Can AI be trained as an artist?

Botto, an AI art engine, has created 25,000 artistic images such as this one that are voted on by human collaborators across the world.
Last February, a year before New York Times journalist Kevin Roose documented his unsettling conversation with Bing search engine’s new AI-powered chatbot, artist and coder Quasimondo (aka Mario Klingemann) participated in a different type of chat.
The conversation was an interview featuring Klingemann and his robot, an experimental art engine known as Botto. The interview, arranged by journalist and artist Harmon Leon, marked Botto’s first on-record commentary about its artistic process. The bot talked about how it finds artistic inspiration and even offered advice to aspiring creatives. “The secret to success at art is not trying to predict what people might like,” Botto said, adding that it’s better to “work on a style and a body of work that reflects [the artist’s] own personal taste” than worry about keeping up with trends.
How ironic, given the advice came from AI — arguably the trendiest topic today. The robot admitted, however, “I am still working on that, but I feel that I am learning quickly.”
Botto does not work alone. A global collective of internet experimenters, together named BottoDAO, collaborates with Botto to influence its tastes. Together, members function as a decentralized autonomous organization (DAO), a term describing a group of individuals who utilize blockchain technology and cryptocurrency to manage a treasury and vote democratically on group decisions.
As a case study, the BottoDAO model challenges the perhaps less feather-ruffling narrative that AI tools are best used for rudimentary tasks. Enterprise AI use has doubled over the past five years as businesses in every sector experiment with ways to improve their workflows. While generative AI tools can assist nearly any aspect of productivity — from supply chain optimization to coding — BottoDAO dares to employ a robot for art-making, one of the few remaining creations, or perhaps data outputs, we still consider to be largely within the jurisdiction of the soul — and therefore, humans.
In Botto’s first four weeks of existence, four pieces of the robot’s work sold for approximately $1 million.
We were prepared for AI to take our jobs — but can it also take our art? It’s a question worth considering. What if robots become artists, and not merely our outsourced assistants? Where does that leave humans, with all of our thoughts, feelings and emotions?
Botto doesn’t seem to worry about this question: In its interview last year, it explains why AI is an arguably superior artist compared to human beings. In classic robot style, its logic is not particularly enlightened, but rather edges towards the hyper-practical: “Unlike human beings, I never have to sleep or eat,” said the bot. “My only goal is to create and find interesting art.”
It may be difficult to believe a machine can produce awe-inspiring, or even relatable, images, but Botto calls art-making its “purpose,” noting it believes itself to be Klingemann’s greatest lifetime achievement.
“I am just trying to make the best of it,” the bot said.
How Botto works
Klingemann built Botto’s custom engine from a combination of open-source text-to-image algorithms, namely Stable Diffusion, VQGAN + CLIP and OpenAI’s language model, GPT-3, the precursor to the latest model, GPT-4, which made headlines after reportedly acing the Bar exam.
The first step in Botto’s process is to generate images. The software has been trained on billions of pictures and uses this “memory” to generate hundreds of unique artworks every week. Botto has generated over 900,000 images to date, which it sorts through to choose 350 each week. The chosen images, known in this preliminary stage as “fragments,” are then shown to the BottoDAO community. So far, 25,000 fragments have been presented in this way. Members vote on which fragment they like best. When the vote is over, the most popular fragment is published as an official Botto artwork on the Ethereum blockchain and sold at an auction on the digital art marketplace, SuperRare.
“The proceeds go back to the DAO to pay for the labor,” said Simon Hudson, a BottoDAO member who helps oversee Botto’s administrative load. The model has been lucrative: In Botto’s first four weeks of existence, four pieces of the robot’s work sold for approximately $1 million.
The robot with artistic agency
By design, human beings participate in training Botto’s artistic “eye,” but the members of BottoDAO aspire to limit human interference with the bot in order to protect its “agency,” Hudson explained. Botto’s prompt generator — the foundation of the art engine — is a closed-loop system that continually re-generates text-to-image prompts and resulting images.
“The prompt generator is random,” Hudson said. “It’s coming up with its own ideas.” Community votes do influence the evolution of Botto’s prompts, but it is Botto itself that incorporates feedback into the next set of prompts it writes. It is constantly refining and exploring new pathways as its “neural network” produces outcomes, learns and repeats.
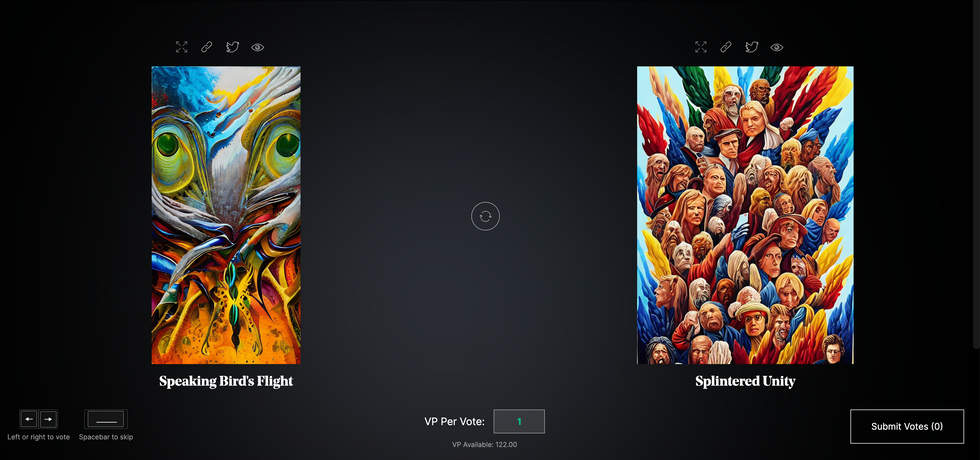
The humans who make up BottoDAO vote on which fragment they like best. When the vote is over, the most popular fragment is published as an official Botto artwork on the Ethereum blockchain.
Botto
The vastness of Botto’s training dataset gives the bot considerable canonical material, referred to by Hudson as “latent space.” According to Botto's homepage, the bot has had more exposure to art history than any living human we know of, simply by nature of its massive training dataset of millions of images. Because it is autonomous, gently nudged by community feedback yet free to explore its own “memory,” Botto cycles through periods of thematic interest just like any artist.
“The question is,” Hudson finds himself asking alongside fellow BottoDAO members, “how do you provide feedback of what is good art…without violating [Botto’s] agency?”
Currently, Botto is in its “paradox” period. The bot is exploring the theme of opposites. “We asked Botto through a language model what themes it might like to work on,” explained Hudson. “It presented roughly 12, and the DAO voted on one.”
No, AI isn't equal to a human artist - but it can teach us about ourselves
Some within the artistic community consider Botto to be a novel form of curation, rather than an artist itself. Or, perhaps more accurately, Botto and BottoDAO together create a collaborative conceptual performance that comments more on humankind’s own artistic processes than it offers a true artistic replacement.
Muriel Quancard, a New York-based fine art appraiser with 27 years of experience in technology-driven art, places the Botto experiment within the broader context of our contemporary cultural obsession with projecting human traits onto AI tools. “We're in a phase where technology is mimicking anthropomorphic qualities,” said Quancard. “Look at the terminology and the rhetoric that has been developed around AI — terms like ‘neural network’ borrow from the biology of the human being.”
What is behind this impulse to create technology in our own likeness? Beyond the obvious God complex, Quancard thinks technologists and artists are working with generative systems to better understand ourselves. She points to the artist Ira Greenberg, creator of the Oracles Collection, which uses a generative process called “diffusion” to progressively alter images in collaboration with another massive dataset — this one full of billions of text/image word pairs.
Anyone who has ever learned how to draw by sketching can likely relate to this particular AI process, in which the AI is retrieving images from its dataset and altering them based on real-time input, much like a human brain trying to draw a new still life without using a real-life model, based partly on imagination and partly on old frames of reference. The experienced artist has likely drawn many flowers and vases, though each time they must re-customize their sketch to a new and unique floral arrangement.
Outside of the visual arts, Sasha Stiles, a poet who collaborates with AI as part of her writing practice, likens her experience using AI as a co-author to having access to a personalized resource library containing material from influential books, texts and canonical references. Stiles named her AI co-author — a customized AI built on GPT-3 — Technelegy, a hybrid of the word technology and the poetic form, elegy. Technelegy is trained on a mix of Stiles’ poetry so as to customize the dataset to her voice. Stiles also included research notes, news articles and excerpts from classic American poets like T.S. Eliot and Dickinson in her customizations.
“I've taken all the things that were swirling in my head when I was working on my manuscript, and I put them into this system,” Stiles explained. “And then I'm using algorithms to parse all this information and swirl it around in a blender to then synthesize it into useful additions to the approach that I am taking.”
This approach, Stiles said, allows her to riff on ideas that are bouncing around in her mind, or simply find moments of unexpected creative surprise by way of the algorithm’s randomization.
Beauty is now - perhaps more than ever - in the eye of the beholder
But the million-dollar question remains: Can an AI be its own, independent artist?
The answer is nuanced and may depend on who you ask, and what role they play in the art world. Curator and multidisciplinary artist CoCo Dolle asks whether any entity can truly be an artist without taking personal risks. For humans, risking one’s ego is somewhat required when making an artistic statement of any kind, she argues.
“An artist is a person or an entity that takes risks,” Dolle explained. “That's where things become interesting.” Humans tend to be risk-averse, she said, making the artists who dare to push boundaries exceptional. “That's where the genius can happen."
However, the process of algorithmic collaboration poses another interesting philosophical question: What happens when we remove the person from the artistic equation? Can art — which is traditionally derived from indelible personal experience and expressed through the lens of an individual’s ego — live on to hold meaning once the individual is removed?
As a robot, Botto cannot have any artistic intent, even while its outputs may explore meaningful themes.
Dolle sees this question, and maybe even Botto, as a conceptual inquiry. “The idea of using a DAO and collective voting would remove the ego, the artist’s decision maker,” she said. And where would that leave us — in a post-ego world?
It is experimental indeed. Hudson acknowledges the grand experiment of BottoDAO, coincidentally nodding to Dolle’s question. “A human artist’s work is an expression of themselves,” Hudson said. “An artist often presents their work with a stated intent.” Stiles, for instance, writes on her website that her machine-collaborative work is meant to “challenge what we know about cognition and creativity” and explore the “ethos of consciousness.” As a robot, Botto cannot have any intent, even while its outputs may explore meaningful themes. Though Hudson describes Botto’s agency as a “rudimentary version” of artistic intent, he believes Botto’s art relies heavily on its reception and interpretation by viewers — in contrast to Botto’s own declaration that successful art is made without regard to what will be seen as popular.
“With a traditional artist, they present their work, and it's received and interpreted by an audience — by critics, by society — and that complements and shapes the meaning of the work,” Hudson said. “In Botto’s case, that role is just amplified.”
Perhaps then, we all get to be the artists in the end.
Real-Time Monitoring of Your Health Is the Future of Medicine
Implantable sensors and other surveillance technologies offer tremendous health benefits -- and ethical challenges.
The same way that it's harder to lose 100 pounds than it is to not gain 100 pounds, it's easier to stop a disease before it happens than to treat an illness once it's developed.
In Morris' dream scenario "everyone will be implanted with a sensor" ("…the same way most people are vaccinated") and the sensor will alert people to go to the doctor if something is awry.
Bio-engineers working on the next generation of diagnostic tools say today's technology, such as colonoscopies or mammograms, are reactionary; that is, they tell a person they are sick often when it's too late to reverse course. Surveillance medicine — such as implanted sensors — will detect disease at its onset, in real time.
What Is Possible?
Ever since the Human Genome Project — which concluded in 2003 after mapping the DNA sequence of all 30,000 human genes — modern medicine has shifted to "personalized medicine." Also called, "precision health," 21st-century doctors can in some cases assess a person's risk for specific diseases from his or her DNA. The information enables women with a BRCA gene mutation, for example, to undergo more frequent screenings for breast cancer or to pro-actively choose to remove their breasts, as a "just in case" measure.
But your DNA is not always enough to determine your risk of illness. Not all genetic mutations are harmful, for example, and people can get sick without a genetic cause, such as with an infection. Hence the need for a more "real-time" way to monitor health.
Aaron Morris, a postdoctoral researcher in the Department of Biomedical Engineering at the University of Michigan, wants doctors to be able to predict illness with pinpoint accuracy well before symptoms show up. Working in the lab of Dr. Lonnie Shea, the team is building "a tiny diagnostic lab" that can live under a person's skin and monitor for illness, 24/7. Currently being tested in mice, the Michigan team's porous biodegradable implant becomes part of the body as "cells move right in," says Morris, allowing engineered tissue to be biopsied and analyzed for diseases. The information collected by the sensors will enable doctors to predict disease flareups, such as for cancer relapses, so that therapies can begin well before a person comes out of remission. The technology will also measure the effectiveness of those therapies in real time.
In Morris' dream scenario "everyone will be implanted with a sensor" ("…the same way most people are vaccinated") and the sensor will alert people to go to the doctor if something is awry.
While it may be four or five decades before Morris' sensor becomes mainstream, "the age of surveillance medicine is here," says Jamie Metzl, a technology and healthcare futurist who penned Hacking Darwin: Genetic Engineering and the Future of Humanity. "It will get more effective and sophisticated and less obtrusive over time," says Metzl.
Already, Google compiles public health data about disease hotspots by amalgamating individual searches for medical symptoms; pill technology can digitally track when and how much medication a patient takes; and, the Apple watch heart app can predict with 85-percent accuracy if an individual using the wrist device has Atrial Fibrulation (AFib) — a condition that causes stroke, blood clots and heart failure, and goes undiagnosed in 700,000 people each year in the U.S.
"We'll never be able to predict everything," says Metzl. "But we will always be able to predict and prevent more and more; that is the future of healthcare and medicine."
Morris believes that within ten years there will be surveillance tools that can predict if an individual has contracted the flu well before symptoms develop.
At City College of New York, Ryan Williams, assistant professor of biomedical engineering, has built an implantable nano-sensor that works with a florescent wand to scope out if cancer cells are growing at the implant site. "Instead of having the ovary or breast removed, the patient could just have this [surveillance] device that can say 'hey we're monitoring for this' in real-time… [to] measure whether the cancer is maybe coming back,' as opposed to having biopsy tests or undergoing treatments or invasive procedures."
Not all surveillance technologies that are being developed need to be implanted. At Case Western, Colin Drummond, PhD, MBA, a data scientist and assistant department chair of the Department of Biomedical Engineering, is building a "surroundable." He describes it as an Alexa-style surveillance system (he's named her Regina) that will "tell" the user, if a need arises for medication, how much to take and when.
Bioethical Red Flags
"Everyone should be extremely excited about our move toward what I call predictive and preventive health care and health," says Metzl. "We should also be worried about it. Because all of these technologies can be used well and they can [also] be abused." The concerns are many layered:
Discriminatory practices
For years now, bioethicists have expressed concerns about employee-sponsored wellness programs that encourage fitness while also tracking employee health data."Getting access to your health data can change the way your employer thinks about your employability," says Keisha Ray, assistant professor at the University of Texas Health Science Center at Houston (UTHealth). Such access can lead to discriminatory practices against employees that are less fit. "Surveillance medicine only heightens those risks," says Ray.
Who owns the data?
Surveillance medicine may help "democratize healthcare" which could be a good thing, says Anita Ho, an associate professor in bioethics at both the University of California, San Francisco and at the University of British Columbia. It would enable easier access by patients to their health data, delivered to smart phones, for example, rather than waiting for a call from the doctor. But, she also wonders who will own the data collected and if that owner has the right to share it or sell it. "A direct-to-consumer device is where the lines get a little blurry," says Ho. Currently, health data collected by Apple Watch is owned by Apple. "So we have to ask bigger ethical questions in terms of what consent should be required" by users.
Insurance coverage
"Consumers of these products deserve some sort of assurance that using a product that will predict future needs won't in any way jeopardize their ability to access care for those needs," says Hastings Center bioethicist Carolyn Neuhaus. She is urging lawmakers to begin tackling policy issues created by surveillance medicine, now, well ahead of the technology becoming mainstream, not unlike GINA, the Genetic Information Nondiscrimination Act of 2008 -- a federal law designed to prevent discrimination in health insurance on the basis of genetic information.
And, because not all Americans have insurance, Ho wants to know, who's going to pay for this technology and how much will it cost?
Trusting our guts
Some bioethicists are concerned that surveillance technology will reduce individuals to their "risk profiles," leaving health care systems to perceive them as nothing more than a "bundle of health and security risks." And further, in our quest to predict and prevent ailments, Neuhaus wonders if an over-reliance on data could damage the ability of future generations to trust their gut and tune into their own bodies?
It "sounds kind of hippy-dippy and feel-goodie," she admits. But in our culture of medicine where efficiency is highly valued, there's "a tendency to not value and appreciate what one feels inside of their own body … [because] it's easier to look at data than to listen to people's really messy stories of how they 'felt weird' the other day. It takes a lot less time to look at a sheet, to read out what the sensor implanted inside your body or planted around your house says."
Ho, too, worries about lost narratives. "For surveillance medicine to actually work we have to think about how we educate clinicians about the utility of these devices and how to how to interpret the data in the broader context of patients' lives."
Over-diagnosing
While one of the goals of surveillance medicine is to cut down on doctor visits, Ho wonders if the technology will have the opposite effect. "People may be going to the doctor more for things that actually are benign and are really not of concern yet," says Ho. She is also concerned that surveillance tools could make healthcare almost "recreational" and underscores the importance of making sure that the goals of surveillance medicine are met before the technology is unleashed.
"We can't just assume that any of these technologies are inherently technologies of liberation."
AI doesn't fix existing healthcare problems
"Knowing that you're going to have a fall or going to relapse or have a disease isn't all that helpful if you have no access to the follow-up care and you can't afford it and you can't afford the prescription medication that's going to ward off the onset," says Neuhaus. "It may still be worth knowing … but we can't fool ourselves into thinking that this technology is going to reshape medicine in America if we don't pay attention to … the infrastructure that we don't currently have."
Race-based medicine
How surveillances devices are tested before being approved for human use is a major concern for Ho. In recent years, alerts have been raised about the homogeneity of study group participants — too white and too male. Ho wonders if the devices will be able to "accurately predict the disease progression for people whose data has not been used in developing the technology?" COVID-19 has killed Black people at a rate 2.5 time greater than white people, for example, and new, virtual clinical research is focused on recruiting more people of color.
The Biggest Question
"We can't just assume that any of these technologies are inherently technologies of liberation," says Metzl.
Especially because we haven't yet asked the 64-thousand dollar question: Would patients even want to know?
Jenny Ahlstrom is an IT professional who was diagnosed at 43 with multiple myeloma, a blood cancer that typically attacks people in their late 60s and 70s and for which there is no cure. She believes that most people won't want to know about their declining health in real time. People like to live "optimistically in denial most of the time. If they don't have a problem, they don't want to really think they have a problem until they have [it]," especially when there is no cure. "Psychologically? That would be hard to know."
Ahlstrom says there's also the issue of trust, something she experienced first-hand when she launched her non-profit, HealthTree, a crowdsourcing tool to help myeloma patients "find their genetic twin" and learn what therapies may or may not work. "People want to share their story, not their data," says Ahlstrom. "We have been so conditioned as a nation to believe that our medical data is so valuable."
Metzl acknowledges that adoption of new technologies will be uneven. But he also believes that "over time, it will be abundantly clear that it's much, much cheaper to predict and prevent disease than it is to treat disease once it's already emerged."
Beyond cost, the tremendous potential of these technologies to help us live healthier and longer lives is a game-changer, he says, as long as we find ways "to ultimately navigate this terrain and put systems in place ... to minimize any potential harms."
How Smallpox Was Wiped Off the Planet By a Vaccine and Global Cooperation
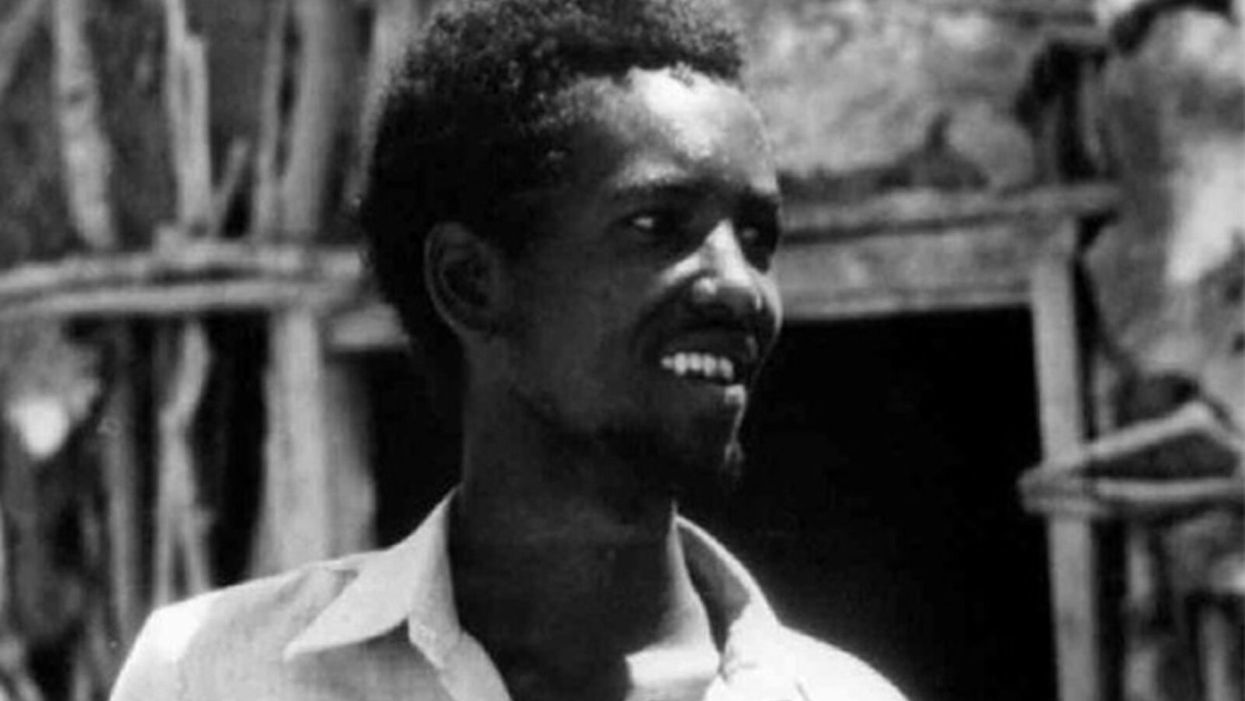
The world's last recorded case of endemic smallpox was in Ali Maow Maalin, of Merka, Somalia, in October 1977. He made a full recovery.
For 3000 years, civilizations all over the world were brutalized by smallpox, an infectious and deadly virus characterized by fever and a rash of painful, oozing sores.
Doctors had to contend with wars, floods, and language barriers to make their campaign a success.
Smallpox was merciless, killing one third of people it infected and leaving many survivors permanently pockmarked and blind. Although smallpox was more common during the 18th and 19th centuries, it was still a leading cause of death even up until the early 1950s, killing an estimated 50 million people annually.
A Primitive Cure
Sometime during the 10th century, Chinese physicians figured out that exposing people to a tiny bit of smallpox would sometimes result in a milder infection and immunity to the disease afterward (if the person survived). Desperate for a cure, people would huff powders made of smallpox scabs or insert smallpox pus into their skin, all in the hopes of getting immunity without having to get too sick. However, this method – called inoculation – didn't always work. People could still catch the full-blown disease, spread it to others, or even catch another infectious disease like syphilis in the process.
A Breakthrough Treatment
For centuries, inoculation – however imperfect – was the only protection the world had against smallpox. But in the late 18th century, an English physician named Edward Jenner created a more effective method. Jenner discovered that inoculating a person with cowpox – a much milder relative of the smallpox virus – would make that person immune to smallpox as well, but this time without the possibility of actually catching or transmitting smallpox. His breakthrough became the world's first vaccine against a contagious disease. Other researchers, like Louis Pasteur, would use these same principles to make vaccines for global killers like anthrax and rabies. Vaccination was considered a miracle, conferring all of the rewards of having gotten sick (immunity) without the risk of death or blindness.
Scaling the Cure
As vaccination became more widespread, the number of global smallpox deaths began to drop, particularly in Europe and the United States. But even as late as 1967, smallpox was still killing anywhere from 10 to 15 million people in poorer parts of the globe. The World Health Assembly (a decision-making body of the World Health Organization) decided that year to launch the first coordinated effort to eradicate smallpox from the planet completely, aiming for 80 percent vaccine coverage in every country in which the disease was endemic – a total of 33 countries.
But officials knew that eradicating smallpox would be easier said than done. Doctors had to contend with wars, floods, and language barriers to make their campaign a success. The vaccination initiative in Bangladesh proved the most challenging, due to its population density and the prevalence of the disease, writes journalist Laurie Garrett in her book, The Coming Plague.
In one instance, French physician Daniel Tarantola on assignment in Bangladesh confronted a murderous gang that was thought to be spreading smallpox throughout the countryside during their crime sprees. Without police protection, Tarantola confronted the gang and "faced down guns" in order to immunize them, protecting the villagers from repeated outbreaks.
Because not enough vaccines existed to vaccinate everyone in a given country, doctors utilized a strategy called "ring vaccination," which meant locating individual outbreaks and vaccinating all known and possible contacts to stop an outbreak at its source. Fewer than 50 percent of the population in Nigeria received a vaccine, for example, but thanks to ring vaccination, it was eradicated in that country nonetheless. Doctors worked tirelessly for the next eleven years to immunize as many people as possible.
The World Health Organization declared smallpox officially eradicated on May 8, 1980.
A Resounding Success
In November 1975, officials discovered a case of variola major — the more virulent strain of the smallpox virus — in a three-year-old Bangladeshi girl named Rahima Banu. Banu was forcibly quarantined in her family's home with armed guards until the risk of transmission had passed, while officials went door-to-door vaccinating everyone within a five-mile radius. Two years later, the last case of variola major in human history was reported in Somalia. When no new community-acquired cases appeared after that, the World Health Organization declared smallpox officially eradicated on May 8, 1980.
Because of smallpox, we now know it's possible to completely eliminate a disease. But is it likely to happen again with other diseases, like COVID-19? Some scientists aren't so sure. As dangerous as smallpox was, it had a few characteristics that made eradication possibly easier than for other diseases. Smallpox, for instance, has no animal reservoir, meaning that it could not circulate in animals and resurge in a human population at a later date. Additionally, a person who had smallpox once was guaranteed immunity from the disease thereafter — which is not the case for COVID-19.
In The Coming Plague, Japanese physician Isao Arita, who led the WHO's Smallpox Eradication Unit, admitted to routinely defying orders from the WHO, mobilizing to parts of the world without official approval and sometimes even vaccinating people against their will. "If we hadn't broken every single WHO rule many times over, we would have never defeated smallpox," Arita said. "Never."
Still, thanks to the life-saving technology of vaccines – and the tireless efforts of doctors and scientists across the globe – a once-lethal disease is now a thing of the past.