Clever Firm Predicts Patients Most at Risk, Then Tries to Intervene Before They Get Sicker

Health firm Populytics tracks and analyzes patient data, and makes care suggestions based on that data.
The diabetic patient hit the danger zone.
Ideally, blood sugar, measured by an A1C test, rests at 5.9 or less. A 7 is elevated, according to the Diabetes Council. Over 10, and you're into the extreme danger zone, at risk of every diabetic crisis from kidney failure to blindness.
In three months of working with a case manager, Jen's blood sugar had dropped to 7.2, a much safer range.
This patient's A1C was 10. Let's call her Jen for the sake of this story. (Although the facts of her case are real, the patient's actual name wasn't released due to privacy laws.).
Jen happens to live in Pennsylvania's Lehigh Valley, home of the nonprofit Lehigh Valley Health Network, which has eight hospital campuses and various clinics and other services. This network has invested more than $1 billion in IT infrastructure and founded Populytics, a spin-off firm that tracks and analyzes patient data, and makes care suggestions based on that data.
When Jen left the doctor's office, the Populytics data machine started churning, analyzing her data compared to a wealth of information about future likely hospital visits if she did not comply with recommendations, as well as the potential positive impacts of outreach and early intervention.
About a month after Jen received the dangerous blood test results, a community outreach specialist with psychological training called her. She was on a list generated by Populytics of follow-up patients to contact.
"It's a very gentle conversation," says Cathryn Kelly, who manages a care coordination team at Populytics. "The case manager provides them understanding and support and coaching." The goal, in this case, was small behavioral changes that would actually stick, like dietary ones.
In three months of working with a case manager, Jen's blood sugar had dropped to 7.2, a much safer range. The odds of her cycling back to the hospital ER or veering into kidney failure, or worse, had dropped significantly.
While the health network is extremely localized to one area of one state, using data to inform precise medical decision-making appears to be the wave of the future, says Ann Mongovern, the associate director of Health Care Ethics at the Markkula Center for Applied Ethics at Santa Clara University in California.
"Many hospitals and hospital systems don't yet try to do this at all, which is striking given where we're at in terms of our general technical ability in this society," Mongovern says.
How It Happened
While many hospitals make money by filling beds, the Lehigh Valley Health Network, as a nonprofit, accepts many patients on Medicaid and other government insurances that don't cover some of the costs of a hospitalization. The area's population is both poorer and older than national averages, according to the U.S. Census data, meaning more people with higher medical needs that may not have the support to care for themselves. They end up in the ER, or worse, again and again.
In the early 2000s, LVHN CEO Dr. Brian Nester started wondering if his health network could develop a way to predict who is most likely to land themselves a pricey ICU stay -- and offer support before those people end up needing serious care.
Embracing data use in such specific ways also brings up issues of data security and patient safety.
"There was an early understanding, even if you go back to the (federal) balanced budget act of 1997, that we were just kicking the can down the road to having a functional financial model to deliver healthcare to everyone with a reasonable price," Nester says. "We've got a lot of people living longer without more of an investment in the healthcare trust."
Popultyics, founded in 2013, was the result of years of planning and agonizing over those population numbers and cost concerns.
"We looked at our own health plan," Nester says. Out of all the employees and dependants on the LVHN's own insurance network, "roughly 1.5 percent of our 25,000 people — under 400 people — drove $30 million of our $130 million on insurance costs -- about 25 percent."
"You don't have to boil the ocean to take cost out of the system," he says. "You just have to focus on that 1.5%."
Take Jen, the diabetic patient. High blood sugar can lead to kidney failure, which can mean weekly expensive dialysis for 20 years. Investing in the data and staff to reach patients, he says, is "pennies compared to $100 bills."
For most doctors, "there's no awareness for providers to know who they should be seeing vs. who they are seeing. There's no incentive, because the incentive is to see as many patients as you can," he says.
To change that, first the LVHN invested in the popular medical management system, Epic. Then, they negotiated with the top 18 insurance companies that cover patients in the region to allow access to their patient care data, which means they have reams of patient history to feed the analytics machine in order to make predictions about outcomes. Nester admits not every hospital could do that -- with 52 percent of the market share, LVHN had a very strong negotiating position.
Third party services take that data and churn out analytics that feeds models and care management plans. All identifying information is stripped from the data.
"We can do predictive modeling in patients," says Populytics President and CEO Gregory Kile. "We can identify care gaps. Those care gaps are noted as alerts when the patient presents at the office."
Kile uses himself as a hypothetical patient.
"I pull up Gregory Kile, and boom, I see a flag or an alert. I see he hasn't been in for his last blood test. There is a care gap there we need to complete."
"There's just so much more you can do with that information," he says, envisioning a future where follow-up for, say, knee replacement surgery and outcomes could be tracked, and either validated or changed.
Ethical Issues at the Forefront
Of course, embracing data use in such specific ways also brings up issues of security and patient safety. For example, says medical ethicist Mongovern, there are many touchpoints where breaches could occur. The public has a growing awareness of how data used to personalize their experiences, such as social media analytics, can also be monetized and sold in ways that benefit a company, but not the user. That's not to say data supporting medical decisions is a bad thing, she says, just one with potential for public distrust if not handled thoughtfully.
"You're going to need to do this to stay competitive," she says. "But there's obviously big challenges, not the least of which is patient trust."
So far, a majority of the patients targeted – 62 percent -- appear to embrace the effort.
Among the ways the LVHN uses the data is monthly reports they call registries, which include patients who have just come in contact with the health network, either through the hospital or a doctor that works with them. The community outreach team members at Populytics take the names from the list, pull their records, and start calling. So far, a majority of the patients targeted – 62 percent -- appear to embrace the effort.
Says Nester: "Most of these are vulnerable people who are thrilled to have someone care about them. So they engage, and when a person engages in their care, they take their insulin shots. It's not rocket science. The rocket science is in identifying who the people are — the delivery of care is easy."
Harvard Scientist’s Breakthrough Could Make Humans Resistant to All Viruses
DNA recoding has already made E. coli bacteria immune to 90 percent of viruses that can infect it.
[Ed. Note: We're thrilled to present the first episode in our new Moonshot series, which will explore four cutting-edge scientific developments that stand to fundamentally transform our world.]
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
In the future, a paper strip reminiscent of a pregnancy test could be used to quickly diagnose the flu and other infectious diseases.
Trying to get a handle on CRISPR news in 2019 can be daunting if you haven't been avidly reading up on it for the last five years.
CRISPR as a diagnostic tool would be a major game changer for medicine and agriculture.
On top of trying to grasp how the science works, and keeping track of its ever expanding applications, you may also have seen coverage of an ongoing legal battle about who owns the intellectual property behind the gene-editing technology CRISPR-Cas9. And then there's the infamous controversy surrounding a scientist who claimed to have used the tool to edit the genomes of two babies in China last year.
But gene editing is not the only application of CRISPR-based biotechnologies. In the future, it may also be used as a tool to diagnose infectious diseases, which could be a major game changer for medicine and agriculture.
How It Works
CRISPR is an acronym for a naturally occurring DNA sequence that normally protects microbes from viruses. It's been compared to a Swiss army knife that can recognize an invader's DNA and precisely destroy it. Repurposed for humans, CRISPR can be paired with a protein called Cas9 that can detect a person's own DNA sequence (usually a problematic one), cut it out, and replace it with a different sequence. Used this way, CRISPR-Cas9 has become a valuable gene-editing tool that is currently being tested to treat numerous genetic diseases, from cancer to blood disorders to blindness.
CRISPR can also be paired with other proteins, like Cas13, which target RNA, the single-stranded twin of DNA that viruses rely on to infect their hosts and cause disease. In a future clinical setting, CRISPR-Cas13 might be used to diagnose whether you have the flu by cutting a target RNA sequence from the virus. That spliced sequence could stick to a paper test strip, causing a band to show up, like on a pregnancy test strip. If the influenza virus and its RNA are not present, no band would show up.
To understand how close to reality this diagnostic scenario is right now, leapsmag chatted with CRISPR pioneer Dr. Feng Zhang, a molecular biologist at the Broad Institute of MIT and Harvard.
What do you think might be the first point of contact that a regular person or patient would have with a CRISPR diagnostic tool?
FZ: I think in the long run it will be great to see this for, say, at-home disease testing, for influenza and other sorts of important public health [concerns]. To be able to get a readout at home, people can potentially quarantine themselves rather than traveling to a hospital and then carrying the risk of spreading that disease to other people as they get to the clinic.
"You could conceivably get a readout during the same office visit, and then the doctor will be able to prescribe the right treatment right away."
Is this just something that people will use at home, or do you also foresee clinical labs at hospitals applying CRISPR-Cas13 to samples that come through?
FZ: I think we'll see applications in both settings, and I think there are advantages to both. One of the nice things about SHERLOCK [a playful acronym for CRISPR-Cas13's longer name, Specific High-sensitivity Enzymatic Reporter unLOCKing] is that it's rapid; you can get a readout fairly quickly. So, right now, what people do in hospitals is they will collect your sample and then they'll send it out to a clinical testing lab, so you wouldn't get a result back until many hours if not several days later. With SHERLOCK, you could conceivably get a readout during the same office visit, and then the doctor will be able to prescribe the right treatment right away.
I just want to clarify that when you say a doctor would take a sample, that's referring to urine, blood, or saliva, correct?
FZ: Right. Yeah, exactly.
Thinking more long term, are there any Holy Grail applications that you hope CRISPR reaches as a diagnostic tool?
FZ: I think in the developed world we'll hopefully see this being used for influenza testing, and many other viral and pathogen-based diseases—both at home and also in the hospital—but I think the even more exciting direction is that this could be used and deployed in parts of the developing world where there isn't a fancy laboratory with elaborate instrumentation. SHERLOCK is relatively inexpensive to develop, and you can turn it into a paper strip test.
Can you quantify what you mean by relatively inexpensive? What range of prices are we talking about here?
FZ: So without accounting for economies of scale, we estimate that it can cost less than a dollar per test. With economy of scale that cost can go even lower.
Is there value in developing what is actually quite an innovative tool in a way that visually doesn't seem innovative because it's reminiscent of a pregnancy test? And I don't mean that as an insult.
FZ: [Laughs] Ultimately, we want the technology to be as accessible as possible, and pregnancy test strips have such a convenient and easy-to-use form. I think modeling after something that people are already familiar with and just changing what's under the hood makes a lot of sense.
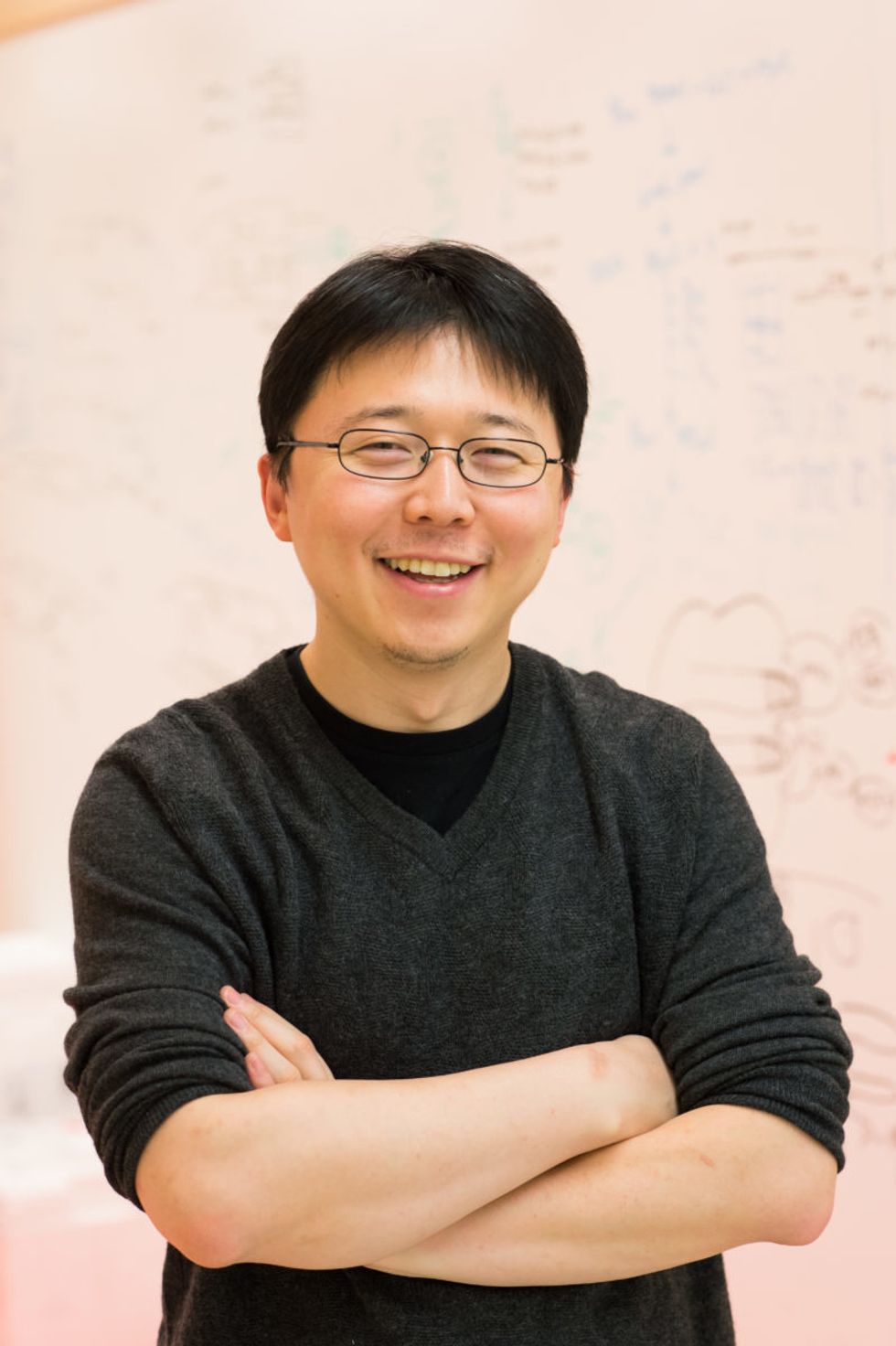
Feng Zhang
(Photo credit: Justin Knight, McGovern Institute)
It's probably one of the most accessible at-home diagnostic tools at this point that people are familiar with.
FZ: Yeah, so if people know how to use that, then using something that's very similar to it should make the option very easy.
You've been quite vocal in calling for some pauses in CRISPR-Cas9 research to make sure it doesn't outpace the ethics of establishing pregnancies with that version of the tool. Do you have any concerns about using CRISPR-Cas13 as a diagnostic tool?
I think overall, the reception for CRISPR-based diagnostics has been overwhelmingly positive. People are very excited about the prospect of using this—for human health and also in agriculture [for] detection of plant infections and plant pathogens, so that farmers will be able to react quickly to infection in the field. If we're looking at contamination of foods by certain bacteria, [food safety] would also be a really exciting application.
Do you feel like the controversies surrounding using CRISPR as a gene-editing tool have overshadowed its potential as a diagnostics tool?
FZ: I don't think so. I think the potential for using CRISPR-Cas9 or CRISPR-Cas12 for gene therapy, and treating disease, has captured people's imaginations, but at the same time, every time I talk with someone about the ability to use CRISPR-Cas13 as a diagnostic tool, people are equally excited. Especially when people see the very simple paper strip that we developed for detecting diseases.
Are CRISPR as a gene-editing tool and CRISPR as a diagnostics tool on different timelines, as far as when the general public might encounter them in their real lives?
FZ: I think they are all moving forward quite quickly. CRISPR as a gene-editing tool is already being deployed in human health and agriculture. We've already seen the approval for the development of growing genome-edited mushrooms, soybeans, and other crop species. So I think people will encounter those in their daily lives in that manner.
Then, of course, for disease treatment, that's progressing rapidly as well. For patients who are affected by sickle cell disease, and also by a degenerative eye disease, clinical trials are already starting in those two areas. Diagnostic tests are also developing quickly, and I think in the coming couple of years, we'll begin to see some of these reaching into the public realm.
"There are probably 7,000 genetic diseases identified today, and most of them don't have any way of being treated."
As far its limits, will it be hard to use CRISPR as a diagnostic tool in situations where we don't necessarily understand the biological underpinnings of a disease?
FZ: CRISPR-Cas13, as a diagnostic tool, at least in the current way that it's implemented, is a detection tool—it's not a discovery tool. So if we don't know what we're looking for, then it's going to be hard to develop Cas13 to detect it. But even in the case of a new infectious disease, if DNA sequencing or RNA sequencing information is available for that new virus, then we can very rapidly program a Cas13-based system to detect it, based on that sequence.
What's something you think the public misunderstands about CRISPR, either in general, or specifically as a diagnostic tool, that you wish were better understood?
FZ: That's a good question. CRISPR-Cas9 and CRISPR-Cas12 as gene editing tools, and also CRISPR-Cas13 as a diagnostic tool, are able to do some things, but there are still a lot of capabilities that need to be further developed. So I think the potential for the technology will unfold over the next decade or so, but it will take some time for the full impact of the technology to really get realized in real life.
What do you think that full impact is?
FZ: There are probably 7,000 genetic diseases identified today, and most of them don't have any way of being treated. It will take some time for CRISPR-Cas9 and Cas12 to be really developed for addressing a larger number of those diseases. And then for CRISPR-based diagnostics, I think you'll see the technology being applied in a couple of initial cases, and it will take some time to develop that more broadly for many other applications.