A Team of Israeli Students Just Created Honey Without Bees

The bee-free honey on the left, and the Israeli team that won the iGEM competition.
Can you make honey without honeybees? According to 12 Israeli students who took home a gold medal in the iGEM (International Genetically Engineered Machine) competition with their synthetic honey project, the answer is yes, you can.
The honey industry faces serious environmental challenges, like the mysterious Colony Collapse Disorder.
For the past year, the team from Technion-Israel Institute of Technology has been working on creating sustainable, artificial honey—no bees required. Why? As the team explains in a video on the project's website, "Studies have shown the amazing nutritional values of honey. However, the honey industry harms the environment, and particularly the bees. That's why vegans don't use honey and why our honey will be a great replacement."
Indeed, honey has long been a controversial product in the vegan community. Some say it's stealing an animal's food source (though bees make more honey than they can possibly use). Some avoid eating honey because it is an animal product and bees' natural habitats are disturbed by humans harvesting it. Others feel that because bees aren't directly killed or harmed in the production of honey, it's not actually unethical to eat.
However, there's no doubt that the honey industry faces some serious environmental challenges. Colony Collapse Disorder, a mysterious phenomenon in which worker bees in colonies disappear in large numbers without any real explanation, came to international attention in 2006. Several explanations from poisonous pesticides to immune-suppressing stress to new or emerging diseases have been posited, but no definitive cause has been found.
There's also the problem of human-managed honey farms having a negative impact on the natural honeybee population.
So how can honey be made without honeybees? It's all about bacteria and enzymes.
The way bees make honey is by collecting nectar from flowers, transporting it in their "honey stomach" (which is separate from their food stomach), and bringing it back to the hive, where it gets transferred from bee mouth to bee mouth. That transferal process reduces the moisture content from about 70 percent to 20 percent, and honey is formed.
The product is still currently under development.
The Technion students created a model of a synthetic honey stomach metabolic pathway, in which the bacterium Bacillus subtilis "learns" to produce honey. "The bacteria can independently control the production of enzymes, eventually achieving a product with the same sugar profile as real honey, and the same health benefits," the team explains. Bacillus subtilis, which is found in soil, vegetation, and our own gastrointestinal tracts, has a natural ability to produce catalase, one of the enzymes needed for honey production. The product is still currently under development.
Whether this project results in a real-world jar of honey we'll be able to buy at the grocery store remains to be seen, but imagine how happy the bees—and vegans—would be if it did.
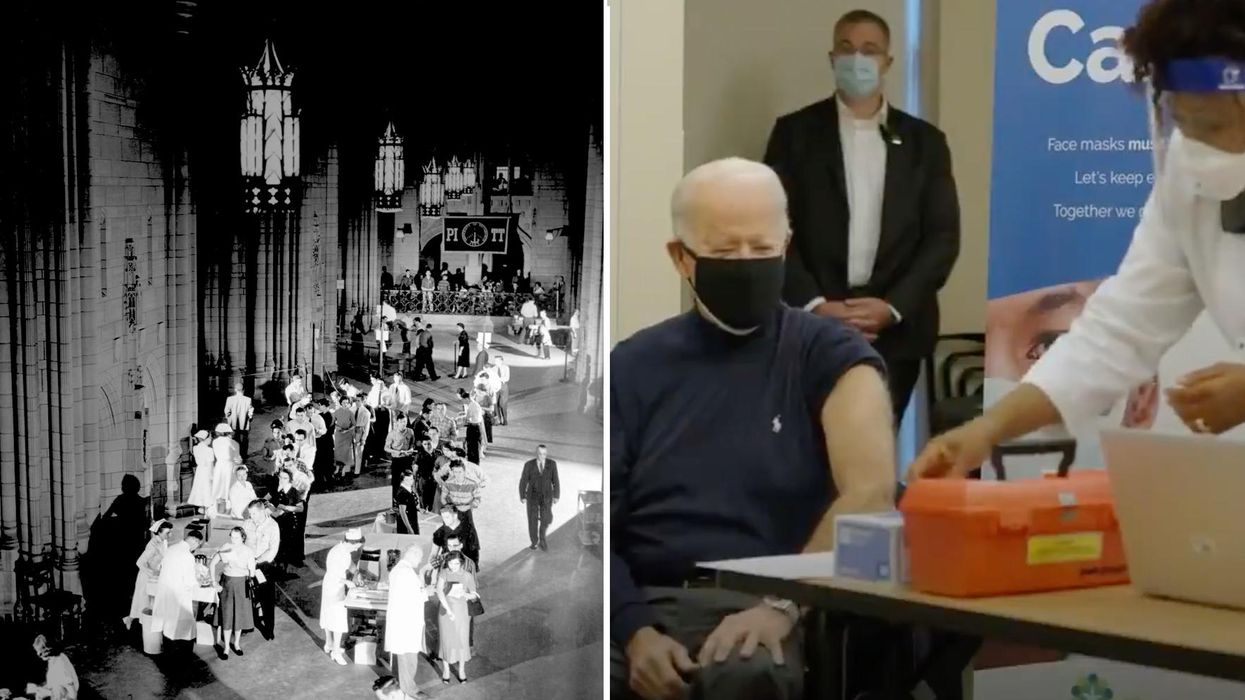
On left, people excitedly line up for Salk's polio vaccine in 1957; on right, Joe Biden gets one of the COVID vaccines on December 21, 2020.
On the morning of April 12, 1955, newsrooms across the United States inked headlines onto newsprint: the Salk Polio vaccine was "safe, effective, and potent." This was long-awaited news. Americans had limped through decades of fear, unaware of what caused polio or how to cure it, faced with the disease's terrifying, visible power to paralyze and kill, particularly children.
The announcement of the polio vaccine was celebrated with noisy jubilation: church bells rang, factory whistles sounded, people wept in the streets. Within weeks, mass inoculation began as the nation put its faith in a vaccine that would end polio.
Today, most of us are blissfully ignorant of child polio deaths, making it easier to believe that we have not personally benefited from the development of vaccines. According to Dr. Steven Pinker, cognitive psychologist and author of the bestselling book Enlightenment Now, we've become blasé to the gifts of science. "The default expectation is not that disease is part of life and science is a godsend, but that health is the default, and any disease is some outrage," he says.
We're now in the early stages of another vaccine rollout, one we hope will end the ravages of the COVID-19 pandemic. And yet, the Pfizer, Moderna, and AstraZeneca vaccines are met with far greater hesitancy and skepticism than the polio vaccine was in the 50s.
In 2021, concerns over the speed and safety of vaccine development and technology plague this heroic global effort, but the roots of vaccine hesitancy run far deeper. Vaccine hesitancy has always existed in the U.S., even in the polio era, motivated in part by fears around "living virus" in a bad batch of vaccines produced by Cutter Laboratories in 1955. But in the last half century, we've witnessed seismic cultural shifts—loss of public trust, a rise in misinformation, heightened racial and socioeconomic inequality, and political polarization have all intensified vaccine-related fears and resistance. Making sense of how we got here may help us understand how to move forward.
The Rise and Fall of Public Trust
When the polio vaccine was released in 1955, "we were nearing an all-time high point in public trust," says Matt Baum, Harvard Kennedy School professor and lead author of several reports measuring public trust and vaccine confidence. Baum explains that the U.S. was experiencing a post-war boom following the Allied triumph in WWII, a popular Roosevelt presidency, and the rapid innovation that elevated the country to an international superpower.
The 1950s witnessed the emergence of nuclear technology, a space program, and unprecedented medical breakthroughs, adds Emily Brunson, Texas State University anthropologist and co-chair of the Working Group on Readying Populations for COVID-19 Vaccine. "Antibiotics were a game changer," she states. While before, people got sick with pneumonia for a month, suddenly they had access to pills that accelerated recovery.
During this period, science seemed to hold all the answers; people embraced the idea that we could "come to know the world with an absolute truth," Brunson explains. Doctors were portrayed as unquestioned gods, so Americans were primed to trust experts who told them the polio vaccine was safe.
"The emotional tone of the news has gone downward since the 1940s, and journalists consider it a professional responsibility to cover the negative."
That blind acceptance eroded in the 1960s and 70s as people came to understand that science can be inherently political. "Getting to an absolute truth works out great for white men, but these things affect people socially in radically different ways," Brunson says. As the culture began questioning the white, patriarchal biases of science, doctors lost their god-like status and experts were pushed off their pedestals. This trend continues with greater intensity today, as President Trump has led a campaign against experts and waged a war on science that began long before the pandemic.
The Shift in How We Consume Information
In the 1950s, the media created an informational consensus. The fundamental ideas the public consumed about the state of the world were unified. "People argued about the best solutions, but didn't fundamentally disagree on the factual baseline," says Baum. Indeed, the messaging around the polio vaccine was centralized and consistent, led by President Roosevelt's successful March of Dimes crusade. People of lower socioeconomic status with limited access to this information were less likely to have confidence in the vaccine, but most people consumed media that assured them of the vaccine's safety and mobilized them to receive it.
Today, the information we consume is no longer centralized—in fact, just the opposite. "When you take that away, it's hard for people to know what to trust and what not to trust," Baum explains. We've witnessed an increase in polarization and the technology that makes it easier to give people what they want to hear, reinforcing the human tendencies to vilify the other side and reinforce our preexisting ideas. When information is engineered to further an agenda, each choice and risk calculation made while navigating the COVID-19 pandemic is deeply politicized.
This polarization maps onto a rise in socioeconomic inequality and economic uncertainty. These factors, associated with a sense of lost control, prime people to embrace misinformation, explains Baum, especially when the situation is difficult to comprehend. "The beauty of conspiratorial thinking is that it provides answers to all these questions," he says. Today's insidious fragmentation of news media accelerates the circulation of mis- and disinformation, reaching more people faster, regardless of veracity or motivation. In the case of vaccines, skepticism around their origin, safety, and motivation is intensified.
Alongside the rise in polarization, Pinker says "the emotional tone of the news has gone downward since the 1940s, and journalists consider it a professional responsibility to cover the negative." Relentless focus on everything that goes wrong further erodes public trust and paints a picture of the world getting worse. "Life saved is not a news story," says Pinker, but perhaps it should be, he continues. "If people were more aware of how much better life was generally, they might be more receptive to improvements that will continue to make life better. These improvements don't happen by themselves."
The Future Depends on Vaccine Confidence
So far, the U.S. has been unable to mitigate the catastrophic effects of the pandemic through social distancing, testing, and contact tracing. President Trump has downplayed the effects and threat of the virus, censored experts and scientists, given up on containing the spread, and mobilized his base to protest masks. The Trump Administration failed to devise a national plan, so our national plan has defaulted to hoping for the "miracle" of a vaccine. And they are "something of a miracle," Pinker says, describing vaccines as "the most benevolent invention in the history of our species." In record-breaking time, three vaccines have arrived. But their impact will be weakened unless we achieve mass vaccination. As Brunson notes, "The technology isn't the fix; it's people taking the technology."
Significant challenges remain, including facilitating widespread access and supporting on-the-ground efforts to allay concerns and build trust with specific populations with historic reasons for distrust, says Brunson. Baum predicts continuing delays as well as deaths from other causes that will be linked to the vaccine.
Still, there's every reason for hope. The new administration "has its eyes wide open to these challenges. These are the kind of problems that are amenable to policy solutions if we have the will," Baum says. He forecasts widespread vaccination by late summer and a bounce back from the economic damage, a "Good News Story" that will bolster vaccine acceptance in the future. And Pinker reminds us that science, medicine, and public health have greatly extended our lives in the last few decades, a trend that can only continue if we're willing to roll up our sleeves.
Scientists Are Working to Develop a Clever Nasal Spray That Tricks the Coronavirus Out of the Body
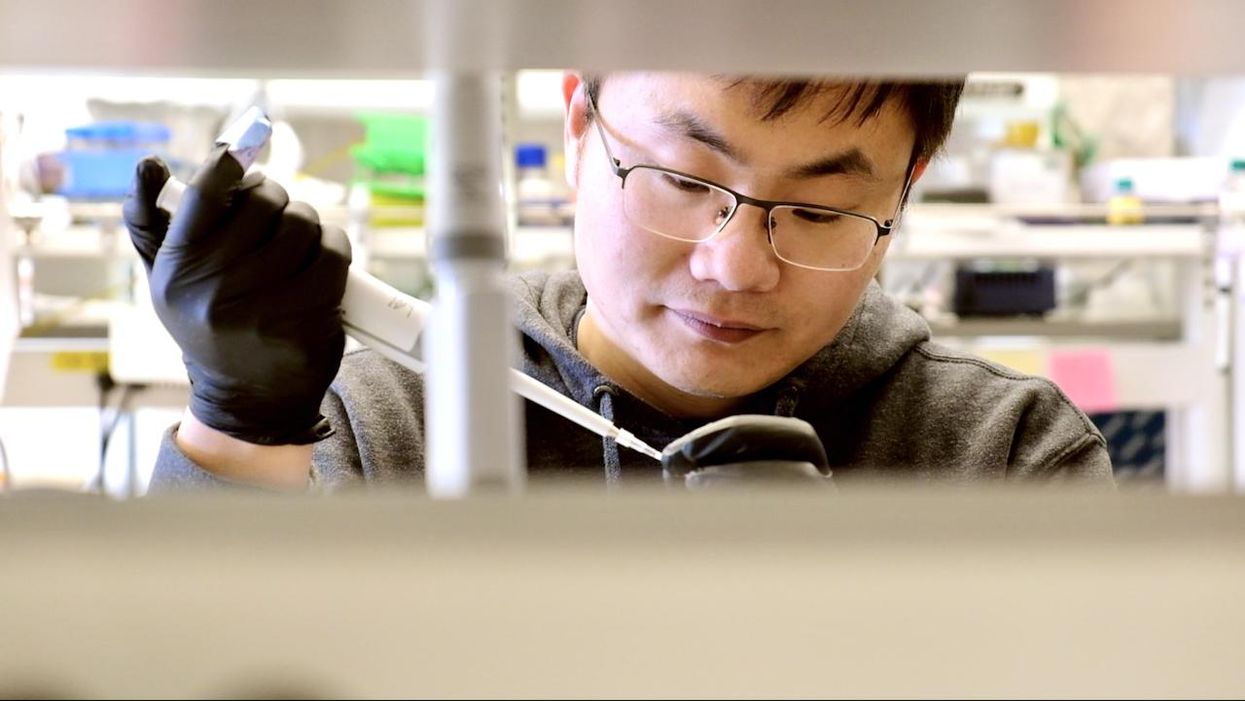
Biochemist Longxing Cao is working with colleagues at the University of Washington on promising research to disable infectious coronavirus in a person's nose.
Imagine this scenario: you get an annoying cough and a bit of a fever. When you wake up the next morning you lose your sense of taste and smell. That sounds familiar, so you head to a doctor's office for a Covid test, which comes back positive.
Your next step? An anti-Covid nasal spray of course, a "trickster drug" that will clear the once-dangerous and deadly virus out of the body. The drug works by tricking the coronavirus with decoy receptors that appear to be just like those on the surface of our own cells. The virus latches onto the drug's molecules "thinking" it is breaking into human cells, but instead it flushes out of your system before it can cause any serious damage.
This may sounds like science fiction, but several research groups are already working on such trickster coronavirus drugs, with some candidates close to clinical trials and possibly even becoming available late this year. The teams began working on them when the pandemic arrived, and continued in lockdown.
This may sounds like science fiction, but several research groups are already working on such trickster coronavirus drugs, with some candidates close to clinical trials and possibly even becoming available late this year. The teams began working on them when the pandemic arrived, and continued in lockdown.
When the pandemic first hit and the state of California issued a lockdown order on March 16, postdoctoral researchers Anum and Jeff Glasgow found themselves stuck at home with nothing to do. The two scientists who study bioengineering felt that they were well equipped to research molecular ways of disabling coronavirus's cell-penetrating spike protein, but they could no longer come to their labs at the University of California San Francisco.
"We were upset that no one put us in the game," says Anum Glasgow. "We have a lot of experience between us doing these types of projects so we wanted to contribute." But they still had computers so they began modeling the potential virus-disabling proteins in silico using Robetta, special software for designing and modeling protein structures, developed and maintained by University of Washington biochemist David Baker and his lab.
"We saw some imperfections in that lock and key and we created something better. We made a 10 times tighter adhesive."
The SARS-CoV-2 virus that causes Covid-19 uses its surface spike protein to bind on to a specific receptor on human cells called ACE2. Unfortunately for humans, the spike protein's molecular shape fits the ACE2 receptor like a well-cut key, making it very successful at breaking into our cells. But if one could design a molecular ACE2-mimic to "trick" the virus into latching onto it instead, the virus would no longer be able to enter cells. Scientists call such mimics receptor traps or inhibitors, or blockers. "It would block the adhesive part of the virus that binds to human cells," explains Jim Wells, professor of pharmaceutical chemistry at UCSF, whose lab took part in designing the ACE2-receptor mimic, working with the Glasgows and other colleagues.
The idea of disabling infectious or inflammatory agents by tricking them into binding to the targets' molecular look-alikes is something scientists have tried with other diseases. The anti-inflammatory drugs commonly used to treat autoimmune conditions, including rheumatoid arthritis, Crohn's disease and ulcerative colitis, rely on conceptually similar molecular mechanisms. Called TNF blockers, these drugs block the activity of the inflammatory cytokines, molecules that promote inflammation. "One of the biggest selling drugs in the world is a receptor trap," says Jeff Glasgow. "It acts as a receptor decoy. There's a TNF receptor that traps the cytokine."
In the recent past, scientists also pondered a similar look-alike approach to treating urinary tract infections, which are often caused by a pathogenic strain of Escherichia coli. An E. coli bacterium resembles a squid with protruding filaments equipped with proteins that can change their shape to form hooks, used to hang onto specific sugar molecules called ligands, which are present on the surface of the epithelial cells lining the urinary tract.
A recent study found that a sugar-like compound that's structurally similar to that ligand can play a similar trick on the E. Coli. When administered in in sufficient amounts, the compound hooks the bacteria on, which is then excreted out of the body with urine. The "trickster" method had been also tried against the HIV virus, but it wasn't very effective because HIV has a high mutation rate and multiple ways of entering human cells.
But the coronavirus spike protein's shape is more stable. And while it has a strong affinity for the ACE2 receptors, its natural binding to these receptors isn't perfect, which allowed the UCSF researchers to design a mimic with a better grip. "We saw some imperfections in that lock and key and we created something better," says Wells. "We made a 10 times tighter adhesive." The team demonstrated that their traps neutralized SARS-CoV-2 in lab experiments and published their study in the Proceedings of the National Academy of Sciences.
Baker, who is the director of the Institute for Protein Design at the University of Washington, was also devising ACE2 look-alikes with his team. Only unlike the UCSF team, they didn't perfect the virus-receptor lock and key combo, but instead designed their mimics from scratch. Using Robetta, they digitally modeled over two million proteins, zeroed-in on over 100,000 potential candidates and identified a handful with a strong promise of blocking SARS-CoV-2, testing them against the virus in human cells. Their design of the miniprotein inhibitors was published in the journal Science.

Biochemist David Baker, pictured in his lab at the University of Washington.
UW
The concept of the ACE2 receptor mimics is somewhat similar to the antibody plasma, but better, the teams explain. Antibodies don't always coat all of the virus's spike proteins and sometimes don't bind perfectly. By contrast, the ACE2 mimics directly compete with the virus's entry mechanism. ACE2 mimics are also easier and cheaper to make, researchers say.
Antibodies, which are long protein chains, must be grown inside mammalian cells, which is a slow and costly process. As drugs, antibody cocktails must be kept refrigerated. On the contrary, proteins that mimic ACE2 receptors are smaller and can be produced by bacteria easily and inexpensively. Designed to specs, these proteins don't need refrigeration and are easy to store. "We designed them to be very stable," says Baker. "Our computation design tries to come up with the stable proteins that have the desired functions."
That stability may allow the team to create an inhaler drug rather than an intravenous one, which would be another advantage over the antibody plasma, given via an IV. The team envisions people spraying the miniprotein solution into their nose, creating a protecting coating that would disable the inhaled virus. "The infection starts from your respiratory system, from your nose," explains Longxing Cao, the study's co-author—so a nasal spray would be a natural way to administer it. "So that you can have it like a layer, similar to a mask."
As the virus evolves, new variants are arising. But the teams think that their ACE2 protein mimics should work on the new variants too for several reasons. "Since the new SARS-CoV-2 variants still use ACE2 for their cell entry, they will likely still be susceptible to ACE2-based traps," Glasgow says.
Cao explains that their approach should work too because most of the mutations happen outside the ACE2 binding region. Plus, they are building multiple binders that can bind to an array of the coronavirus variants. "Our binder can still bind with most of the variants and we are trying to make one protein that could inhibit all the future escape variants," he says.
Baker and Cao hope that their miniproteins may be available to patients later this year. But besides getting the medicine out to patients, this approach will allow researchers to test the computer-modeled mimics end-to-end with an unprecedented speed. That would give humans a leg up in future pandemics or zoonotic disease outbreaks, which remain an increasingly pressing threat due to human activity and climate change.
"That's what we are focused on right now—understanding what we have learned from this pandemic to improve our design methods," says Baker. "So that we should be able to obtain binders like these very quickly when a new pandemic threat is identified."
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.