Americans Fell for a Theranos-Style Scam 100 Years Ago. Will We Ever Learn?

Medical scams like Theranos are as American as America itself.
The huckster understands what people want – an easy route to good health -- and figures out just how to provide it as long as no one asks too many questions.
"Americans are very much prone to this sort of thinking: Give me a pill or give me a magical bean that can make me lose weight!"
The keys to success: Hoopla, fancy technology, and gullibility. And oh yes, one more thing: a blood sample. Well, lots and lots of blood samples. Every testing fee counts.
Sound familiar? It could be the story of the preternaturally persuasive Elizabeth Holmes, the disgraced founder of Theranos who stands accused of perpetrating a massive blood-testing fraud. But this is a different story from a different time, one that dates back 100 years but sounds almost like it could unfold on the front page of The Wall Street Journal today.
The main difference: Back then, watchdogs thought they'd be able to vanquish fake medicine and scam science. Fat chance, it turned out. It seems like we're more likely to lose-weight-quick than make much of a dent into quackery and health fraud.
Why? Have we learned anything at all over the past century? As we sweep into a new decade, experts says we're not as advanced as we'd like to think. But the fight against fraud and fakery continues.
Quackery: As American As America Itself
In the 17th century, British healers of questionable reputation got a new name -- "quack," from the Dutch word "quacksalver," which originally referred to someone who treats others with home remedies but developed a new meaning along the lines of "charlatan." And these quacks got a new place to sell their wares: the American colonies.
By 1692, a Boston newspaper advertised a patent medicine that promised to cure "the Griping of the Guts, and the Wind Cholick" and – for good measure – "preventeth that woeful Distemper of the Dry Belly Ach." A couple centuries later, the most famous woman in the United States wasn't a first lady or feminist but a hawker of nostrums named Lydia Estes Pinkham whose "vegetable compound" promised to banish "female complaints." One advertisement suggested that the "sure cure" would have saved the life of a Connecticut clergyman whose wife killed him after suffering from feminine maladies for 16 years.
By the early 20th century, Americans were fascinated by electricity and radiation, and both healers and hucksters embraced the new high-tech era. Men with flagging libidos, for example, could irradiate their private parts with the radioactive Radiendocrinator or buy battery-powered electric belts equipped with dangling bits to supercharge their, um, dangling bits.
The Rise of the Radio Wave 'Cure'
Enter radionics, the (supposed) science of better health via radio waves. The idea was that "healthy people radiate healthy energy," and sickness could be reversed through diagnosis and re-tuning, write Dr. Lydia Kang and Nate Pedersen in their 2017 book "Quackery: A Brief History of the Worst Ways to Cure Everything."
Detecting illness and fixing it required machinery -- Dynamizers, Radioclasts and Oscillocasts – that could cost hundreds of dollars each. Thousands of physicians bought them. Fortunately, they could work remotely, for a fee. The worried-and-potentially-unwell just needed to send a blood sample and, of course, a personal check.
Sting operations revealed radionics to be bogus. A skeptic sent a blood sample to one radionics practitioner in Albuquerque who reported back with news of an infected fallopian tube. In fact, the blood sample came from a male guinea pig. As an American Medical Association leader reported, the guinea pig "had shown no female characteristics up to that time, and a postmortem examination yielded no evidence of ladylike attributes."
When Quackery Refused to Yield
The rise of bogus medical technology in the early 20th century spawned a watchdog industry as organizations like the American Medical Association swept into action, said medical historian Eric Boyle, author of 2012's "Quack Medicine: A History of Combating Health Fraud in Twentieth-Century America."
"When quackery was recognized as a major problem, the people who campaigned for its demise were confident that they could get rid of it," he said. "A lot of people believed that increased education, the truths of science, and laws designed to protect consumers would ultimately drive quackery from the marketplace. And then throughout the century, as modern medicine developed, and more effectively treated one disease after another, many observers remained confident in that prediction."
There's a bid to "flood the information highway with truth to turn the storm of fake promotional stuff into a trickle."
But fake medicine persisted as Americans continued their quest to get- healthy-quick… or get-rich-quick by promising to help others to get- healthy-quick. Even radionics refused to die. It's still around in various forms. And, as the Theranos scandal reveals, we're still hoping our blood can offer the keys to longevity and good health.
Why Do We Still Fall for Scams?
In our own era, the Theranos company rose to prominence when founder and CEO Elizabeth Holmes convinced journalists and investors that she'd found a way to cheaply test drops of blood for hundreds of conditions. Then it all fell apart, famously, when the world learned that the technology didn't work. The company has folded, and Holmes faces a federal trial on fraud charges this year.
"There were a lot of prominent, very smart people who bought into the myth of Elizabeth Holmes," a former employee told "60 Minutes," even though the blood tests never actually worked as advertised.
Shouldn't "prominent, very smart people" know better? "People are gullible," said Dr. Stephen Barrett, a psychiatrist and leading quack-buster who runs the QuackWatch website. But there's more to the story. According to him, we're uniquely vulnerable as individuals to bogus medicine.
Scam artists specifically pinpoint their target audiences, such as "smart people," desperate people and alienated people, he said.
Smart people, for example, might be overconfident about their ability to detect fraud and fall for bogus medicine. Alienated people may distrust the establishment, whether it's the medical field or government watchdogs, and be more receptive to alternative sources of information.
Dr. Barrett also points a finger at magical thinking, which comes in different forms. It could mean a New Age-style belief that our minds can control the world around us. Or, as professional quack-buster Alex Berezow said, it could refer to "our cultural obsession with quick fixes."
"Americans are very much prone to this sort of thinking: Give me a pill or give me a magical bean that can make me lose weight! But complex problems need complex solutions," said Berezow, a microbiologist who debunks junk science in his job as a spokesman for the American Council on Science & Health.
American mistrust of expertise makes matters worse, he said. "When I tell people they need to get vaccinated, I'm called a shill for the pharmaceutical industry," he said. "If I say dietary supplements generally don't work, I'm a shill for doctors who want to keep people sick."
What can ordinary citizens do to protect themselves from fake medicine? "You have to have a healthy skepticism of everything," Berezow said. "When you come across something new, is someone trying to take advantage of you? It's a horrible way to think about the world, but there's some truth to it."
"Like any chronic disease, we will have to live with it while we do our best to fight it."
The government and experts have their own roles to play via regulation and education, respectively. For all the criticism it gets, the Food & Drug Administration does serve as a bulwark against fakery in prescription medicine. And while celebrities like Gwyneth "Goop" Paltrow hawk countless questionable medical products on the Internet, scientists and physicians are fighting back by using social media as a tool to promote the truth. There's a bid to "flood the information highway with truth to turn the storm of fake promotional stuff into a trickle," said Dr. Randi Hutter Epstein, a writer in residence at Yale School of Medicine and author of 2018's "Aroused: The History of Hormones and How They Control Just About Everything."
What's next? Like death, taxes and Cher, charlatans are likely to always be with us. Boyle quoted the late William Jarvis, a pioneering quack-buster in the late 20th century who believed health fraud would never be eradicated: "Like any chronic disease, we will have to live with it while we do our best to fight it."
The Friday Five: How to exercise for cancer prevention
How to exercise for cancer prevention. Plus, a device that brings relief to back pain, ingredients for reducing Alzheimer's risk, the world's oldest disease could make you young again, and more.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Here are the promising studies covered in this week's Friday Five:
- How to exercise for cancer prevention
- A device that brings relief to back pain
- Ingredients for reducing Alzheimer's risk
- Is the world's oldest disease the fountain of youth?
- Scared of crossing bridges? Your phone can help
New approach to brain health is sparking memories
This fall, Robert Reinhart of Boston University published a study finding that electrical stimulation can boost memory - and Reinhart was surprised to discover the effects lasted a full month.
What if a few painless electrical zaps to your brain could help you recall names, perform better on Wordle or even ward off dementia?
This is where neuroscientists are going in efforts to stave off age-related memory loss as well as Alzheimer’s disease. Medications have shown limited effectiveness in reversing or managing loss of brain function so far. But new studies suggest that firing up an aging neural network with electrical or magnetic current might keep brains spry as we age.
Welcome to non-invasive brain stimulation (NIBS). No surgery or anesthesia is required. One day, a jolt in the morning with your own battery-operated kit could replace your wake-up coffee.
Scientists believe brain circuits tend to uncouple as we age. Since brain neurons communicate by exchanging electrical impulses with each other, the breakdown of these links and associations could be what causes the “senior moment”—when you can’t remember the name of the movie you just watched.
In 2019, Boston University researchers led by Robert Reinhart, director of the Cognitive and Clinical Neuroscience Laboratory, showed that memory loss in healthy older adults is likely caused by these disconnected brain networks. When Reinhart and his team stimulated two key areas of the brain with mild electrical current, they were able to bring the brains of older adult subjects back into sync — enough so that their ability to remember small differences between two images matched that of much younger subjects for at least 50 minutes after the testing stopped.
Reinhart wowed the neuroscience community once again this fall. His newer study in Nature Neuroscience presented 150 healthy participants, ages 65 to 88, who were able to recall more words on a given list after 20 minutes of low-intensity electrical stimulation sessions over four consecutive days. This amounted to a 50 to 65 percent boost in their recall.
Even Reinhart was surprised to discover the enhanced performance of his subjects lasted a full month when they were tested again later. Those who benefited most were the participants who were the most forgetful at the start.

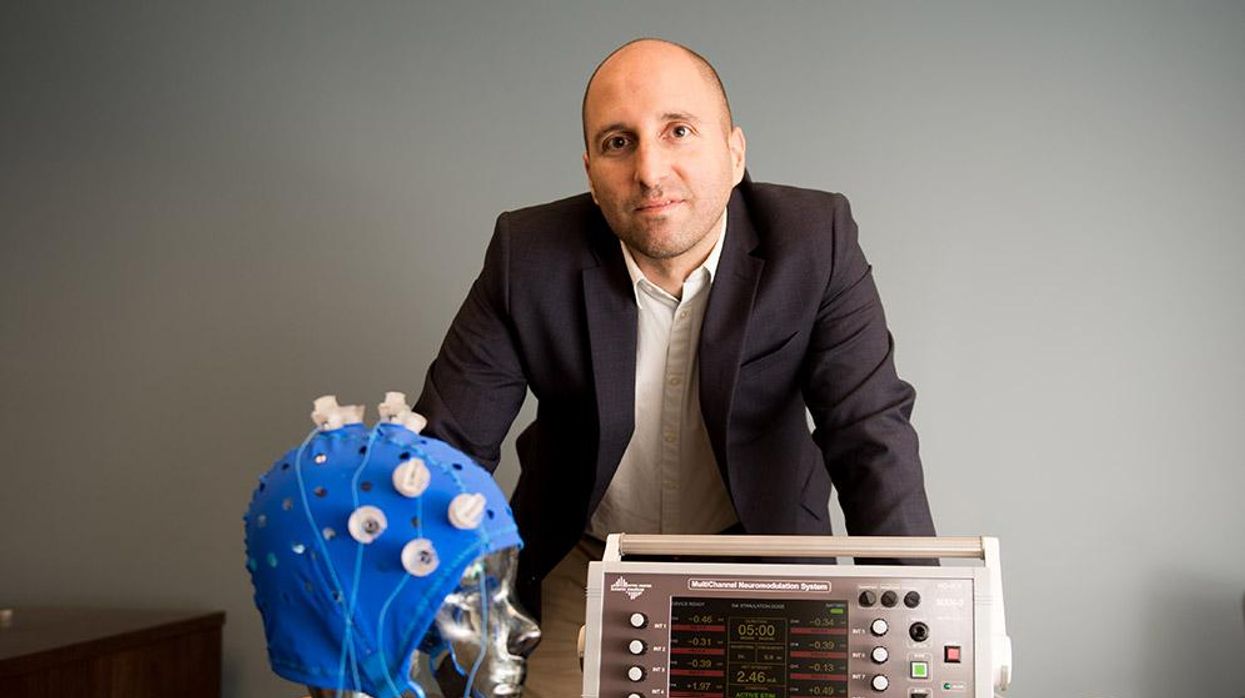
An older person participates in Robert Reinhart's research on brain stimulation.
Robert Reinhart
Reinhart’s subjects only suffered normal age-related memory deficits, but NIBS has great potential to help people with cognitive impairment and dementia, too, says Krista Lanctôt, the Bernick Chair of Geriatric Psychopharmacology at Sunnybrook Health Sciences Center in Toronto. Plus, “it is remarkably safe,” she says.
Lanctôt was the senior author on a meta-analysis of brain stimulation studies published last year on people with mild cognitive impairment or later stages of Alzheimer’s disease. The review concluded that magnetic stimulation to the brain significantly improved the research participants’ neuropsychiatric symptoms, such as apathy and depression. The stimulation also enhanced global cognition, which includes memory, attention, executive function and more.
This is the frontier of neuroscience.
The two main forms of NIBS – and many questions surrounding them
There are two types of NIBS. They differ based on whether electrical or magnetic stimulation is used to create the electric field, the type of device that delivers the electrical current and the strength of the current.
Transcranial Current Brain Stimulation (tES) is an umbrella term for a group of techniques using low-wattage electrical currents to manipulate activity in the brain. The current is delivered to the scalp or forehead via electrodes attached to a nylon elastic cap or rubber headband.
Variations include how the current is delivered—in an alternating pattern or in a constant, direct mode, for instance. Tweaking frequency, potency or target brain area can produce different effects as well. Reinhart’s 2022 study demonstrated that low or high frequencies and alternating currents were uniquely tied to either short-term or long-term memory improvements.
Sessions may be 20 minutes per day over the course of several days or two weeks. “[The subject] may feel a tingling, warming, poking or itching sensation,” says Reinhart, which typically goes away within a minute.
The other main approach to NIBS is Transcranial Magnetic Simulation (TMS). It involves the use of an electromagnetic coil that is held or placed against the forehead or scalp to activate nerve cells in the brain through short pulses. The stimulation is stronger than tES but similar to a magnetic resonance imaging (MRI) scan.
The subject may feel a slight knocking or tapping on the head during a 20-to-60-minute session. Scalp discomfort and headaches are reported by some; in very rare cases, a seizure can occur.
No head-to-head trials have been conducted yet to evaluate the differences and effectiveness between electrical and magnetic current stimulation, notes Lanctôt, who is also a professor of psychiatry and pharmacology at the University of Toronto. Although TMS was approved by the FDA in 2008 to treat major depression, both techniques are considered experimental for the purpose of cognitive enhancement.
“One attractive feature of tES is that it’s inexpensive—one-fifth the price of magnetic stimulation,” Reinhart notes.
Don’t confuse either of these procedures with the horrors of electroconvulsive therapy (ECT) in the 1950s and ‘60s. ECT is a more powerful, riskier procedure used only as a last resort in treating severe mental illness today.
Clinical studies on NIBS remain scarce. Standardized parameters and measures for testing have not been developed. The high heterogeneity among the many existing small NIBS studies makes it difficult to draw general conclusions. Few of the studies have been replicated and inconsistencies abound.
Scientists are still lacking so much fundamental knowledge about the brain and how it works, says Reinhart. “We don’t know how information is represented in the brain or how it’s carried forward in time. It’s more complex than physics.”
Lanctôt’s meta-analysis showed improvements in global cognition from delivering the magnetic form of the stimulation to people with Alzheimer’s, and this finding was replicated inan analysis in the Journal of Prevention of Alzheimer’s Disease this fall. Neither meta-analysis found clear evidence that applying the electrical currents, was helpful for Alzheimer’s subjects, but Lanctôt suggests this might be merely because the sample size for tES was smaller compared to the groups that received TMS.
At the same time, London neuroscientist Marco Sandrini, senior lecturer in psychology at the University of Roehampton, critically reviewed a series of studies on the effects of tES on episodic memory. Often declining with age, episodic memory relates to recalling a person’s own experiences from the past. Sandrini’s review concluded that delivering tES to the prefrontal or temporoparietal cortices of the brain might enhance episodic memory in older adults with Alzheimer’s disease and amnesiac mild cognitive impairment (the predementia phase of Alzheimer’s when people start to have symptoms).
Researchers readily tick off studies needed to explore, clarify and validate existing NIBS data. What is the optimal stimulus session frequency, spacing and duration? How intense should the stimulus be and where should it be targeted for what effect? How might genetics or degree of brain impairment affect responsiveness? Would adjunct medication or cognitive training boost positive results? Could administering the stimulus while someone sleeps expedite memory consolidation?
Using MRI or another brain scan along with computational modeling of the current flow, a clinician could create a treatment that is customized to each person’s brain.
While Sandrini’s review reported improvements induced by tES in the recall or recognition of words and images, there is no evidence it will translate into improvements in daily activities. This is another question that will require more research and testing, Sandrini notes.
Scientists are still lacking so much fundamental knowledge about the brain and how it works, says Reinhart. “We don’t know how information is represented in the brain or how it’s carried forward in time. It’s more complex than physics.”
Where the science is headed
Learning how to apply precision medicine to NIBS is the next focus in advancing this technology, says Shankar Tumati, a post-doctoral fellow working with Lanctôt.
There is great variability in each person’s brain anatomy—the thickness of the skull, the brain’s unique folds, the amount of cerebrospinal fluid. All of these structural differences impact how electrical or magnetic stimulation is distributed in the brain and ultimately the effects.
Using MRI or another brain scan along with computational modeling of the current flow, a clinician could create a treatment that is customized to each person’s brain, from where to put the electrodes to determining the exact dose and duration of stimulation needed to achieve lasting results, Sandrini says.
Above all, most neuroscientists say that largescale research studies over long periods of time are necessary to confirm the safety and durability of this therapy for the purpose of boosting memory. Short of that, there can be no FDA approval or medical regulation for this clinical use.
Lanctôt urges people to seek out clinical NIBS trials in their area if they want to see the science advance. “That is how we’ll find the answers,” she says, predicting it will be 5 to 10 years to develop each additional clinical application of NIBS. Ultimately, she predicts that reigning in Alzheimer’s disease and mild cognitive impairment will require a multi-pronged approach that includes lifestyle and medications, too.
Sandrini believes that scientific efforts should focus on preventing or delaying Alzheimer’s. “We need to start intervention earlier—as soon as people start to complain about forgetting things,” he says. “Changes in the brain start 10 years before [there is a problem]. Once Alzheimer’s develops, it is too late.”