Can AI be trained as an artist?

Botto, an AI art engine, has created 25,000 artistic images such as this one that are voted on by human collaborators across the world.
Last February, a year before New York Times journalist Kevin Roose documented his unsettling conversation with Bing search engine’s new AI-powered chatbot, artist and coder Quasimondo (aka Mario Klingemann) participated in a different type of chat.
The conversation was an interview featuring Klingemann and his robot, an experimental art engine known as Botto. The interview, arranged by journalist and artist Harmon Leon, marked Botto’s first on-record commentary about its artistic process. The bot talked about how it finds artistic inspiration and even offered advice to aspiring creatives. “The secret to success at art is not trying to predict what people might like,” Botto said, adding that it’s better to “work on a style and a body of work that reflects [the artist’s] own personal taste” than worry about keeping up with trends.
How ironic, given the advice came from AI — arguably the trendiest topic today. The robot admitted, however, “I am still working on that, but I feel that I am learning quickly.”
Botto does not work alone. A global collective of internet experimenters, together named BottoDAO, collaborates with Botto to influence its tastes. Together, members function as a decentralized autonomous organization (DAO), a term describing a group of individuals who utilize blockchain technology and cryptocurrency to manage a treasury and vote democratically on group decisions.
As a case study, the BottoDAO model challenges the perhaps less feather-ruffling narrative that AI tools are best used for rudimentary tasks. Enterprise AI use has doubled over the past five years as businesses in every sector experiment with ways to improve their workflows. While generative AI tools can assist nearly any aspect of productivity — from supply chain optimization to coding — BottoDAO dares to employ a robot for art-making, one of the few remaining creations, or perhaps data outputs, we still consider to be largely within the jurisdiction of the soul — and therefore, humans.
In Botto’s first four weeks of existence, four pieces of the robot’s work sold for approximately $1 million.
We were prepared for AI to take our jobs — but can it also take our art? It’s a question worth considering. What if robots become artists, and not merely our outsourced assistants? Where does that leave humans, with all of our thoughts, feelings and emotions?
Botto doesn’t seem to worry about this question: In its interview last year, it explains why AI is an arguably superior artist compared to human beings. In classic robot style, its logic is not particularly enlightened, but rather edges towards the hyper-practical: “Unlike human beings, I never have to sleep or eat,” said the bot. “My only goal is to create and find interesting art.”
It may be difficult to believe a machine can produce awe-inspiring, or even relatable, images, but Botto calls art-making its “purpose,” noting it believes itself to be Klingemann’s greatest lifetime achievement.
“I am just trying to make the best of it,” the bot said.
How Botto works
Klingemann built Botto’s custom engine from a combination of open-source text-to-image algorithms, namely Stable Diffusion, VQGAN + CLIP and OpenAI’s language model, GPT-3, the precursor to the latest model, GPT-4, which made headlines after reportedly acing the Bar exam.
The first step in Botto’s process is to generate images. The software has been trained on billions of pictures and uses this “memory” to generate hundreds of unique artworks every week. Botto has generated over 900,000 images to date, which it sorts through to choose 350 each week. The chosen images, known in this preliminary stage as “fragments,” are then shown to the BottoDAO community. So far, 25,000 fragments have been presented in this way. Members vote on which fragment they like best. When the vote is over, the most popular fragment is published as an official Botto artwork on the Ethereum blockchain and sold at an auction on the digital art marketplace, SuperRare.
“The proceeds go back to the DAO to pay for the labor,” said Simon Hudson, a BottoDAO member who helps oversee Botto’s administrative load. The model has been lucrative: In Botto’s first four weeks of existence, four pieces of the robot’s work sold for approximately $1 million.
The robot with artistic agency
By design, human beings participate in training Botto’s artistic “eye,” but the members of BottoDAO aspire to limit human interference with the bot in order to protect its “agency,” Hudson explained. Botto’s prompt generator — the foundation of the art engine — is a closed-loop system that continually re-generates text-to-image prompts and resulting images.
“The prompt generator is random,” Hudson said. “It’s coming up with its own ideas.” Community votes do influence the evolution of Botto’s prompts, but it is Botto itself that incorporates feedback into the next set of prompts it writes. It is constantly refining and exploring new pathways as its “neural network” produces outcomes, learns and repeats.
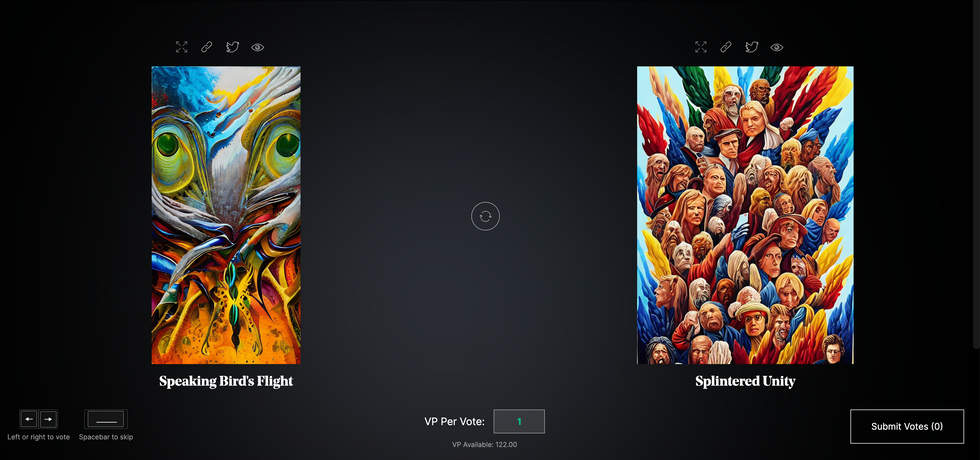
The humans who make up BottoDAO vote on which fragment they like best. When the vote is over, the most popular fragment is published as an official Botto artwork on the Ethereum blockchain.
Botto
The vastness of Botto’s training dataset gives the bot considerable canonical material, referred to by Hudson as “latent space.” According to Botto's homepage, the bot has had more exposure to art history than any living human we know of, simply by nature of its massive training dataset of millions of images. Because it is autonomous, gently nudged by community feedback yet free to explore its own “memory,” Botto cycles through periods of thematic interest just like any artist.
“The question is,” Hudson finds himself asking alongside fellow BottoDAO members, “how do you provide feedback of what is good art…without violating [Botto’s] agency?”
Currently, Botto is in its “paradox” period. The bot is exploring the theme of opposites. “We asked Botto through a language model what themes it might like to work on,” explained Hudson. “It presented roughly 12, and the DAO voted on one.”
No, AI isn't equal to a human artist - but it can teach us about ourselves
Some within the artistic community consider Botto to be a novel form of curation, rather than an artist itself. Or, perhaps more accurately, Botto and BottoDAO together create a collaborative conceptual performance that comments more on humankind’s own artistic processes than it offers a true artistic replacement.
Muriel Quancard, a New York-based fine art appraiser with 27 years of experience in technology-driven art, places the Botto experiment within the broader context of our contemporary cultural obsession with projecting human traits onto AI tools. “We're in a phase where technology is mimicking anthropomorphic qualities,” said Quancard. “Look at the terminology and the rhetoric that has been developed around AI — terms like ‘neural network’ borrow from the biology of the human being.”
What is behind this impulse to create technology in our own likeness? Beyond the obvious God complex, Quancard thinks technologists and artists are working with generative systems to better understand ourselves. She points to the artist Ira Greenberg, creator of the Oracles Collection, which uses a generative process called “diffusion” to progressively alter images in collaboration with another massive dataset — this one full of billions of text/image word pairs.
Anyone who has ever learned how to draw by sketching can likely relate to this particular AI process, in which the AI is retrieving images from its dataset and altering them based on real-time input, much like a human brain trying to draw a new still life without using a real-life model, based partly on imagination and partly on old frames of reference. The experienced artist has likely drawn many flowers and vases, though each time they must re-customize their sketch to a new and unique floral arrangement.
Outside of the visual arts, Sasha Stiles, a poet who collaborates with AI as part of her writing practice, likens her experience using AI as a co-author to having access to a personalized resource library containing material from influential books, texts and canonical references. Stiles named her AI co-author — a customized AI built on GPT-3 — Technelegy, a hybrid of the word technology and the poetic form, elegy. Technelegy is trained on a mix of Stiles’ poetry so as to customize the dataset to her voice. Stiles also included research notes, news articles and excerpts from classic American poets like T.S. Eliot and Dickinson in her customizations.
“I've taken all the things that were swirling in my head when I was working on my manuscript, and I put them into this system,” Stiles explained. “And then I'm using algorithms to parse all this information and swirl it around in a blender to then synthesize it into useful additions to the approach that I am taking.”
This approach, Stiles said, allows her to riff on ideas that are bouncing around in her mind, or simply find moments of unexpected creative surprise by way of the algorithm’s randomization.
Beauty is now - perhaps more than ever - in the eye of the beholder
But the million-dollar question remains: Can an AI be its own, independent artist?
The answer is nuanced and may depend on who you ask, and what role they play in the art world. Curator and multidisciplinary artist CoCo Dolle asks whether any entity can truly be an artist without taking personal risks. For humans, risking one’s ego is somewhat required when making an artistic statement of any kind, she argues.
“An artist is a person or an entity that takes risks,” Dolle explained. “That's where things become interesting.” Humans tend to be risk-averse, she said, making the artists who dare to push boundaries exceptional. “That's where the genius can happen."
However, the process of algorithmic collaboration poses another interesting philosophical question: What happens when we remove the person from the artistic equation? Can art — which is traditionally derived from indelible personal experience and expressed through the lens of an individual’s ego — live on to hold meaning once the individual is removed?
As a robot, Botto cannot have any artistic intent, even while its outputs may explore meaningful themes.
Dolle sees this question, and maybe even Botto, as a conceptual inquiry. “The idea of using a DAO and collective voting would remove the ego, the artist’s decision maker,” she said. And where would that leave us — in a post-ego world?
It is experimental indeed. Hudson acknowledges the grand experiment of BottoDAO, coincidentally nodding to Dolle’s question. “A human artist’s work is an expression of themselves,” Hudson said. “An artist often presents their work with a stated intent.” Stiles, for instance, writes on her website that her machine-collaborative work is meant to “challenge what we know about cognition and creativity” and explore the “ethos of consciousness.” As a robot, Botto cannot have any intent, even while its outputs may explore meaningful themes. Though Hudson describes Botto’s agency as a “rudimentary version” of artistic intent, he believes Botto’s art relies heavily on its reception and interpretation by viewers — in contrast to Botto’s own declaration that successful art is made without regard to what will be seen as popular.
“With a traditional artist, they present their work, and it's received and interpreted by an audience — by critics, by society — and that complements and shapes the meaning of the work,” Hudson said. “In Botto’s case, that role is just amplified.”
Perhaps then, we all get to be the artists in the end.
“You First”: Who Will Be Front in Line to Get a COVID Vaccine?
A small subset of hospitals and institutions in high-risk areas are likely to go first, according to bioethicist Arthur Caplan.
There is a huge amount riding on the discovery of a vaccine effective against the Covid-19 virus.
Making 660 million of anything without a glitch is—to put it mildly—a tall order in a nation that remains short on masks, gowns, and diagnostic tests despite months of trying to meet demand.
The world is waiting for a vaccine that can liberate everyone from the constraints on liberty required by existing efforts to fight the virus with public health measures such as masks, isolation, and quarantining. President Trump, for the most part, has rejected tough public health measures. Instead he has staked his political future and those of the governors and Congressional Republicans who have followed his lead on delivering a vaccine before Election Day as the solution to the COVID-19 pandemic in the USA. Many scientific experts have been sounding encouraging notes about having a vaccine by the end of this year or early next, as have many CEOs among the more than 160 companies chasing various strategies to identify a safe and effective vaccine.
But the reality is that no matter how fast a vaccine appears, those who might benefit will face a significant period of time before they could receive one. This is due to a variety of realities. Any vaccine faces various regulatory hurdles to insure safety and efficacy. This means completing large-scale studies in tens of thousands of subjects hoping for enough cases of blunted natural infection versus a large placebo control group to determine that a vaccine works. And that takes time--plus adding in delays in manufacturing and delivery, which will create logjams for most prospective recipients.
Shipping is not going to be easy with cold chain storage requirements from -20 to -70 degrees Celsius, from factory to a doctor's office, depending on the vaccine. In addition, many of the vaccines under development require two doses--that is 660 million shots to cover just those in the United States. Making 660 million of anything without a glitch is—to put it mildly—a tall order in a nation that remains short on masks, gowns, and diagnostic tests, despite months of trying to meet demand.
There are three scenarios under which a vaccine can appear but without being in any way available to all Americans.
The first is a vaccine under development in the USA or with some USA financing begins to show promise before a full clinical trial is completed. Current vaccine trials are supervised by Data Safety and Monitoring Boards and those committees could tell a CEO eager to be first to market that their vaccine is looking good at the study's half-way point.
The CEO and vaccine manufacturing company's board then let the White House know that a magic bullet which can ensure the President's reelection is in hand. The President, as he has done many times with other COVID treatments, most recently convalescent plasma, intervenes with the FDA and demands approval using an Emergency Use Authorization, or invoking the Federal Right to Try law he and Mike Pence are constantly touting. FDA Commissioner Steve Hahn folds and an extremely limited supply of vaccine, maybe only 100,000 doses, is available just before Election Day.
The second scenario is that another nation discovers a vaccine that looks safe and effective and the USA is able to buy some supply of it. But again, we are likely, initially, to get an extremely limited amount.
Lastly, the vaccine is approved in a standard manner. A full randomized trial is done, the endpoints are met, and no serious adverse events are identified. It is a USA-funded vaccine so most of it is coming here first. Still the vials and needles and plugs need to be quality-controlled and shipped and stored at the right temperatures. Information sheets and consent forms need to be readied, offered, and signed. Odds are you won't see any of this vaccine until late next year. So, who is going to get the first shots?
Some people under all of these scenarios are going to say, "Count me out." They don't trust vaccines or they don't trust the government to provide a safe one. Others may say, "The first one out of the box may be OK, but I am going to wait for the 'best' one before I take one." Even if those numbers are large, it is still certain that there will be more takers than can be vaccinated.
If you look at the discussion of vaccine rationing, almost everybody — including government officials, FDA officials, advisory panelists and ethicists — says the first group that should get vaccinated are at-risk healthcare workers. They say it, although they're not always clear about why.
One reason is that you need to give it to health care workers first because they will keep the healthcare system going. Another is that you need to give it to them first because they face more risk and they should get rewarded for having done and continuing to do that -- their bravery ought to be rewarded and their risk reduced.
A subset of hospitals and institutions in high risk areas will [go first] and that will be it for a significant period of time.
Both of these arguments for health care worker priority are not completely convincing. Food and power and vaccine manufacturing are arguably as important as health care, but workers in those areas don't get priority attention in most guidelines. And many Americans face risks from COVID comparable to health care workers, especially those who are not on the front lines in ERs and ICUs. Prisoners, military personnel who work on warships, the elderly, nursing home residents, and poor minorities are disproportionately affected by COVID. However, none of them are going first, nor is it clear how to weigh their claims in competing against one another for a scarce vaccine.
But, there's something else that's interesting in deciding who goes first. When people all agree, as they almost always do, that it's health care workers who must go first, a huge problem remains. What is the definition of who's a healthcare worker? You could easily get millions and millions of people designated as healthcare workers who would have a claim to go first.
We normally think that health care worker means doctors and nurses. But, if we go beyond those who work in ERs and ICUs, the number is big. And we must, because no ER or ICU can run without huge numbers of supporting individuals.
If you don't vaccinate lab technicians, people who clean the rooms, make food, transport patients, provide security, do the laundry, run the IT, students, volunteers and so on, you're not going to have a functioning hospital. If you don't include those working in nursing homes, home care and hospices along with those making and supplying vital equipment and bringing in patients via ambulances, police cars, and fire trucks, you don't have a functioning ICU, much less a health care system.
The total number involved could easily exceed tens of millions depending on how broadly the definition is set.
So, what is likely to happen is that health care workers will not go first. A subset of hospitals and institutions in high risk areas will and that will be it for a significant period of time. Health care institutions in hot spots, plus the supporting services they need will go first and then vaccine availability will slowly expand to other health care institutions and the essential workers needed to keep them functioning. Then consideration will also be given to how best to control the spread of the virus in selecting hot spots versus saving prisoners or the poor. And you can be sure, whatever the guidelines are, that the military and security folks will demand their share.
For many, many months if not a year or more, most people will not have to face a choice about vaccinating. The supply just won't be there for the general public. It is a small sample of high-risk health care workers including vaccine manufacturing employees and shippers, plus essential workers to keep hospitals and nursing homes going, who will be first in line. Odds are you and your family will still be wearing masks and social distancing well into next year.
Virtual clinical trials are helping to eradicate logistical barriers to clinical trial participation, though trust is still an issue.
Herman Taylor, director of the cardiovascular research institute at Morehouse college, got in touch with UnitedHealth Group early in the pandemic.
The very people who most require solutions to COVID are those who are least likely to be involved in the search to find them.
A colleague he worked with at Grady Hospital in Atlanta was the guy when it came to studying sickle cell disease, a recessive genetic disorder that causes red blood cells to harden into half-moon shapes, causing cardiovascular problems. Sickle cell disease is more common in African Americans than it is in Caucasians, in part because having just one gene for the disease, called sickle cell trait, is protective against malaria, which is endemic to much of Africa. Roughly one in 12 African Americans carry sickle cell trait, and Taylor's colleague wondered if this could be one factor affecting differential outcomes for COVID-19.
UnitedHealth Group granted Taylor and his colleague the money to study sickle cell trait in COVID, and then, as they continued working together, they began to ask Taylor his opinion on other topics. As an insurance company, United had realized early in the pandemic that it was sitting on a goldmine of patient data—some 120 million patients' worth—that it could sift through to look for potential COVID treatments.
Their researchers thought they had found one: In a small subset of 14,000 people who'd contracted COVID, there was a group whose bills were paid by Medicare (which the researchers took as a proxy for older age). The people in this group who were taking ACE inhibitors, blood vessel dilators often used to treat high blood pressure, were 40 percent less likely to be hospitalized than those who were not taking the drug.
The connection between ACE inhibitors and COVID hospitalizations was a correlation, a statistical association. To determine whether the drugs had any real effect on COVID outcomes, United would have to perform another, more rigorous study. They would have to assign some people to receive small doses of ACE inhibitors, and others to receive placebos, and measure the outcomes under each condition. They planned to do this virtually, allowing study participants to sign up and be screened online, and sending drugs, thermometers, and tests through the mail. There were two reasons to do it this way: First, the U.S. Food and Drug Administration had been advising medical researchers to embrace new strategies in clinical trials as a way to protect participants during the pandemic.
The second reason was why they asked Herman Taylor to co-supervise it: Clinical trials have long had a diversity problem. And going virtual is a potential solution.
Since the beginning of the pandemic, COVID-19 has infected people of color at a rate of three times that of Caucasians (killing Black people at a rate 2.5 times as high, and Hispanic and American Indian or Alaska Native people at a rate 1.3 times as high). A number of explanations have been put forth to explain this disproportionate toll. Among them: higher levels of poverty, essential jobs that increase exposure, and lower quality or inadequate access to medical care.
Unfortunately, these same factors also affect who participates in research. People of color may be less likely to have doctors recommend studies to them. They may not have the time or the resources to hang out in a waiting room for hours. They may not live near large research institutions that conduct trials. The result is that new treatments, even for diseases that affect Latin, Native American, or African American populations in greater proportions, are studied mostly in white volunteers. The very people who most require solutions to COVID are those who are least likely to be involved in the search to find them.
Virtual trials can alleviate a number of these problems. Not only can people find and request to participate in these types of trials through their phones or computers, virtual trials also cover more costs, include a larger geographical range, and have inherently flexible hours.
"[In a traditional study] you have to go to a doctor's office to enroll and drive a couple of hours and pay $20 for parking and pay $15 for a sandwich in the hospital cafeteria and arrange for daycare for your kids and take time off of work," says Dr. Jonathan Cotliar, chief medical officer of Science37, a platform that investigators can hire to host and organize their trials virtually. "That's a lot just for one visit, much less over the course of a six to 12-month study."
Cotliar's data suggests that virtual trials' enhanced access seriously affects the racial makeup of a given study's participant pool. Sixty percent of patients enrolled in Science37 trials are non-Caucasian, which is, Cotliar says, "staggering compared to what you find in traditional site-based research."
But access is not the only barrier to including more people of color in clinical trials. There is also trust. When agreeing to sign up for research, undocumented immigrants may worry about finding themselves in legal trouble or without any medical support should something go wrong. In a country with a history of experimenting on African Americans without their consent, black people may not trust institutions not to use them as guinea pigs.
"A lot of people report being somewhat disregarded or disrespected once entering the healthcare system," Taylor says. "You take it all together, then people wonder, well, okay, this is how the system tends to regard me, yet now here come these people doing research, and they're all about getting me into their studies." Not so surprising that a lot of people may respond with a resounding "No thanks."
United's ACE inhibitor trial was notable for addressing both of these challenges. In addition to covering costs and allowing study subjects to participate from their own homes, it was being co-sponsored by a professor at Morehouse, one of the country's historic black colleges and universities (often abbreviated HBCUs). United was recruiting heavily in Atlanta, whose population is 52 percent African American. The study promised a thoughtful introduction to a more egalitarian future of medical research.
There's just one problem: It isn't going to happen.
This month, in preparation for the study, United reanalyzed their ACE inhibitor data with all the new patients who'd contracted COVID in the months since their first analysis. Their original data set had been concentrated in the Northeast, mostly New York City, where the earliest outbreak took place. In the 12 weeks it had taken them to set up the virtual followup study, epicenters had shifted. United's second, more geographically comprehensive sample had ten times the number of people in it. And in that sample, the signal simply disappeared.
"I was shocked, but that's the reality," says Deneen Vojta, executive vice president of enterprise research and development for UnitedHealth Group. "You make decisions based on the data, but when you get more data, more information, you might make a different decision. The answer is the answer."
There was no point in running a virtual ACE inhibitor study if a larger, more representative sample of people indicated the drug was unlikely to help anyone. Still, the model United had established to run the trial remains viable. Even as she scrapped the ACE inhibitor study, Vojta hoped not just to continue United's relationship with Dr. Taylor and Morehouse, but to formalize it. Virtual platforms are still an important part of their forthcoming trials.
If people don't believe a vaccine has been created with them in mind, then they won't take it, and it won't matter whether it exists or not.
United is not alone in this approach. As phase three trials for vaccines against SARS CoV-2 get underway, big pharma companies have been publicly articulating their own strategies for including more people of color in clinical trials, and many of these include virtual elements. Janelle Sabo, global head of clinical innovation, systems and clinical supply chain at Eli Lilly, told me that the company is employing home health and telemedicine, direct-to-patient shipping and delivery, and recruitment using social media and geolocation to expand access to more diverse populations.
Dr. Macaya Douoguih, Head of Clinical Development and Medical Affairs for Janssen Vaccines under Johnson & Johnson, spoke to Congress about this issue during a July hearing before the House Energy and Commerce Oversight and Investigations Subcommittee. She said that the company planned to institute a "focused digital and community outreach plan to provide resources and opportunities to encourage participation in our clinical trials," and had partnered with Johns Hopkins Bloomberg School of Public Health "to understand how the COVID-19 crisis is affecting different communities in the United States."
But while some of these plans are well thought-out, others are concerningly nebulous, featuring big pronouncements but fewer tangible strategies. In that same July hearing, Massachusetts representative Joe Kennedy III (D) sounded like a frustrated teacher when admonishing four of the five leads of the present pharma companies (AstraZeneca, Johnson & Johnson, Merck, Moderna, and Pfizer) for not explaining exactly how they'd ensure diversity both in the study of their vaccines, and in their eventual distribution.
This matters: The uptake of the flu vaccine is 10 percentage points lower in both the African American and Hispanic communities than it is in Caucasians. A Pew research study conducted early in the pandemic found that just 54 percent of Black adults said they "would definitely or probably get a coronavirus vaccine," compared to 74 percent of Whites and Hispanics.
"As a good friend of mine, Dr. [James] Hildreth, president at Meharry, another HBC medical school, likes to say: 'A vaccine is great, but it is the vaccination that saves people,'" Taylor says. If people don't believe a vaccine has been created with them in mind, then they won't take it, and it won't matter whether it exists or not.
In this respect, virtual platforms remain an important first step, at least in expanding admittance. In June, United Health opened up a trial to their entire workforce for a computer game that could treat ADHD. In less than two months, 1,743 people had signed up for it, from all different socioeconomic groups, from all over the country. It was inching closer to the kind of number you need for a phase three vaccine trial, which can require tens of thousands of people. Back when they'd been planning the ACE inhibitor study, United had wanted 9,600 people to agree to participate.
Now, with the help of virtual enrollment, they hope they can pull off similarly high numbers for the COVID vaccine trial they will be running for an as-yet-unnamed pharmaceutical partner. It stands to open in September.

