Scientists Are Harnessing Sound Waves in Hopes of Treating Alzheimer’s
Researchers at Columbia University are testing an experimental treatment for Alzheimer's that uses ultrasound waves and "microbubbles."
In 2010, a 67-year-old former executive assistant for a Fortune 500 company was diagnosed with mild cognitive impairment. By 2014, her doctors confirmed she had Alzheimer's disease.
As her disease progressed, she continued to live independently but wasn't able to drive anymore. Today, she can manage most of her everyday tasks, but her two daughters are considering a live-in caregiver. Despite her condition, the woman may represent a beacon of hope for the approximately 44 million people worldwide living with Alzheimer's disease. The now 74-year-old is among a small cadre of Alzheimer's patients who have undergone an experimental ultrasound procedure aimed at slowing cognitive decline.
In November 2020, Elisa Konofagou, a professor of biomedical engineering and director of the Ultrasound and Elasticity Imaging Laboratory at Columbia University, and her team used ultrasound to noninvasively open the woman's blood-brain barrier. This barrier is a highly selective membrane of cells that prevents toxins and pathogens from entering the brain while allowing vital nutrients to pass through. This regulatory function means the blood-brain barrier filters out most drugs, making treating Alzheimer's and other brain diseases a challenge.
Ultrasound uses high-frequency sound waves to produce live images from the inside of the human body. But scientists think it could also be used to boost the effectiveness of Alzheimer's drugs, or potentially even improve brain function in dementia patients without the use of drugs.
The procedure, which involves a portable ultrasound system, is the culmination of 17 years of lab work. As part of a small clinical trial, scientists positioned a sensor transmitting ultrasound waves on top of the woman's head while she sat in a chair. The sensor sends ultrasound pulses throughout the target region. Meanwhile, investigators intravenously infused microbubbles into the woman to boost the effects of the ultrasound. Three days after the procedure, scientists scanned her brain so that they could measure the effects of the treatments. Five months later, they took more images of her brain to see if the effects of the treatment lasted.
Promising Signs
After the first brain scan, Konofagou and her team found that amyloid-beta, the protein that clumps together in the brains of Alzheimer's patients and disrupts cell function, had declined by 14%. At the woman's second scan, amyloid levels were still lower than before the experimental treatment, but only by 10% this time. Konofagou thinks repeat ultrasound treatments given early on in the development of Alzheimer's may have the best chance at keeping amyloid plaques at bay.
This reduction in amyloid appeared to halt the woman's cognitive decline, at least temporarily. Following the ultrasound treatment, the woman took a 30-point test used to measure cognitive impairment in Alzheimer's. Her score — 22, indicating mild cognitive impairment — remained the same as before the intervention. Konofagou says this was actually a good sign.
"Typically, every six months an Alzheimer's patient scores two to three points lower, so this is highly encouraging," she says.
Konofagou speculates that the results might have been even more impressive had they applied the ultrasound on a larger section of the brain at a higher frequency. The selected site was just 4 cubic centimeters. Current safety protocols set by the U.S. Food and Drug Administration stipulate that investigators conducting such trials only treat one brain region with the lowest pressure possible.
The Columbia trial is aided by microbubble technology. During the procedure, investigators infused tiny, gas-filled spheres into the woman's veins to enhance the ultrasound reflection of the sound waves.
The big promise of ultrasound is that it could eventually make drugs for Alzheimer's obsolete.
"Ultrasound with microbubbles wakes up immune cells that go on to discard amyloid-beta," Konofagou says. "In this way, we can recover the function of brain neurons, which are destroyed by Alzheimer's in a sort of domino effect." What's more, a drug delivered alongside ultrasound can penetrate the brain at a dose up to 10 times higher.
Costas Arvanitis, an assistant professor at Georgia Institute of Technology who studies ultrasonic biophysics and isn't involved in the Columbia trial, is excited about the research. "First, by applying ultrasound you can make larger drugs — picture an antibody — available to the brain," he says. Then, you can use ultrasound to improve the therapeutic index, or the ratio of the effectiveness of a drug versus the ratio of adverse effects. "Some drugs might be effective but because we have to provide them in high doses to see significant responses they tend to come with side effects. By improving locally the concentration of a drug, you open up the possibility to reduce the dose."
The Columbia trial will enroll just six patients and is designed to test the feasibility and safety of the approach, not its efficacy. Still, Arvantis is hopeful about the potential benefits of the technique. "The technology has already been demonstrated to be safe, its components are now tuned to the needs of this specific application, and it's safe to say it's only a matter of time before we are able to develop personalized treatments," he says.
Konofagou and her colleagues recently presented their findings at the 20th Annual International Symposium for Therapeutic Ultrasound and intend to publish them in a scientific journal later this year. They plan to recruit more participants for larger trials, which will determine how effective the therapy is at improving memory and brain function in Alzheimer's patients. They're also in talks with pharmaceutical companies about ways to use their therapeutic approach to improve current drugs or even "create new drugs," says Konofagou.
A New Treatment Approach
On June 7, the FDA approved the first Alzheimer's disease drug in nearly two decades. Aducanumab, a drug developed by Biogen, is an antibody designed to target and reduce amyloid plaques. The drug has already sparked immense enthusiasm — and controversy. Proponents say the drug is a much-needed start in the fight against the disease, but others argue that the drug doesn't substantially improve cognition. They say the approval could open the door to the FDA greenlighting more Alzheimer's drugs that don't have a clear benefit, giving false hope to both patients and their families.
Konofagou's ultrasound approach could potentially boost the effects of drugs like aducanumab. "Our technique can be seamlessly combined with aducanumab in early Alzheimer's, where it has shown the most promise, to further enhance both its amyloid load reduction and further reduce cognitive deficits while using exactly the same drug regimen otherwise," she says. For the Columbia team, the goal is to use ultrasound to maximize the effects of aducanumab, as they've done with other drugs in animal studies.
But Konofagou's approach could transcend drug controversies, and even drugs altogether. The big promise of ultrasound is that it could eventually make drugs for Alzheimer's obsolete.
"There are already indications that the immune system is alerted each time ultrasound is exerted on the brain or when the brain barrier is being penetrated and gets activated, which on its own may have sufficient therapeutic effects," says Konofagou. Her team is now working with psychiatrists in hopes of using brain stimulation to treat patients with depression.
The potential to modulate the brain without drugs is huge and untapped, says Kim Butts Pauly, a professor of radiology, electrical engineering and bioengineering at Stanford University, who's not involved in the Columbia study. But she admits that scientists don't know how to fully control ultrasound in the brain yet. "We're only at the starting point of getting the tools to understand and harness how ultrasound microbubbles stimulate an immune response in the brain."
Meanwhile, the 74-year-old woman who received the ultrasound treatment last year, goes on about her life, having "both good days and bad days," her youngest daughter says. COVID-19's isolation took a toll on her, but both she and her daughters remain grateful for the opportunity to participate in the ultrasound trial.
"My mother wants to help, if not for herself, then for those who will follow her," the daughter says. She hopes her mother will be able to join the next phase of the trial, which will involve a drug in conjunction with the ultrasound treatment. "This may be the combination where the magic will happen," her daughter says.
Health breakthroughs of 2022 that should have made bigger news
Nine experts break down the biggest biotech and health breakthroughs that didn't get the attention they deserved in 2022.
As the world has attempted to move on from COVID-19 in 2022, attention has returned to other areas of health and biotech with major regulatory approvals such as the Alzheimer's drug lecanemab – which can slow the destruction of brain cells in the early stages of the disease – being hailed by some as momentous breakthroughs.
This has been a year where psychedelic medicines have gained the attention of mainstream researchers with a groundbreaking clinical trial showing that psilocybin treatment can help relieve some of the symptoms of major depressive disorder. And with messenger RNA (mRNA) technology still very much capturing the imagination, the readouts of cancer vaccine trials have made headlines around the world.
But at the same time there have been vital advances which will likely go on to change medicine, and yet have slipped beneath the radar. I asked nine forward-thinking experts on health and biotech about the most important, but underappreciated, breakthrough of 2022.
Their descriptions, below, were lightly edited by Leaps.org for style and format.
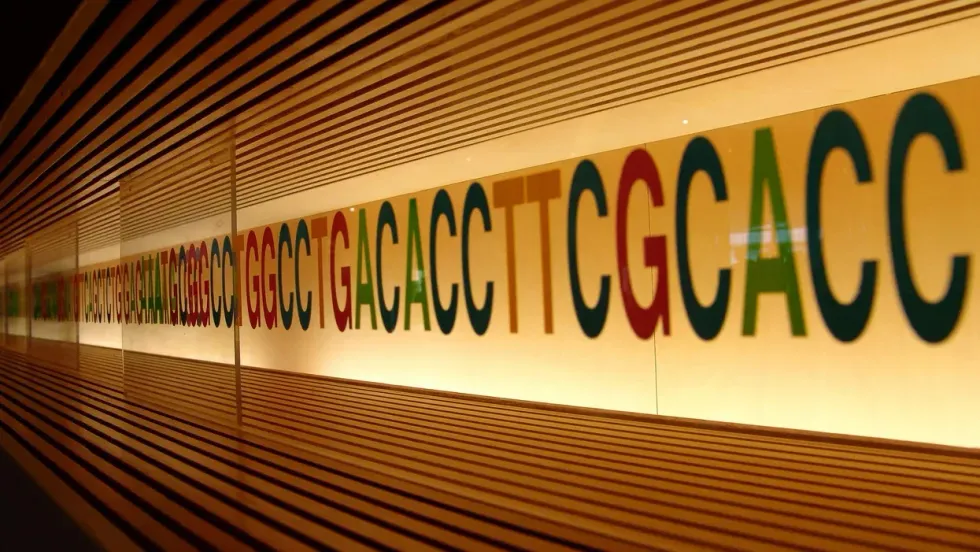
New drug targets for Alzheimer’s disease

Professor Julie Williams, Director, Dementia Research Institute, Cardiff University
Genetics has changed our view of Alzheimer’s disease in the last five to six years. The beta amyloid hypothesis has dominated Alzheimer’s research for a long time, but there are multiple components to this complex disease, of which getting rid of amyloid plaques is one, but it is not the whole story. In April 2022, Nature published a paper which is the culmination of a decade’s worth of work - groups all over the world working together to identify 75 genes associated with risk of developing Alzheimer’s. This provides us with a roadmap for understanding the disease mechanisms.
For example, it is showing that there is something different about the immune systems of people who develop Alzheimer’s disease. There is something different about the way they process lipids in the brain, and very specific processes of how things travel through cells called endocytosis. When it comes to immunity, it indicates that the complement system is affecting whether synapses, which are the connections between neurons, get eliminated or not. In Alzheimer’s this process is more severe, so patients are losing more synapses, and this is correlated with cognition.
The genetics also implicates very specific tissues like microglia, which are the housekeepers in the brain. One of their functions is to clear away beta amyloid, but they also prune and nibble away at parts of the brain that are indicated to be diseased. If you have these risk genes, it seems that you are likely to prune more tissue, which may be part of the cell death and neurodegeneration that we observe in Alzheimer’s patients.
Genetics is telling us that we need to be looking at multiple causes of this complex disease, and we are doing that now. It is showing us that there are a number of different processes which combine to push patients into a disease state which results in the death of connections between nerve cells. These findings around the complement system and other immune-related mechanisms are very interesting as there are already drugs which are available for other diseases which could be repurposed in clinical trials. So it is really a turning point for us in the Alzheimer’s disease field.
Preventing Pandemics with Organ-Tissue Equivalents

Anthony Atala, Director of the Wake Forest Institute for Regenerative Medicine
COVID-19 has shown us that we need to be better prepared ahead of future pandemics and have systems in place where we can quickly catalogue a new virus and have an idea of which treatment agents would work best against it.
At Wake Forest Institute, our scientists have developed what we call organ-tissue equivalents. These are miniature tissues and organs, created using the same regenerative medicine technologies which we have been using to create tissues for patients. For example, if we are making a miniature liver, we will recreate this structure using the six different cell types you find in the liver, in the right proportions, and then the right extracellular matrix which holds the structure together. You're trying to replicate all the characteristics of the liver, but just in a miniature format.
We can now put these organ-tissue equivalents in a chip-like device, where we can expose them to different types of viral infections, and start to get a realistic idea of how the human body reacts to these viruses. We can use artificial intelligence and machine learning to map the pathways of the body’s response. This will allow us to catalogue known viruses far more effectively, and begin storing information on them.
Powering Deep Brain Stimulators with Breath

Islam Mosa, Co-Founder and CTO of VoltXon
Deep brain stimulation (DBS) devices are becoming increasingly common with 150,000 new devices being implanted every year for people with Parkinson’s disease, but also psychiatric conditions such as treatment-resistant depression and obsessive-compulsive disorders. But one of the biggest limitations is the power source – I call DBS devices energy monsters. While cardiac pacemakers use similar technology, their batteries last seven to ten years, but DBS batteries need changing every two to three years. This is because they are generating between 60-180 pulses per second.
Replacing the batteries requires surgery which costs a lot of money, and with every repeat operation comes a risk of infection, plus there is a lot of anxiety on behalf of the patient that the battery is running out.
My colleagues at the University of Connecticut and I, have developed a new way of charging these devices using the person’s own breathing movements, which would mean that the batteries never need to be changed. As the patient breathes in and out, their chest wall presses on a thin electric generator, which converts that movement into static electricity, charging a supercapacitor. This discharges the electricity required to power the DBS device and send the necessary pulses to the brain.
So far it has only been tested in a simulated pig, using a pig lung connected to a pump, but there are plans now to test it in a real animal, and then progress to clinical trials.
Smartwatches for Disease Detection
Jessilyn Dunn, Assistant Professor in Duke Biomedical Engineering
A group of researchers recently showed that digital biomarkers of infection can reveal when someone is sick, often before they feel sick. The team, which included Duke biomedical engineers, used information from smartwatches to detect Covid-19 cases five to 10 days earlier than diagnostic tests. Smartwatch data included aspects of heart rate, sleep quality and physical activity. Based on this data, we developed an algorithm to decide which people have the most need to take the diagnostic tests. With this approach, the percent of tests that come back positive are about four- to six-times higher, depending on which factors we monitor through the watches.
Our study was one of several showing the value of digital biomarkers, rather than a single blockbuster paper. With so many new ideas and technologies coming out around Covid, it’s hard to be that signal through the noise. More studies are needed, but this line of research is important because, rather than treat everyone as equally likely to have an infectious disease, we can use prior knowledge from smartwatches. With monkeypox, for example, you've got many more people who need to be tested than you have tests available. Information from the smartwatches enables you to improve how you allocate those tests.
Smartwatch data could also be applied to chronic diseases. For viruses, we’re looking for information about anomalies – a big change point in people’s health. For chronic diseases, it’s more like a slow, steady change. Our research lays the groundwork for the signals coming from smartwatches to be useful in a health setting, and now it’s up to us to detect more of these chronic cases. We want to go from the idea that we have this single change point, like a heart attack or stroke, and focus on the part before that, to see if we can detect it.
A Vaccine For RSV

Norbert Pardi, Vaccines Group Lead, Penn Institute for RNA Innovation, University of Pennsylvania
Scientists have long been trying to develop a vaccine for respiratory syncytial virus (RSV), and it looks like Pfizer are closing in on this goal, based on the latest clinical trial data in newborns which they released in November. Pfizer have developed a protein-based vaccine against the F protein of RSV, which they are giving to pregnant women. It turns out that it induces a robust immune response after the administration of a single shot and it seems to be highly protective in newborns. The efficacy was over 80% after 90 days, so it protected very well against severe disease, and even though this dropped a little after six month, it was still pretty high.
I think this has been a very important breakthrough, and very timely at the moment with both COVID-19, influenza and RSV circulating, which just shows the importance of having a vaccine which works well in both the very young and the very old.
The road to an RSV vaccine has also illustrated the importance of teamwork in 21st century vaccine development. You need people with different backgrounds to solve these challenges – microbiologists, immunologists and structural biologists working together to understand how viruses work, and how our immune system induces protective responses against certain viruses. It has been this kind of teamwork which has yielded the findings that targeting the prefusion stabilized form of the F protein in RSV induces much stronger and highly protective immune responses.
Gene therapy shows its potential

Nicole Paulk, Assistant Professor of Gene Therapy at the University of California, San Francisco
The recent US Food and Drug Administration (FDA) approval of Hemgenix, a gene therapy for hemophilia B, is big for a lot of reasons. While hemophilia is absolutely a rare disease, it is astronomically more common than the first two approvals – Luxturna for RPE65-meidated inherited retinal dystrophy and Zolgensma for spinal muscular atrophy - so many more patients will be treated with this. In terms of numbers of patients, we are now starting to creep up into things that are much more common, which is a huge step in terms of our ability to scale the production of an adeno-associated virus (AAV) vector for gene therapy.
Hemophilia is also a really special patient population because this has been the darling indication for AAV gene therapy for the last 20 to 30 years. AAV trafficks to the liver so well, it’s really easy for us to target the tissues that we want. If you look at the numbers, there have been more gene therapy scientists working on hemophilia than any other condition. There have just been thousands and thousands of us working on gene therapy indications for the last 20 or 30 years, so to see the first of these approvals make it, feels really special.
I am sure it is even more special for the patients because now they have a choice – do I want to stay on my recombinant factor drug that I need to take every day for the rest of my life, or right now I could get a one-time infusion of this virus and possibly experience curative levels of expression for the rest of my life. And this is just the first one for hemophilia, there’s going to end up being a dozen gene therapies within the next five years, targeted towards different hemophilias.
Every single approval is momentous for the entire field because it gets investors excited, it gets companies and physicians excited, and that helps speed things up. Right now, it's still a challenge to produce enough for double digit patients. But with more interest comes the experiments and trials that allow us to pick up the knowledge to scale things up, so that we can go after bigger diseases like diabetes, congestive heart failure, cancer, all of these much bigger afflictions.
Treating Thickened Hearts

John Spertus, Professor in Metabolic and Vascular Disease Research, UMKC School of Medicine
Hypertrophic cardiomyopathy (HCM) is a disease that causes your heart muscle to enlarge, and the walls of your heart chambers thicken and reduce in size. Because of this, they cannot hold as much blood and may stiffen, causing some sufferers to experience progressive shortness of breath, fatigue and ultimately heart failure.
So far we have only had very crude ways of treating it, using beta blockers, calcium channel blockers or other medications which cause the heart to beat less strongly. This works for some patients but a lot of time it does not, which means you have to consider removing part of the wall of the heart with surgery.
Earlier this year, a trial of a drug called mavacamten, became the first study to show positive results in treating HCM. What is remarkable about mavacamten is that it is directed at trying to block the overly vigorous contractile proteins in the heart, so it is a highly targeted, focused way of addressing the key problem in these patients. The study demonstrated a really large improvement in patient quality of life where they were on the drug, and when they went off the drug, the quality of life went away.
Some specialists are now hypothesizing that it may work for other cardiovascular diseases where the heart either beats too strongly or it does not relax well enough, but just having a treatment for HCM is a really big deal. For years we have not been very aggressive in identifying and treating these patients because there have not been great treatments available, so this could lead to a new era.
Regenerating Organs

David Andrijevic, Associate Research Scientist in neuroscience at Yale School of Medicine
As soon as the heartbeat stops, a whole chain of biochemical processes resulting from ischemia – the lack of blood flow, oxygen and nutrients – begins to destroy the body’s cells and organs. My colleagues and I at Yale School of Medicine have been investigating whether we can recover organs after prolonged ischemia, with the main goal of expanding the organ donor pool.
Earlier this year we published a paper in which we showed that we could use technology to restore blood circulation, other cellular functions and even heart activity in pigs, one hour after their deaths. This was done using a perfusion technology to substitute heart, lung and kidney function, and deliver an experimental cell protective fluid to these organs which aimed to stop cell death and aid in the recovery.
One of the aims of this technology is that it can be used in future to lengthen the time window for recovering organs for donation after a person has been declared dead, a logistical hurdle which would allow us to substantially increase the donor pool. We might also be able to use this cell protective fluid in studies to see if it can help people who have suffered from strokes and myocardial infarction. In future, if we managed to achieve an adequate brain recovery – and the brain, out of all the organs, is the most susceptible to ischemia – this might also change some paradigms in resuscitation medicine.
Antibody-Drug Conjugates for Cancer

Yosi Shamay, Cancer Nanomedicine and Nanoinformatics researcher at the Technion Israel Institute of Technology
For the past four or five years, antibody-drug conjugates (ADCs) - a cancer drug where you have an antibody conjugated to a toxin - have been used only in patients with specific cancers that display high expression of a target protein, for example HER2-positive breast cancer. But in 2022, there have been clinical trials where ADCs have shown remarkable results in patients with low expression of HER2, which is something we never expected to see.
In July 2022, AstraZeneca published the results of a clinical trial, which showed that an ADC called trastuzumab deruxtecan can offer a very big survival benefit to breast cancer patients with very little expression of HER2, levels so low that they would be borderline undetectable for a pathologist. They got a strong survival signal for patients with very aggressive, metastatic disease.
I think this is very interesting and important because it means that it might pave the way to include more patients in clinical trials looking at ADCs for other cancers, for example lymphoma, colon cancer, lung cancers, even if they have low expression of the protein target. It also holds implications for CAR-T cells - where you genetically engineer a T cell to attack the cancer - because the concept is very similar. If we now know that an ADC can have a survival benefit, even in patients with very low target expression, the same might be true for T cells.
Look back further: Breakthroughs of 2021
https://leaps.org/6-biotech-breakthroughs-of-2021-that-missed-the-attention-they-deserved/
Repairing Cells and Longevity Myths with Dr. Charles Brenner
Charles Brenner, a leading biochemist at City of Hope National Medical Center in L.A., discovered a vitamin precursor called NR that seems to enable repair of cellular damage that happens as we get older.
Meet Charles Brenner, the Longevity Skeptic. Brenner, a leading biochemist at City of Hope National Medical Center in L.A., has been attending the largest longevity conferences with one main purpose: to point out that some of the other speakers are full of it.
Brenner is "throwing cold water" on several scientists in the field of aging, accusing them of hyping various fountains of youth, despite limited evidence for these therapies.
In this podcast episode, Brenner sat down with Leaps.org to discuss his groundbreaking work on metabolism and his efforts to counter what he considers to be bad science.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
In addition to bringing his candor to conferences, Brenner is applying it in academic journals, publishing a paper in September, "A Science-Based Review of the World's Best-Selling Book on Aging," in which he pans the author of this bestseller, David Sinclair, a Harvard biologist, for talking up the potential for humans to live far past 100. These aspirations may sound nice, but they're not backed by science, Brenner says. He's had high-profile debates online with Sinclair and Aubrey de Grey, a prominent biomedical gerontologist.
Meanwhile, in his own lab work, Brenner is credited with identifying a vitamin precursor called NR that seems to enable repair of cellular damage that happens as we get older - a major discovery that he's helped turn into a supplement, commercialized with a company called ChromaDex.
Whether it's possible to extend human lifespan is a pressing question as investments in longevity startups are projected to increase from $40 billion to $600 billion over the next three years. The field of biological aging seems split on the question of whether "anti-aging" therapies can significantly lengthen our natural lifespans, as Sinclair believes. Brenner, Morgan Levine of Altos Labs and Matt Kaeberlein of the University of Washington have argued that the only realistic goal is to extend one's window of healthy years, or healthspan, rather than trying to break the biological ceiling of our species.
Brenner is an intriguing figure in these debates. Although he’s been introduced in public appearances as a longevity skeptic, he calls himself an optimist.
Links:
Charles Brenner, City of Hope
Charles Brenner on Twitter
Charles Brenner's debate with Aubrey de Grey
Brenner's paper, "A Science-Based Review of the World's Best-Selling Book on Aging"
Peter Attia's recent blog on NR supplements
Brad Stanfield's recent reaction to "David Sinclair vs Charles Brenner"
ChromaDex NR supplement

