How Leqembi became the biggest news in Alzheimer’s disease in 40 years, and what comes next

Betsy Groves, 73, with her granddaughter. Groves learned in 2021 that she has Alzheimer's disease. She hopes to take Leqembi, a drug approved by the FDA last week.
A few months ago, Betsy Groves traveled less than a mile from her home in Cambridge, Mass. to give a talk to a bunch of scientists. The scientists, who worked for the pharmaceutical companies Biogen and Eisai, wanted to know how she lived her life, how she thought about her future, and what it was like when a doctor’s appointment in 2021 gave her the worst possible news. Groves, 73, has Alzheimer’s disease. She caught it early, through a lumbar puncture that showed evidence of amyloid, an Alzheimer’s hallmark, in her cerebrospinal fluid. As a way of dealing with her diagnosis, she joined the Alzheimer’s Association’s National Early-Stage Advisory Board, which helped her shift into seeing her diagnosis as something she could use to help others.
After her talk, Groves stayed for lunch with the scientists, who were eager to put a face to their work. Biogen and Eisai were about to release the first drug to successfully combat Alzheimer’s in 40 years of experimental disaster. Their drug, which is known by the scientific name lecanemab and the marketing name Leqembi, was granted accelerated approval by the U.S. Food and Drug Administration last Friday, Jan. 6, after a study in 1,800 people showed that it reduced cognitive decline by 27 percent over 18 months.
It is no exaggeration to say that this result is a huge deal. The field of Alzheimer’s drug development has been absolutely littered with failures. Almost everything researchers have tried has tanked in clinical trials. “Most of the things that we've done have proven not to be effective, and it's not because we haven’t been taking a ton of shots at goal,” says Anton Porsteinsson, director of the University of Rochester Alzheimer's Disease Care, Research, and Education Program, who worked on the lecanemab trial. “I think it's fair to say you don't survive in this field unless you're an eternal optimist.”
As far back as 1984, a cure looked like it was within reach: Scientists discovered that the sticky plaques that develop in the brains of those who have Alzheimer’s are made up of a protein fragment called beta-amyloid. Buildup of beta-amyloid seemed to be sufficient to disrupt communication between, and eventually kill, memory cells. If that was true, then the cure should be straightforward: Stop the buildup of beta-amyloid; stop the Alzheimer’s disease.
It wasn’t so simple. Over the next 38 years, hundreds of drugs designed either to interfere with the production of abnormal amyloid or to clear it from the brain flamed out in trials. It got so bad that neuroscience drug divisions at major pharmaceutical companies (AstraZeneca, Pfizer, Bristol-Myers, GSK, Amgen) closed one by one, leaving the field to smaller, scrappier companies, like Cambridge-based Biogen and Tokyo-based Eisai. Some scientists began to dismiss the amyloid hypothesis altogether: If this protein fragment was so important to the disease, why didn’t ridding the brain of it do anything for patients? There was another abnormal protein that showed up in the brains of Alzheimer’s patients, called tau. Some researchers defected to the tau camp, or came to believe the proteins caused damage in combination.
The situation came to a head in 2021, when the FDA granted provisional approval to a drug called aducanumab, marketed as Aduhelm, against the advice of its own advisory council. The approval was based on proof that Aduhelm reduced beta-amyloid in the brain, even though one research trial showed it had no effect on people’s symptoms or daily life. Aduhelm could also cause serious side effects, like brain swelling and amyloid related imaging abnormalities (known as ARIA, these are basically micro-bleeds that appear on MRI scans). Without a clear benefit to memory loss that would make these risks worth it, Medicare refused to pay for Aduhelm among the general population. Two congressional committees launched an investigation into the drug’s approval, citing corporate greed, lapses in protocol, and an unjustifiably high price. (Aduhelm was also produced by the pharmaceutical company Biogen.)
To be clear, Leqembi is not the cure Alzheimer’s researchers hope for. While the drug is the first to show clear signs of a clinical benefit, the scientific establishment is split on how much of a difference Leqembi will make in the real world.
So far, Leqembi is like Aduhelm in that it has been given accelerated approval only for its ability to remove amyloid from the brain. Both are monoclonal antibodies that direct the immune system to attack and clear dysfunctional beta-amyloid. The difference is that, while that’s all Aduhelm was ever shown to do, Leqembi’s makers have already asked the FDA to give it full approval – a decision that would increase the likelihood that Medicare will cover it – based on data that show it also improves Alzheimer’s sufferer’s lives. Leqembi targets a different type of amyloid, a soluble version called “protofibrils,” and that appears to change the effect. “It can give individuals and their families three, six months longer to be participating in daily life and living independently,” says Claire Sexton, PhD, senior director of scientific programs & outreach for the Alzheimer's Association. “These types of changes matter for individuals and for their families.”
To be clear, Leqembi is not the cure Alzheimer’s researchers hope for. It does not halt or reverse the disease, and people do not get better. While the drug is the first to show clear signs of a clinical benefit, the scientific establishment is split on how much of a difference Leqembi will make in the real world. It has “a rather small effect,” wrote NIH Alzheimer’s researcher Madhav Thambisetty, MD, PhD, in an email to Leaps.org. “It is unclear how meaningful this difference will be to patients, and it is unlikely that this level of difference will be obvious to a patient (or their caregivers).” Another issue is cost: Leqembi will become available to patients later this month, but Eisai is setting the price at $26,500 per year, meaning that very few patients will be able to afford it unless Medicare chooses to reimburse them for it.
The same side effects that plagued Aduhelm are common in Leqembi treatment as well. In many patients, amyloid doesn’t just accumulate around neurons, it also forms deposits in the walls of blood vessels. Blood vessels that are shot through with amyloid are more brittle. If you infuse a drug that targets amyloid, brittle blood vessels in the brain can develop leakage that results in swelling or bleeds. Most of these come with no symptoms, and are only seen during testing, which is why they are called “imaging abnormalities.” But in situations where patients have multiple diseases or are prescribed incompatible drugs, they can be serious enough to cause death. The three deaths reported from Leqembi treatment (so far) are enough to make Thambisetty wonder “how well the drug may be tolerated in real world clinical practice where patients are likely to be sicker and have multiple other medical conditions in contrast to carefully selected patients in clinical trials.”
Porsteinsson believes that earlier detection of Alzheimer’s disease will be the next great advance in treatment, a more important step forward than Leqembi’s approval.
Still, there are reasons to be excited. A successful Alzheimer’s drug can pave the way for combination studies, in which patients try a known effective drug alongside newer, more experimental ones; or preventative studies, which take place years before symptoms occur. It also represents enormous strides in researchers’ understanding of the disease. For example, drug dosages have increased massively—in some cases quadrupling—from the early days of Alzheimer’s research. And patient selection for studies has changed drastically as well. Doctors now know that you’ve got to catch the disease early, through PET-scans or CSF tests for amyloid, if you want any chance of changing its course.
Porsteinsson believes that earlier detection of Alzheimer’s disease will be the next great advance in treatment, a more important step forward than Leqembi’s approval. His lab already uses blood tests for different types of amyloid, for different types of tau, and for measures of neuroinflammation, neural damage, and synaptic health, but commercially available versions from companies like C2N, Quest, and Fuji Rebio are likely to hit the market in the next couple of years. “[They are] going to transform the diagnosis of Alzheimer's disease,” Porsteinsson says. “If someone is experiencing memory problems, their physicians will be able to order a blood test that will tell us if this is the result of changes in your brain due to Alzheimer's disease. It will ultimately make it much easier to identify people at a very early stage of the disease, where they are most likely to benefit from treatment.”
Learn more about new blood tests to detect Alzheimer's
Early detection can help patients for more philosophical reasons as well. Betsy Groves credits finding her Alzheimer’s early with giving her the space to understand and process the changes that were happening to her before they got so bad that she couldn’t. She has been able to update her legal documents and, through her role on the Advisory Group, help the Alzheimer’s Association with developing its programs and support services for people in the early stages of the disease. She still drives, and because she and her husband love to travel, they are hoping to get out of grey, rainy Cambridge and off to Texas or Arizona this spring.
Because her Alzheimer’s disease involves amyloid deposits (a “substantial portion” do not, says Claire Sexton, which is an additional complication for research), and has not yet reached an advanced stage, Groves may be a good candidate to try Leqembi. She says she’d welcome the opportunity to take it. If she can get access, Groves hopes the drug will give her more days to be fully functioning with her husband, daughters, and three grandchildren. Mostly, she avoids thinking about what the latter stages of Alzheimer’s might be like, but she knows the time will come when it will be her reality. “So whatever lecanemab can do to extend my more productive ways of engaging with relationships in the world,” she says. “I'll take that in a minute.”
Out of Thin Air: A Fresh Solution to Farming’s Water Shortages
Dry, arid and remote farming regions are vulnerable to water shortages, but scientists are working on a promising new solution.
California has been plagued by perilous droughts for decades. Freshwater shortages have sparked raging wildfires and killed fruit and vegetable crops. And California is not alone in its danger of running out of water for farming; parts of the Southwest, including Texas, are battling severe drought conditions, according to the North American Drought Monitor. These two states account for 316,900 of the 2 million total U.S. farms.
But even as farming becomes more vulnerable due to water shortages, the world's demand for food is projected to increase 70 percent by 2050, according to Guihua Yu, an associate professor of materials science at The University of Texas at Austin.
"Water is the most limiting natural resource for agricultural production because of the freshwater shortage and enormous water consumption needed for irrigation," Yu said.
As scientists have searched for solutions, an alternative water supply has been hiding in plain sight: Water vapor in the atmosphere. It is abundant, available, and endlessly renewable, just waiting for the moment that technological innovation and necessity converged to make it fit for use. Now, new super-moisture-absorbent gels developed by Yu and a team of researchers can pull that moisture from the air and bring it into soil, potentially expanding the map of farmable land around the globe to dry and remote regions that suffer from water shortages.
"This opens up opportunities to turn those previously poor-quality or inhospitable lands to become useable and without need of centralized water and power supplies," Yu said.
A renewable source of freshwater
The hydrogels are a gelatin-like substance made from synthetic materials. The gels activate in cooler, humid overnight periods and draw water from the air. During a four-week experiment, Yu's team observed that soil with these gels provided enough water to support seed germination and plant growth without an additional liquid water supply. And the soil was able to maintain the moist environment for more than a month, according to Yu.
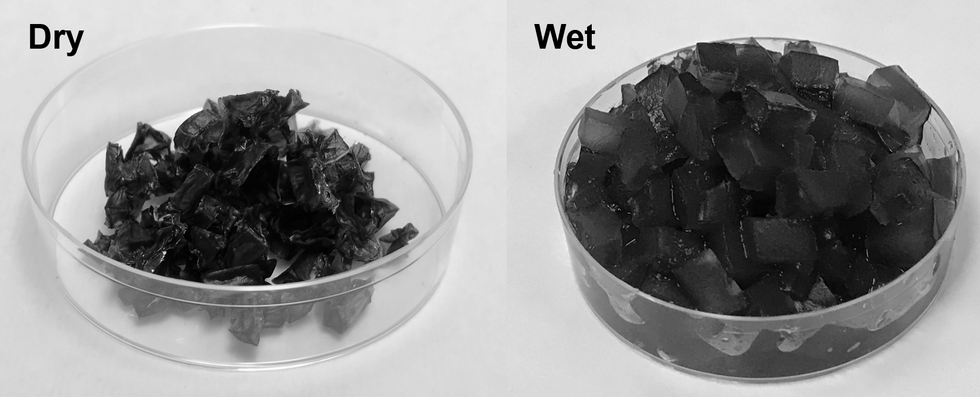
The super absorbent gels developed at the University of Texas at Austin.
Xingyi Zhou, UT Austin
"It is promising to liberate underdeveloped and drought areas from the long-distance water and power supplies for agricultural production," Yu said.
Crops also rely on fertilizer to maintain soil fertility and increase the production yield, but it is easily lost through leaching. Runoff increases agricultural costs and contributes to environmental pollution. The interaction between the gels and agrochemicals offer slow and controlled fertilizer release to maintain the balance between the root of the plant and the soil.
The possibilities are endless
Harvesting atmospheric water is exciting on multiple fronts. The super-moisture-absorbent gel can also be used for passively cooling solar panels. Solar radiation is the magic behind the process. Overnight, as temperatures cool, the gels absorb water hanging in the atmosphere. The moisture is stored inside the gels until the thermometer rises. Heat from the sun serves as the faucet that turns the gels on so they can release the stored water and cool down the panels. Effective cooling of the solar panels is important for sustainable long-term power generation.
In addition to agricultural uses and cooling for energy devices, atmospheric water harvesting technologies could even reach people's homes.
"They could be developed to enable easy access to drinking water through individual systems for household usage," Yu said.
Next steps
Yu and the team are now focused on affordability and developing practical applications for use. The goal is to optimize the gel materials to achieve higher levels of water uptake from the atmosphere.
"We are exploring different kinds of polymers and solar absorbers while exploring low-cost raw materials for production," Yu said.
The ability to transform atmospheric water vapor into a cheap and plentiful water source would be a game-changer. One day in the not-too-distant future, if climate change intensifies and droughts worsen, this innovation may become vital to our very survival.
On left, people excitedly line up for Salk's polio vaccine in 1957; on right, Joe Biden gets one of the COVID vaccines on December 21, 2020.
On the morning of April 12, 1955, newsrooms across the United States inked headlines onto newsprint: the Salk Polio vaccine was "safe, effective, and potent." This was long-awaited news. Americans had limped through decades of fear, unaware of what caused polio or how to cure it, faced with the disease's terrifying, visible power to paralyze and kill, particularly children.
The announcement of the polio vaccine was celebrated with noisy jubilation: church bells rang, factory whistles sounded, people wept in the streets. Within weeks, mass inoculation began as the nation put its faith in a vaccine that would end polio.
Today, most of us are blissfully ignorant of child polio deaths, making it easier to believe that we have not personally benefited from the development of vaccines. According to Dr. Steven Pinker, cognitive psychologist and author of the bestselling book Enlightenment Now, we've become blasé to the gifts of science. "The default expectation is not that disease is part of life and science is a godsend, but that health is the default, and any disease is some outrage," he says.
We're now in the early stages of another vaccine rollout, one we hope will end the ravages of the COVID-19 pandemic. And yet, the Pfizer, Moderna, and AstraZeneca vaccines are met with far greater hesitancy and skepticism than the polio vaccine was in the 50s.
In 2021, concerns over the speed and safety of vaccine development and technology plague this heroic global effort, but the roots of vaccine hesitancy run far deeper. Vaccine hesitancy has always existed in the U.S., even in the polio era, motivated in part by fears around "living virus" in a bad batch of vaccines produced by Cutter Laboratories in 1955. But in the last half century, we've witnessed seismic cultural shifts—loss of public trust, a rise in misinformation, heightened racial and socioeconomic inequality, and political polarization have all intensified vaccine-related fears and resistance. Making sense of how we got here may help us understand how to move forward.
The Rise and Fall of Public Trust
When the polio vaccine was released in 1955, "we were nearing an all-time high point in public trust," says Matt Baum, Harvard Kennedy School professor and lead author of several reports measuring public trust and vaccine confidence. Baum explains that the U.S. was experiencing a post-war boom following the Allied triumph in WWII, a popular Roosevelt presidency, and the rapid innovation that elevated the country to an international superpower.
The 1950s witnessed the emergence of nuclear technology, a space program, and unprecedented medical breakthroughs, adds Emily Brunson, Texas State University anthropologist and co-chair of the Working Group on Readying Populations for COVID-19 Vaccine. "Antibiotics were a game changer," she states. While before, people got sick with pneumonia for a month, suddenly they had access to pills that accelerated recovery.
During this period, science seemed to hold all the answers; people embraced the idea that we could "come to know the world with an absolute truth," Brunson explains. Doctors were portrayed as unquestioned gods, so Americans were primed to trust experts who told them the polio vaccine was safe.
"The emotional tone of the news has gone downward since the 1940s, and journalists consider it a professional responsibility to cover the negative."
That blind acceptance eroded in the 1960s and 70s as people came to understand that science can be inherently political. "Getting to an absolute truth works out great for white men, but these things affect people socially in radically different ways," Brunson says. As the culture began questioning the white, patriarchal biases of science, doctors lost their god-like status and experts were pushed off their pedestals. This trend continues with greater intensity today, as President Trump has led a campaign against experts and waged a war on science that began long before the pandemic.
The Shift in How We Consume Information
In the 1950s, the media created an informational consensus. The fundamental ideas the public consumed about the state of the world were unified. "People argued about the best solutions, but didn't fundamentally disagree on the factual baseline," says Baum. Indeed, the messaging around the polio vaccine was centralized and consistent, led by President Roosevelt's successful March of Dimes crusade. People of lower socioeconomic status with limited access to this information were less likely to have confidence in the vaccine, but most people consumed media that assured them of the vaccine's safety and mobilized them to receive it.
Today, the information we consume is no longer centralized—in fact, just the opposite. "When you take that away, it's hard for people to know what to trust and what not to trust," Baum explains. We've witnessed an increase in polarization and the technology that makes it easier to give people what they want to hear, reinforcing the human tendencies to vilify the other side and reinforce our preexisting ideas. When information is engineered to further an agenda, each choice and risk calculation made while navigating the COVID-19 pandemic is deeply politicized.
This polarization maps onto a rise in socioeconomic inequality and economic uncertainty. These factors, associated with a sense of lost control, prime people to embrace misinformation, explains Baum, especially when the situation is difficult to comprehend. "The beauty of conspiratorial thinking is that it provides answers to all these questions," he says. Today's insidious fragmentation of news media accelerates the circulation of mis- and disinformation, reaching more people faster, regardless of veracity or motivation. In the case of vaccines, skepticism around their origin, safety, and motivation is intensified.
Alongside the rise in polarization, Pinker says "the emotional tone of the news has gone downward since the 1940s, and journalists consider it a professional responsibility to cover the negative." Relentless focus on everything that goes wrong further erodes public trust and paints a picture of the world getting worse. "Life saved is not a news story," says Pinker, but perhaps it should be, he continues. "If people were more aware of how much better life was generally, they might be more receptive to improvements that will continue to make life better. These improvements don't happen by themselves."
The Future Depends on Vaccine Confidence
So far, the U.S. has been unable to mitigate the catastrophic effects of the pandemic through social distancing, testing, and contact tracing. President Trump has downplayed the effects and threat of the virus, censored experts and scientists, given up on containing the spread, and mobilized his base to protest masks. The Trump Administration failed to devise a national plan, so our national plan has defaulted to hoping for the "miracle" of a vaccine. And they are "something of a miracle," Pinker says, describing vaccines as "the most benevolent invention in the history of our species." In record-breaking time, three vaccines have arrived. But their impact will be weakened unless we achieve mass vaccination. As Brunson notes, "The technology isn't the fix; it's people taking the technology."
Significant challenges remain, including facilitating widespread access and supporting on-the-ground efforts to allay concerns and build trust with specific populations with historic reasons for distrust, says Brunson. Baum predicts continuing delays as well as deaths from other causes that will be linked to the vaccine.
Still, there's every reason for hope. The new administration "has its eyes wide open to these challenges. These are the kind of problems that are amenable to policy solutions if we have the will," Baum says. He forecasts widespread vaccination by late summer and a bounce back from the economic damage, a "Good News Story" that will bolster vaccine acceptance in the future. And Pinker reminds us that science, medicine, and public health have greatly extended our lives in the last few decades, a trend that can only continue if we're willing to roll up our sleeves.

