Abortions Before Fetal Viability Are Legal: Might Science and the Change on the Supreme Court Undermine That?

The United States Supreme Court Building in Washington, D.C.
This article is part of the magazine, "The Future of Science In America: The Election Issue," co-published by LeapsMag, the Aspen Institute Science & Society Program, and GOOD.
Viability—the potential for a fetus to survive outside the womb—is a core dividing line in American law. For almost 50 years, the Supreme Court of the United States has struck down laws that ban all or most abortions, ruling that women's constitutional rights include choosing to end pregnancies before the point of viability. Once viability is reached, however, states have a "compelling interest" in protecting fetal life. At that point, states can choose to ban or significantly restrict later-term abortions provided states allow an exception to preserve the life or health of the mother.
This distinction between a fetus that could survive outside its mother's body, albeit with significant medical intervention, and one that could not, is at the heart of the court's landmark 1973 decision in Roe v. Wade. The framework of viability remains central to the country's abortion law today, even as some states have passed laws in the name of protecting women's health that significantly undermine Roe. Over the last 30 years, the Supreme Court has upheld these laws, which have the effect of restricting pre-viability abortion access, imposing mandatory waiting periods, requiring parental consent for minors, and placing restrictions on abortion providers.
Viability has always been a slippery notion on which to pin legal rights.
Today, the Guttmacher Institute reports that more than half of American women live in states whose laws are considered hostile to abortion, largely as a result of these intrusions on pre-viability abortion access. Nevertheless, the viability framework stands: while states can pass pre-viability abortion restrictions that (ostensibly) protect the health of the woman or that strike some kind a balance between women's rights and fetal life, it is only after viability that they can completely favor fetal life over the rights of the woman (with limited exceptions when the woman's life is threatened). As a result, judges have struck down certain states' so-called heartbeat laws, which tried to prohibit abortions after detection of a fetal heartbeat (as early as six weeks of pregnancy). Bans on abortion after 12 or 15 weeks' gestation have also been reversed.
Now, with a new Supreme Court Justice expected to be hostile to abortion rights, advances in the care of preterm babies and ongoing research on artificial wombs suggest that the point of viability is already sooner than many assume and could soon be moved radically earlier in gestation, potentially providing a legal basis for earlier and earlier abortion bans.
Viability has always been a slippery notion on which to pin legal rights. It represents an inherently variable and medically shifting moment in the pregnancy timeline that the Roe majority opinion declined to firmly define, noting instead that "[v]iability is usually placed at about seven months (28 weeks) but may occur earlier, even at 24 weeks." Even in 1977, this definition was an optimistic generalization. Every baby is different, and while some 28-week infants born the year Roe was decided did indeed live into adulthood, most died at or shortly after birth. The prognosis for infants born at 24 weeks was much worse.
Today, a baby born at 28 weeks' gestation can be expected to do much better, largely due to the development of surfactant treatment in the early 1990s to help ease the air into babies' lungs. Now, the majority of 24-week-old babies can survive, and several very premature babies, born just shy of 22 weeks' gestation, have lived into childhood. All this variability raises the question: Should the law take a very optimistic, if largely unrealistic, approach to defining viability and place it at 22 weeks, even though the overall survival rate for those preemies remains less than 10% today? Or should the law recognize that keeping a premature infant alive requires specialist care, meaning that actual viability differs not just pregnancy-to-pregnancy but also by healthcare facility and from country to country? A 24-week premature infant born in a rural area or in a developing nation may not be viable as a practical matter, while one born in a major U.S. city with access to state-of-the-art care has a greater than 70% chance of survival. Just as some extremely premature newborns survive, some full-term babies die before, during, or soon after birth, regardless of whether they have access to advanced medical care.
To be accurate, viability should be understood as pregnancy-specific and should take into account the healthcare resources available to that woman. But state laws can't capture this degree of variability by including gestation limits in their abortion laws. Instead, many draw a somewhat arbitrary line at 22, 24, or 28 weeks' gestation, regardless of the particulars of the pregnancy or the medical resources available in that state.
As variable and resource-dependent as viability is today, science may soon move that point even earlier. Ectogenesis is a term coined in 1923 for the growth of an organism outside the body. Long considered science fiction, this technology has made several key advances in the past few years, with scientists announcing in 2017 that they had successfully gestated premature lamb fetuses in an artificial womb for four weeks. Currently in development for use in human fetuses between 22 and 23 weeks' gestation, this technology will almost certainly seek to push viability earlier in pregnancy.
Ectogenesis and other improvements in managing preterm birth deserve to be celebrated, offering new hope to the parents of very premature infants. But in the U.S., and in other nations whose abortion laws are fixed to viability, these same advances also pose a threat to abortion access. Abortion opponents have long sought to move the cutoff for legal abortions, and it is not hard to imagine a state prohibiting all abortions after 18 or 20 weeks by arguing that medical advances render this stage "the new viability," regardless of whether that level of advanced care is available to women in that state. If ectogenesis advances further, the limit could be moved to keep pace.
The Centers for Disease Control and Prevention reports that over 90% of abortions in America are performed at or before 13 weeks, meaning that in the short term, only a small number women would be affected by shifting viability standards. Yet these women are in difficult situations and deserve care and consideration. Research has shown that women seeking later terminations often did not recognize that they were pregnant or had their dates quite wrong, while others report that they had trouble accessing a termination earlier in pregnancy, were afraid to tell their partner or parents, or only recently received a diagnosis of health problems with the fetus.
Shifts in viability over the past few decades have already affected these women, many of whom report struggling to find a provider willing to perform a termination at 18 or 20 weeks out of concern that the woman may have her dates wrong. Ever-earlier gestational limits would continue this chilling effect, making doctors leery of terminating a pregnancy that might be within 2–4 weeks of each new ban. Some states' existing gestational limits on abortion are also inconsistent with prenatal care, which includes genetic testing between 12 and 20 weeks' gestation, as well as an anatomy scan to check the fetus's organ development performed at approximately 20 weeks. If viability moves earlier, prenatal care will be further undermined.
Perhaps most importantly, earlier and earlier abortion bans are inconsistent with the rights and freedoms on which abortion access is based, including recognition of each woman's individual right to bodily integrity and decision-making authority over her own medical care. Those rights and freedoms become meaningless if abortion bans encroach into the weeks that women need to recognize they are pregnant, assess their options, seek medical advice, and access appropriate care. Fetal viability, with its shifting goalposts, isn't the best framework for abortion protection in light of advancing medical science.
Ideally, whether to have an abortion would be a decision that women make in consultation with their doctors, free of state interference. The vast majority of women already make this decision early in pregnancy; the few who come to the decision later do so because something has gone seriously wrong in their lives or with their pregnancies. If states insist on drawing lines based on historical measures of viability, at 24 or 26 or 28 weeks, they should stick with those gestational limits and admit that they no longer represent actual viability but correspond instead to some form of common morality about when the fetus has a protected, if not absolute, right to life. Women need a reasonable amount of time to make careful and informed decisions about whether to continue their pregnancies precisely because these decisions have a lasting impact on their bodies and their lives. To preserve that time, legislators and the courts should decouple abortion rights from ectogenesis and other advances in the care of extremely premature infants that move the point of viability ever earlier.
[Editor's Note: This article was updated after publication to reflect Amy Coney Barrett's confirmation. To read other articles in this special magazine issue, visit the e-reader version.]
How to Measure Your Stress, with Dr. Rosalind Picard
Today’s podcast guest is Rosalind Picard, a researcher, inventor named on over 100 patents, entrepreneur, author, professor and engineer. When it comes to the science related to endowing computer software with emotional intelligence, she wrote the book. It’s published by MIT Press and called Affective Computing.
Dr. Picard is founder and director of the MIT Media Lab’s Affective Computing Research Group. Her research and engineering contributions have been recognized internationally. For example, she received the 2022 International Lombardy Prize for Computer Science Research, considered by many to be the Nobel prize in computer science.
Through her research and companies, Dr. Picard has developed wearable sensors, algorithms and systems for sensing, recognizing and responding to information about human emotion. Her products are focused on using fitness trackers to advance clinical quality treatments for a range of conditions.
Meanwhile, in just the past few years, numerous fitness tracking companies have released products with their own stress sensors and systems. You may have heard about Fitbit’s Stress Management Score, or Whoop’s Stress Monitor – these features and apps measure things like your heart rhythm and a certain type of invisible sweat to identify stress. They’re designed to raise awareness about forms of stress such as anxieties and anger, and suggest strategies like meditation to relax in real time when stress occurs.
But how well do these off-the-shelf gadgets work? There’s no one more knowledgeable and experienced than Rosalind Picard to explain the science behind these stress features, what they do exactly, how they might be able to help us, and their current shortcomings.
Dr. Picard is a member of the National Academy of Engineering and a Fellow of the National Academy of Inventors, and a popular speaker who’s given over a hundred invited keynote talks and a TED talk with over 2 million views. She holds a Bachelors in Electrical Engineering from Georgia Tech, and Masters and Doctorate degrees in Electrical Engineering and Computer Science from MIT. She lives in Newton, Massachusetts with her husband, where they’ve raised three sons.
In our conversation, we discuss stress scores on fitness trackers to improve well-being. She describes the difference between commercial products that might help people become more mindful of their health and products that are FDA approved and really capable of advancing the science. We also talk about several fascinating findings and concepts discovered in Dr. Picard’s lab including the multiple arousal theory, a phenomenon you’ll want to hear about. And we explore the complexity of stress, one reason it’s so tough to measure. For example, many forms of stress are actually good for us. Can fitness trackers tell the difference between stress that’s healthy and unhealthy?
Show links:
- Dr. Picard’s book, Affective Computing
- Dr. Picard’s bio
- Dr. Picard on Twitter
- Dr. Picard’s company, Empatica - https://www.empatica.com/ - The FDA-cleared Empatica Health Monitoring Platform provides accurate, continuous health insights for researchers and clinicians, collected in the real world
- Empatica Twitter
- Dr. Picard and her team have published hundreds of peer-reviewed articles across AI, Machine Learning, Affective Computing, Digital Health, and Human-computer interaction.
- Dr. Picard’s TED talk

Rosalind Picard
Dr. May Edward Chinn, Kizzmekia Corbett, PhD., and Alice Ball, among others, have been behind some of the most important scientific work of the last century.
If you look back on the last century of scientific achievements, you might notice that most of the scientists we celebrate are overwhelmingly white, while scientists of color take a backseat. Since the Nobel Prize was introduced in 1901, for example, no black scientists have landed this prestigious award.
The work of black women scientists has gone unrecognized in particular. Their work uncredited and often stolen, black women have nevertheless contributed to some of the most important advancements of the last 100 years, from the polio vaccine to GPS.
Here are five black women who have changed science forever.
Dr. May Edward Chinn
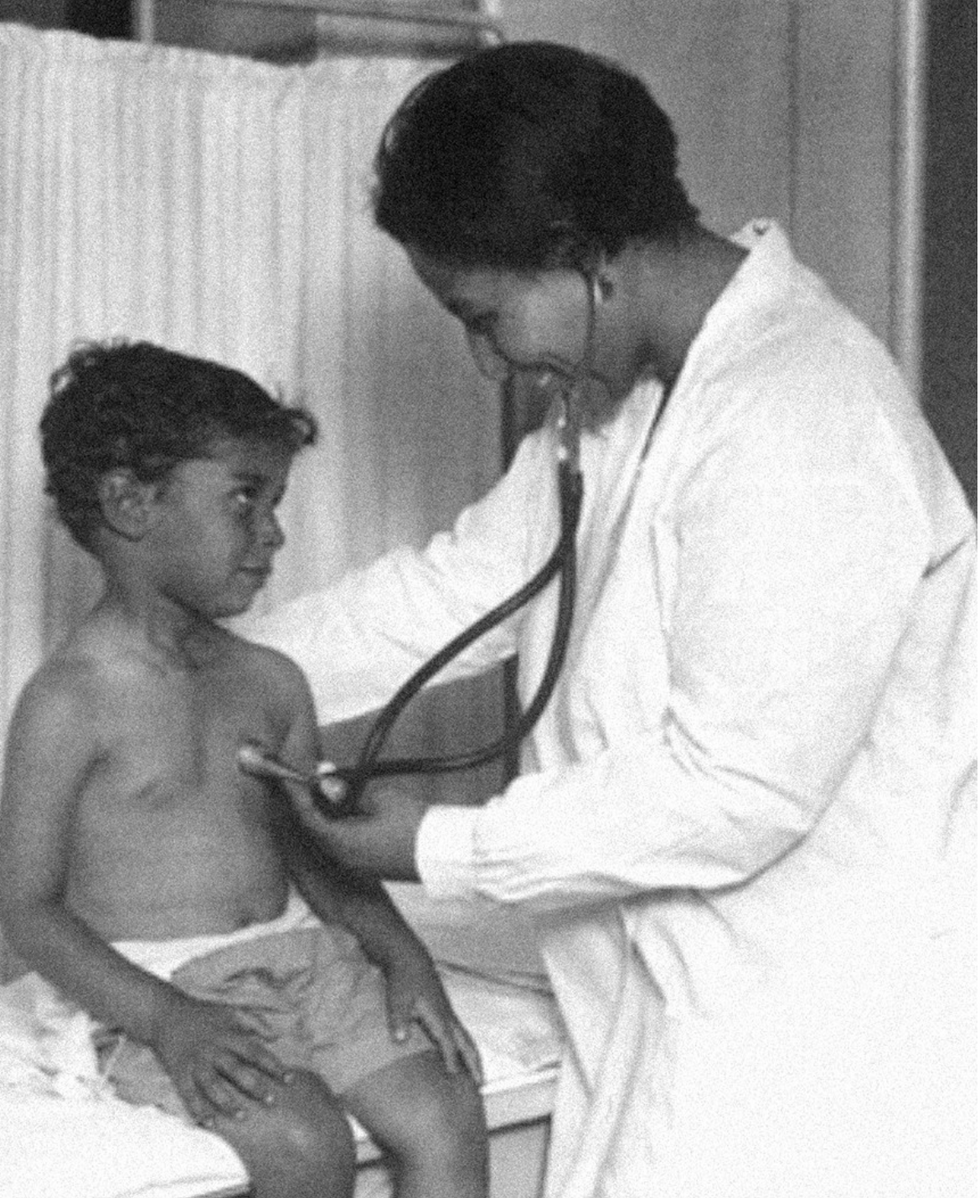
Dr. May Edward Chinn practicing medicine in Harlem
George B. Davis, PhD.
Chinn was born to poor parents in New York City just before the start of the 20th century. Although she showed great promise as a pianist, playing with the legendary musician Paul Robeson throughout the 1920s, she decided to study medicine instead. Chinn, like other black doctors of the time, were barred from studying or practicing in New York hospitals. So Chinn formed a private practice and made house calls, sometimes operating in patients’ living rooms, using an ironing board as a makeshift operating table.
Chinn worked among the city’s poor, and in doing this, started to notice her patients had late-stage cancers that often had gone undetected or untreated for years. To learn more about cancer and its prevention, Chinn begged information off white doctors who were willing to share with her, and even accompanied her patients to other clinic appointments in the city, claiming to be the family physician. Chinn took this information and integrated it into her own practice, creating guidelines for early cancer detection that were revolutionary at the time—for instance, checking patient health histories, checking family histories, performing routine pap smears, and screening patients for cancer even before they showed symptoms. For years, Chinn was the only black female doctor working in Harlem, and she continued to work closely with the poor and advocate for early cancer screenings until she retired at age 81.
Alice Ball

Pictorial Press Ltd/Alamy
Alice Ball was a chemist best known for her groundbreaking work on the development of the “Ball Method,” the first successful treatment for those suffering from leprosy during the early 20th century.
In 1916, while she was an undergraduate student at the University of Hawaii, Ball studied the effects of Chaulmoogra oil in treating leprosy. This oil was a well-established therapy in Asian countries, but it had such a foul taste and led to such unpleasant side effects that many patients refused to take it.
So Ball developed a method to isolate and extract the active compounds from Chaulmoogra oil to create an injectable medicine. This marked a significant breakthrough in leprosy treatment and became the standard of care for several decades afterward.
Unfortunately, Ball died before she could publish her results, and credit for this discovery was given to another scientist. One of her colleagues, however, was able to properly credit her in a publication in 1922.
Henrietta Lacks

onathan Newton/The Washington Post/Getty
The person who arguably contributed the most to scientific research in the last century, surprisingly, wasn’t even a scientist. Henrietta Lacks was a tobacco farmer and mother of five children who lived in Maryland during the 1940s. In 1951, Lacks visited Johns Hopkins Hospital where doctors found a cancerous tumor on her cervix. Before treating the tumor, the doctor who examined Lacks clipped two small samples of tissue from Lacks’ cervix without her knowledge or consent—something unthinkable today thanks to informed consent practices, but commonplace back then.
As Lacks underwent treatment for her cancer, her tissue samples made their way to the desk of George Otto Gey, a cancer researcher at Johns Hopkins. He noticed that unlike the other cell cultures that came into his lab, Lacks’ cells grew and multiplied instead of dying out. Lacks’ cells were “immortal,” meaning that because of a genetic defect, they were able to reproduce indefinitely as long as certain conditions were kept stable inside the lab.
Gey started shipping Lacks’ cells to other researchers across the globe, and scientists were thrilled to have an unlimited amount of sturdy human cells with which to experiment. Long after Lacks died of cervical cancer in 1951, her cells continued to multiply and scientists continued to use them to develop cancer treatments, to learn more about HIV/AIDS, to pioneer fertility treatments like in vitro fertilization, and to develop the polio vaccine. To this day, Lacks’ cells have saved an estimated 10 million lives, and her family is beginning to get the compensation and recognition that Henrietta deserved.
Dr. Gladys West

Andre West
Gladys West was a mathematician who helped invent something nearly everyone uses today. West started her career in the 1950s at the Naval Surface Warfare Center Dahlgren Division in Virginia, and took data from satellites to create a mathematical model of the Earth’s shape and gravitational field. This important work would lay the groundwork for the technology that would later become the Global Positioning System, or GPS. West’s work was not widely recognized until she was honored by the US Air Force in 2018.
Dr. Kizzmekia "Kizzy" Corbett

TIME Magazine
At just 35 years old, immunologist Kizzmekia “Kizzy” Corbett has already made history. A viral immunologist by training, Corbett studied coronaviruses at the National Institutes of Health (NIH) and researched possible vaccines for coronaviruses such as SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome).
At the start of the COVID pandemic, Corbett and her team at the NIH partnered with pharmaceutical giant Moderna to develop an mRNA-based vaccine against the virus. Corbett’s previous work with mRNA and coronaviruses was vital in developing the vaccine, which became one of the first to be authorized for emergency use in the United States. The vaccine, along with others, is responsible for saving an estimated 14 million lives.
