studies covered in this week's Friday Five:
- How to exercise for cancer prevention
- A device that brings relief to back pain
- Ingredients for reducing Alzheimer's risk
- Is the world's oldest disease the fountain of youth?
- Scared of crossing bridges? Your phone can help
New approach to brain health is sparking memories
This fall, Robert Reinhart of Boston University published a study finding that electrical stimulation can boost memory - and Reinhart was surprised to discover the effects lasted a full month.
What if a few painless electrical zaps to your brain could help you recall names, perform better on Wordle or even ward off dementia?
This is where neuroscientists are going in efforts to stave off age-related memory loss as well as Alzheimer’s disease. Medications have shown limited effectiveness in reversing or managing loss of brain function so far. But new studies suggest that firing up an aging neural network with electrical or magnetic current might keep brains spry as we age.
Welcome to non-invasive brain stimulation (NIBS). No surgery or anesthesia is required. One day, a jolt in the morning with your own battery-operated kit could replace your wake-up coffee.
Scientists believe brain circuits tend to uncouple as we age. Since brain neurons communicate by exchanging electrical impulses with each other, the breakdown of these links and associations could be what causes the “senior moment”—when you can’t remember the name of the movie you just watched.
In 2019, Boston University researchers led by Robert Reinhart, director of the Cognitive and Clinical Neuroscience Laboratory, showed that memory loss in healthy older adults is likely caused by these disconnected brain networks. When Reinhart and his team stimulated two key areas of the brain with mild electrical current, they were able to bring the brains of older adult subjects back into sync — enough so that their ability to remember small differences between two images matched that of much younger subjects for at least 50 minutes after the testing stopped.
Reinhart wowed the neuroscience community once again this fall. His newer study in Nature Neuroscience presented 150 healthy participants, ages 65 to 88, who were able to recall more words on a given list after 20 minutes of low-intensity electrical stimulation sessions over four consecutive days. This amounted to a 50 to 65 percent boost in their recall.
Even Reinhart was surprised to discover the enhanced performance of his subjects lasted a full month when they were tested again later. Those who benefited most were the participants who were the most forgetful at the start.

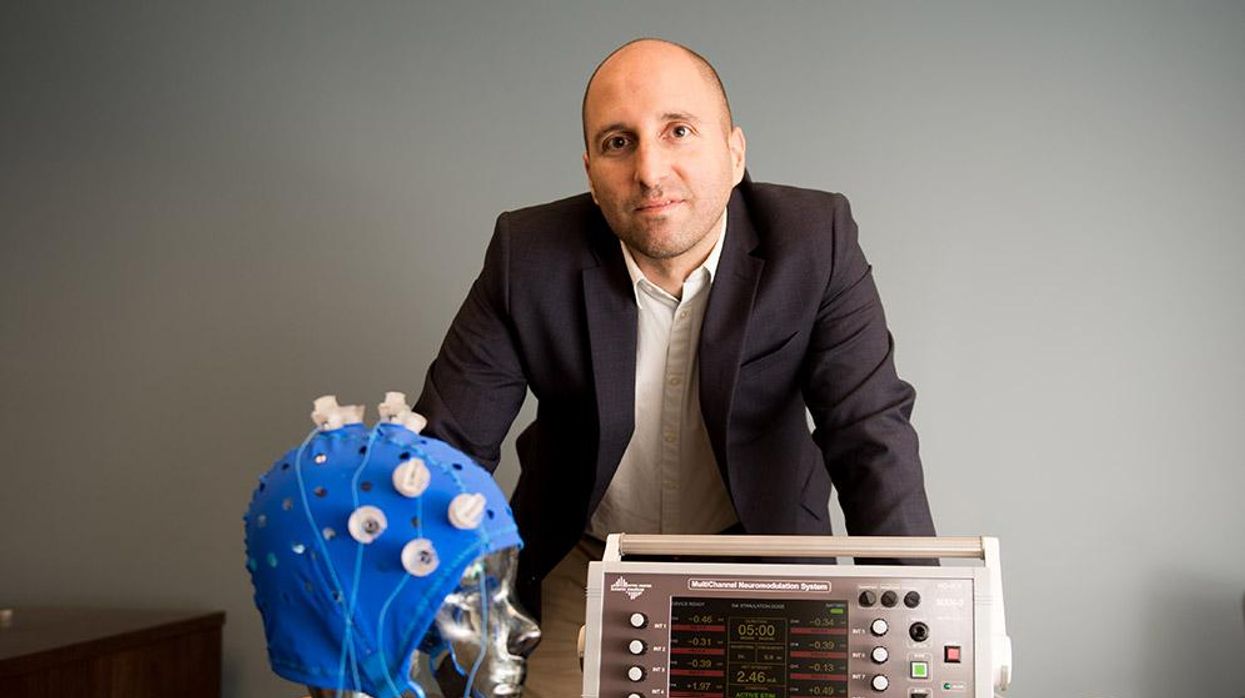
An older person participates in Robert Reinhart's research on brain stimulation.
Robert Reinhart
Reinhart’s subjects only suffered normal age-related memory deficits, but NIBS has great potential to help people with cognitive impairment and dementia, too, says Krista Lanctôt, the Bernick Chair of Geriatric Psychopharmacology at Sunnybrook Health Sciences Center in Toronto. Plus, “it is remarkably safe,” she says.
Lanctôt was the senior author on a meta-analysis of brain stimulation studies published last year on people with mild cognitive impairment or later stages of Alzheimer’s disease. The review concluded that magnetic stimulation to the brain significantly improved the research participants’ neuropsychiatric symptoms, such as apathy and depression. The stimulation also enhanced global cognition, which includes memory, attention, executive function and more.
This is the frontier of neuroscience.
The two main forms of NIBS – and many questions surrounding them
There are two types of NIBS. They differ based on whether electrical or magnetic stimulation is used to create the electric field, the type of device that delivers the electrical current and the strength of the current.
Transcranial Current Brain Stimulation (tES) is an umbrella term for a group of techniques using low-wattage electrical currents to manipulate activity in the brain. The current is delivered to the scalp or forehead via electrodes attached to a nylon elastic cap or rubber headband.
Variations include how the current is delivered—in an alternating pattern or in a constant, direct mode, for instance. Tweaking frequency, potency or target brain area can produce different effects as well. Reinhart’s 2022 study demonstrated that low or high frequencies and alternating currents were uniquely tied to either short-term or long-term memory improvements.
Sessions may be 20 minutes per day over the course of several days or two weeks. “[The subject] may feel a tingling, warming, poking or itching sensation,” says Reinhart, which typically goes away within a minute.
The other main approach to NIBS is Transcranial Magnetic Simulation (TMS). It involves the use of an electromagnetic coil that is held or placed against the forehead or scalp to activate nerve cells in the brain through short pulses. The stimulation is stronger than tES but similar to a magnetic resonance imaging (MRI) scan.
The subject may feel a slight knocking or tapping on the head during a 20-to-60-minute session. Scalp discomfort and headaches are reported by some; in very rare cases, a seizure can occur.
No head-to-head trials have been conducted yet to evaluate the differences and effectiveness between electrical and magnetic current stimulation, notes Lanctôt, who is also a professor of psychiatry and pharmacology at the University of Toronto. Although TMS was approved by the FDA in 2008 to treat major depression, both techniques are considered experimental for the purpose of cognitive enhancement.
“One attractive feature of tES is that it’s inexpensive—one-fifth the price of magnetic stimulation,” Reinhart notes.
Don’t confuse either of these procedures with the horrors of electroconvulsive therapy (ECT) in the 1950s and ‘60s. ECT is a more powerful, riskier procedure used only as a last resort in treating severe mental illness today.
Clinical studies on NIBS remain scarce. Standardized parameters and measures for testing have not been developed. The high heterogeneity among the many existing small NIBS studies makes it difficult to draw general conclusions. Few of the studies have been replicated and inconsistencies abound.
Scientists are still lacking so much fundamental knowledge about the brain and how it works, says Reinhart. “We don’t know how information is represented in the brain or how it’s carried forward in time. It’s more complex than physics.”
Lanctôt’s meta-analysis showed improvements in global cognition from delivering the magnetic form of the stimulation to people with Alzheimer’s, and this finding was replicated inan analysis in the Journal of Prevention of Alzheimer’s Disease this fall. Neither meta-analysis found clear evidence that applying the electrical currents, was helpful for Alzheimer’s subjects, but Lanctôt suggests this might be merely because the sample size for tES was smaller compared to the groups that received TMS.
At the same time, London neuroscientist Marco Sandrini, senior lecturer in psychology at the University of Roehampton, critically reviewed a series of studies on the effects of tES on episodic memory. Often declining with age, episodic memory relates to recalling a person’s own experiences from the past. Sandrini’s review concluded that delivering tES to the prefrontal or temporoparietal cortices of the brain might enhance episodic memory in older adults with Alzheimer’s disease and amnesiac mild cognitive impairment (the predementia phase of Alzheimer’s when people start to have symptoms).
Researchers readily tick off studies needed to explore, clarify and validate existing NIBS data. What is the optimal stimulus session frequency, spacing and duration? How intense should the stimulus be and where should it be targeted for what effect? How might genetics or degree of brain impairment affect responsiveness? Would adjunct medication or cognitive training boost positive results? Could administering the stimulus while someone sleeps expedite memory consolidation?
Using MRI or another brain scan along with computational modeling of the current flow, a clinician could create a treatment that is customized to each person’s brain.
While Sandrini’s review reported improvements induced by tES in the recall or recognition of words and images, there is no evidence it will translate into improvements in daily activities. This is another question that will require more research and testing, Sandrini notes.
Scientists are still lacking so much fundamental knowledge about the brain and how it works, says Reinhart. “We don’t know how information is represented in the brain or how it’s carried forward in time. It’s more complex than physics.”
Where the science is headed
Learning how to apply precision medicine to NIBS is the next focus in advancing this technology, says Shankar Tumati, a post-doctoral fellow working with Lanctôt.
There is great variability in each person’s brain anatomy—the thickness of the skull, the brain’s unique folds, the amount of cerebrospinal fluid. All of these structural differences impact how electrical or magnetic stimulation is distributed in the brain and ultimately the effects.
Using MRI or another brain scan along with computational modeling of the current flow, a clinician could create a treatment that is customized to each person’s brain, from where to put the electrodes to determining the exact dose and duration of stimulation needed to achieve lasting results, Sandrini says.
Above all, most neuroscientists say that largescale research studies over long periods of time are necessary to confirm the safety and durability of this therapy for the purpose of boosting memory. Short of that, there can be no FDA approval or medical regulation for this clinical use.
Lanctôt urges people to seek out clinical NIBS trials in their area if they want to see the science advance. “That is how we’ll find the answers,” she says, predicting it will be 5 to 10 years to develop each additional clinical application of NIBS. Ultimately, she predicts that reigning in Alzheimer’s disease and mild cognitive impairment will require a multi-pronged approach that includes lifestyle and medications, too.
Sandrini believes that scientific efforts should focus on preventing or delaying Alzheimer’s. “We need to start intervention earlier—as soon as people start to complain about forgetting things,” he says. “Changes in the brain start 10 years before [there is a problem]. Once Alzheimer’s develops, it is too late.”