An Astounding Treatment at an Astounding Price: Who Gets to Benefit?

Tony and Kelly Mantoan, with their boys Teddy and Fulton, who both suffer from SMA, a genetic disorder that makes walking, swallowing, and breathing progressively difficult.
Kelly Mantoan was nursing her newborn son, Teddy, in the NICU in a Philadelphia hospital when her doctor came in and silently laid a hand on her shoulder. Immediately, Kelly knew what the gesture meant and started to sob: Teddy, like his one-year-old brother, Fulton, had just tested positive for a neuromuscular condition called spinal muscular atrophy (SMA).
The boys were 8 and 10 when Kelly heard about an experimental new treatment, still being tested in clinical trials, called Spinraza.
"We knew that [SMA] was a genetic disorder, and we knew that we had a 1 in 4 chance of Teddy having SMA," Mantoan recalls. But the idea of having two children with the same severe disability seemed too unfair for Kelly and her husband, Tony, to imagine. "We had lots of well-meaning friends tell us, well, God won't do this to you twice," she says. Except that He, or a cruel trick of nature, had.
In part, the boys' diagnoses were so devastating because there was little that could be done at the time, back in 2009 and 2010, when the boys were diagnosed. Affecting an estimated 1 in 11,000 babies, SMA is a degenerative disease in which the body is deficient in survival motor neuron (SMN) protein, thanks to a genetic mutation or absence of the body's SNM1 gene. So muscles that control voluntary movement – such as walking, breathing, and swallowing – weaken and eventually cease to function altogether.
Babies diagnosed with SMA Type 1 rarely live past toddlerhood, while people diagnosed with SMA Types 2, 3, and 4 can live into adulthood, usually with assistance like ventilators and feeding tubes. Shortly after birth, both Teddy Mantoan and his brother, Fulton, were diagnosed with SMA Type 2.
The boys were 8 and 10 when Kelly heard about an experimental new treatment, still being tested in clinical trials, called Spinraza. Up until then, physical therapy was the only sanctioned treatment for SMA, and Kelly enrolled both her boys in weekly sessions to preserve some of their muscle strength as the disease marched forward. But Spinraza – a grueling regimen of lumbar punctures and injections designed to stimulate a backup survival motor neuron gene to produce more SMN protein – offered new hope.
In clinical trials, after just a few doses of Spinraza, babies with SMA Type 1 began meeting normal developmental milestones – holding up their heads, rolling over, and sitting up. In other trials, Spinraza treatment delayed the need for permanent ventilation, while patients on the placebo arm continued to lose function, and several died. Spinraza was such a success, and so well tolerated among patients, that clinical trials ended early and the drug was fast-tracked for FDA approval in 2016. In January 2017, when Kelly got the call that Fulton and Teddy had been approved by the hospital to start Spinraza infusions, Kelly dropped to her knees in the middle of the kitchen and screamed.
Spinraza, manufactured by Biogen, has been hailed as revolutionary, but it's also not without drawbacks: Priced per injection, just one dose of Spinraza costs $125,000, making it one of the most expensive drugs on the global market. What's worse, treatment requires a "loading dose" of four injections over a four-week period, and then periodic injections every four months, indefinitely. For the first year of treatment, Spinraza treatment costs $750,000 – and then $375,000 for every year thereafter.
Last week, a competitive treatment for SMA Type 1 manufactured by Novartis burst onto the market. The new treatment, called Zolgensma, is a one-time gene therapy intended to be given to infants and is currently priced at $2.125 million, or $425,000 annually for five years, making it the most expensive drug in the world. Like Spinraza, Zolgensma is currently raising challenging questions about how insurers and government payers like Medicaid will be able to afford these treatments without bankrupting an already-strained health care system.
To Biogen's credit, the company provides financial aid for Spinraza patients with private insurance who pay co-pays for treatment, as well as for those who have been denied by Medicaid and Medicare. But getting insurance companies to agree to pay for Spinraza can often be an ordeal in itself. Although Fulton and Teddy Mantoan were approved for treatment over two years ago, a lengthy insurance battle delayed treatment for another eight months – time that, for some SMA patients, can mean a significant loss of muscular function.
Kelly didn't notice anything in either boy – positive or negative – for the first few months of Spinraza injections. But one day in November 2017, as Teddy was lowered off his school bus in his wheelchair, he turned to say goodbye to his friends and "dab," – a dance move where one's arms are extended briefly across the chest and in the air. Normally, Teddy would dab by throwing his arms up in the air with momentum, striking a pose quickly before they fell down limp at his sides. But that day, Teddy held his arms rigid in the air. His classmates, along with Kelly, were stunned. "Teddy, look at your arms!" Kelly remembers shrieking. "You're holding them up – you're dabbing!"

Teddy and Fulton Mantoan, who both suffer from spinal muscular atrophy, have seen life-changing results from Spinraza.
(Courtesy of Kelly Mantoan)
Not long after Teddy's dab, the Mantoans started seeing changes in Fulton as well. "With Fulton, we realized suddenly that he was no longer choking on his food during meals," Kelly said. "Almost every meal we'd have to stop and have him take a sip of water and make him slow down and take small bites so he wouldn't choke. But then we realized we hadn't had to do that in a long time. The nurses at school were like, 'it's not an issue anymore.'"
For the Mantoans, this was an enormous relief: Less choking meant less chance of aspiration pneumonia, a leading cause of death for people with SMA Types 1 and 2.
While Spinraza has been life-changing for the Mantoans, it remains painfully out of reach for many others. Thanks to Spinraza's enormous price tag, the threshold for who gets to use it is incredibly high: Adult and pediatric patients, particularly those with state-sponsored insurance, have reported multiple insurance denials, lengthy appeals processes, and endless bureaucracy from insurance and hospitals alike that stand in the way of treatment.
Kate Saldana, a 21-year-old woman with Type 2 SMA, is one of the many adult patients who have been lobbying for the drug. Saldana, who uses a ventilator 20 hours each day, says that Medicaid denied her Spinraza treatments because they mistakenly believed that she used a ventilator full-time. Saldana is currently in the process of appealing their decision, but knows she is fighting an uphill battle.

Kate Saldana, who suffers from Type 2 SMA, has been fighting unsuccessfully for Medicaid to cover Spinraza.
(Courtesy of Saldana)
"Originally, the treatments were studied and created for infants and children," Saldana said in an e-mail. "There is a plethora of data to support the effectiveness of Spinraza in those groups, but in adults it has not been studied as much. That makes it more difficult for insurance to approve it, because they are not sure if it will be as beneficial."
Saldana has been pursuing treatment unsuccessfully since last August – but others, like Kimberly Hill, a 32-year-old with SMA Type 2, have been waiting even longer. Hill, who lives in Oklahoma, has been fighting for treatment since Spinraza went on the U.S. market in December 2016. Because her mobility is limited to the use of her left thumb, Hill is eager to try anything that will enable her to keep working and finish a Master's degree in Fire and Emergency Management.
"Obviously, my family and I were elated with the approval of Spinraza," Hill said in an e-mail. "We thought I would finally have the chance to get a little stronger and healthier." But with Medicare and Medicaid, coverage and eligibility varies wildly by state. Earlier this year, Medicaid approved Spinraza for adult patients only if a clawback clause was attached to the approval, meaning that under certain conditions the Medicaid funds would need to be paid back. Because of the clawback clause, hospitals have been reluctant to take on Spinraza treatments, effectively barring adult Medicaid patients from accessing the drug altogether.
Hill's hospital is currently in negotiations with Medicaid to move forward with Spinraza treatment, but in the meantime, Hill is in limbo. "We keep being told there is nothing we can do, and we are devastated," Hill said.
"I felt extremely sad and honestly a bit forgotten, like adults [with SMA] don't matter."
Between Spinraza and its new competitor, Zolgensma, some are speculating that insurers will start to favor Zolgensma coverage instead, since the treatment is shorter and ultimately cheaper than Spinraza in the long term. But for some adults with SMA who can't access Spinraza and who don't qualify for Zolgensma treatment, the issue of what insurers will cover is moot.
"I was so excited when I heard that Zolgensma was approved by the FDA," said Annie Wilson, an adult SMA patient from Alameda, Calif. who has been fighting for Spinraza since 2017. "When I became aware that it was only being offered to children, I felt extremely sad and honestly a bit forgotten, like adults [with SMA] don't matter."
According to information from a Biogen representative, more than 7500 people worldwide have been treated with Spinraza to date, one third of whom are adults.
While Spinraza has been revolutionary for thousands of patients, it's unclear how many more lives state agencies and insurance companies will allow it to save.
Recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen as soon as 18 months from now
Like all those whose kidneys have failed, Scott Burton’s life revolves around dialysis. For nearly two decades, Burton has been hooked up (or, since 2020, has hooked himself up at home) to a dialysis machine that performs the job his kidneys normally would. The process is arduous, time-consuming, and expensive. Except for a brief window before his body rejected a kidney transplant, Burton has depended on machines to take the place of his kidneys since he was 12-years-old. His whole life, the 39-year-old says, revolves around dialysis.
“Whenever I try to plan anything, I also have to plan my dialysis,” says Burton says, who works as a freelance videographer and editor. “It’s a full-time job in itself.”
Many of those on dialysis are in line for a kidney transplant that would allow them to trade thrice-weekly dialysis and strict dietary limits for a lifetime of immunosuppressants. Burton’s previous transplant means that his body will likely reject another donated kidney unless it matches perfectly—something he’s not counting on. It’s why he’s enthusiastic about the development of artificial kidneys, small wearable or implantable devices that would do the job of a healthy kidney while giving users like Burton more flexibility for traveling, working, and more.
Still, the devices aren’t ready for testing in humans—yet. But recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen as soon as 18 months from now, according to Jonathan Himmelfarb, a nephrologist at the University of Washington.
“It would liberate people with kidney failure,” Himmelfarb says.
An engineering marvel
Compared to the heart or the brain, the kidney doesn’t get as much respect from the medical profession, but its job is far more complex. “It does hundreds of different things,” says UCLA’s Ira Kurtz.
Kurtz would know. He’s worked as a nephrologist for 37 years, devoting his career to helping those with kidney disease. While his colleagues in cardiology and endocrinology have seen major advances in the development of artificial hearts and insulin pumps, little has changed for patients on hemodialysis. The machines remain bulky and require large volumes of a liquid called dialysate to remove toxins from a patient’s blood, along with gallons of purified water. A kidney transplant is the next best thing to someone’s own, functioning organ, but with over 600,000 Americans on dialysis and only about 100,000 kidney transplants each year, most of those in kidney failure are stuck on dialysis.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. Each of the 45 different cell types in the kidney do something different.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. To build an artificial heart, Kurtz says, you basically need to engineer a pump. An artificial pancreas needs to balance blood sugar levels with insulin secretion. While neither of these tasks is simple, they are fairly straightforward. The kidney, on the other hand, does more than get rid of waste products like urea and other toxins. Each of the 45 different cell types in the kidney do something different, helping to regulate electrolytes like sodium, potassium, and phosphorous; maintaining blood pressure and water balance; guiding the body’s hormonal and inflammatory responses; and aiding in the formation of red blood cells.

There's been little progress for patients during Ira Kurtz's 37 years as a nephrologist. Artificial kidneys would change that.
UCLA
Dialysis primarily filters waste, and does so well enough to keep someone alive, but it isn’t a true artificial kidney because it doesn’t perform the kidney’s other jobs, according to Kurtz, such as sensing levels of toxins, wastes, and electrolytes in the blood. Due to the size and water requirements of existing dialysis machines, the equipment isn’t portable. Physicians write a prescription for a certain duration of dialysis and assess how well it’s working with semi-regular blood tests. The process of dialysis itself, however, is conducted blind. Doctors can’t tell how much dialysis a patient needs based on kidney values at the time of treatment, says Meera Harhay, a nephrologist at Drexel University in Philadelphia.
But it’s the impact of dialysis on their day-to-day lives that creates the most problems for patients. Only one-quarter of those on dialysis are able to remain employed (compared to 85% of similar-aged adults), and many report a low quality of life. Having more flexibility in life would make a major different to her patients, Harhay says.
“Almost half their week is taken up by the burden of their treatment. It really eats away at their freedom and their ability to do things that add value to their life,” she says.
Art imitates life
The challenge for artificial kidney designers was how to compress the kidney’s natural functions into a portable, wearable, or implantable device that wouldn’t need constant access to gallons of purified and sterilized water. The other universal challenge they faced was ensuring that any part of the artificial kidney that would come in contact with blood was kept germ-free to prevent infection.
As part of last year’s KidneyX Prize, a partnership between the U.S. Department of Health and Human Services and the American Society of Nephrology, inventors were challenged to create prototypes for artificial kidneys. Himmelfarb’s team at the University of Washington’s Center for Dialysis Innovation won the prize by focusing on miniaturizing existing technologies to create a portable dialysis machine. The backpack sized AKTIV device (Ambulatory Kidney to Increase Vitality) will recycle dialysate in a closed loop system that removes urea from blood and uses light-based chemical reactions to convert the urea to nitrogen and carbon dioxide, which allows the dialysate to be recirculated.
Himmelfarb says that the AKTIV can be used when at home, work, or traveling, which will give users more flexibility and freedom. “If you had a 30-pound device that you could put in the overhead bins when traveling, you could go visit your grandkids,” he says.
Kurtz’s team at UCLA partnered with the U.S. Kidney Research Corporation and Arkansas University to develop a dialysate-free desktop device (about the size of a small printer) as the first phase of a progression that will he hopes will lead to something small and implantable. Part of the reason for the artificial kidney’s size, Kurtz says, is the number of functions his team are cramming into it. Not only will it filter urea from blood, but it will also use electricity to help regulate electrolyte levels in a process called electrodeionization. Kurtz emphasizes that these additional functions are what makes his design a true artificial kidney instead of just a small dialysis machine.
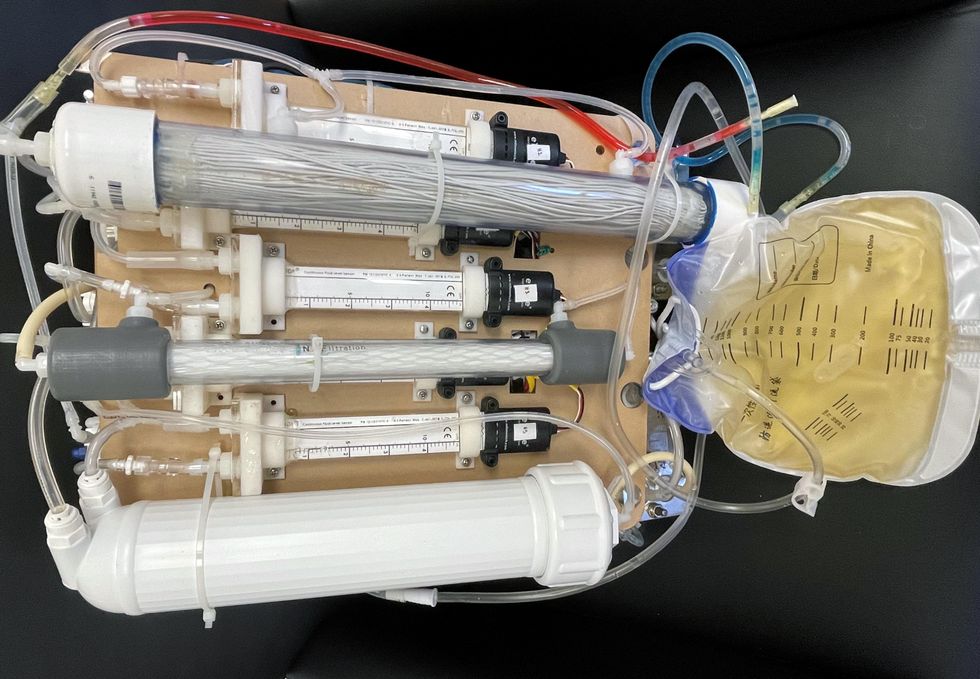
One version of an artificial kidney.
UCLA
“It doesn't have just a static function. It has a bank of sensors that measure chemicals in the blood and feeds that information back to the device,” Kurtz says.
Other startups are getting in on the game. Nephria Bio, a spinout from the South Korean-based EOFlow, is working to develop a wearable dialysis device, akin to an insulin pump, that uses miniature cartridges with nanomaterial filters to clean blood (Harhay is a scientific advisor to Nephria). Ian Welsford, Nephria’s co-founder and CTO, says that the device’s design means that it can also be used to treat acute kidney injuries in resource-limited settings. These potentials have garnered interest and investment in artificial kidneys from the U.S. Department of Defense.
For his part, Burton is most interested in an implantable device, as that would give him the most freedom. Even having a regular outpatient procedure to change batteries or filters would be a minor inconvenience to him.
“Being plugged into a machine, that’s not mimicking life,” he says.
Today’s more than 20,000 mental health apps have a wide range of functionalities and business models. Many of them can be useful for depression.
Even before the pandemic created a need for more telehealth options, depression was a hot area of research for app developers. Given the high prevalence of depression and its connection to suicidality — especially among today’s teenagers and young adults who grew up with mobile devices, use them often, and experience these conditions with alarming frequency — apps for depression could be not only useful but lifesaving.
“For people who are not depressed, but have been depressed in the past, the apps can be helpful for maintaining positive thinking and behaviors,” said Andrea K. Wittenborn, PhD, director of the Couple and Family Therapy Doctoral Program and a professor in human development and family studies at Michigan State University. “For people who are mildly to severely depressed, apps can be a useful complement to working with a mental health professional.”
Health and fitness apps, in general, number in the hundreds of thousands. These are driving a market expected to reach $102.45 billion by next year. The mobile mental health app market is a small part of this but still sizable at $500 million, with revenues generated through user health insurance, employers, and direct payments from individuals.
Apps can provide data that health professionals cannot gather on their own. People’s constant interaction with smartphones and wearable devices yields data on many health conditions for millions of patients in their natural environments and while they go about their usual activities. Compared with the in-office measurements of weight and blood pressure and the brevity of doctor-patient interactions, the thousands of data points gathered unobtrusively over an extended time period provide a far better and more detailed picture of the person and their health.
At their most advanced level, apps for mental health, including depression, passively gather data on how the user touches and interacts with the mobile device through changes in digital biomarkers that relate to depressive symptoms and other conditions.
Building on three decades of research since early “apps” were used for delivering treatment manuals to health professionals, today’s more than 20,000 mental health apps have a wide range of functionalities and business models. Many of these apps can be useful for depression.
Some apps primarily provide a virtual connection to a group of mental health professionals employed or contracted by the app. Others have options for meditation, sleeping or, in the case of industry leaders Calm and Headspace, overall well-being. On the cutting edge are apps that detect changes in a person’s use of mobile devices and their interactions with them.
Apps such as AbleTo, Happify Health, and Woebot Health focus on cognitive behavioral therapy, a type of counseling with proven potential to change a person’s behaviors and feelings. “CBT has been demonstrated in innumerable studies over the last several decades to be effective in the treatment of behavioral health conditions such as depression and anxiety disorders,” said Dr. Reena Pande, chief medical officer at AbleTo. “CBT is intended to be delivered as a structured intervention incorporating key elements, including behavioral activation and adaptive thinking strategies.”
These CBT skills help break the negative self-talk (rumination) common in patients with depression. They are taught and reinforced by some self-guided apps, using either artificial intelligence or programmed interactions with users. Apps can address loneliness and isolation through connections with others, even when a symptomatic person doesn’t feel like leaving the house.
At their most advanced level, apps for mental health, including depression, passively gather data on how the user touches and interacts with the mobile device through changes in “digital biomarkers” that can be associated with onset or worsening of depressive symptoms and other cognitive conditions. In one study, Mindstrong Health gathered a year’s worth of data on how people use their smartphones, such as scrolling through articles, typing and clicking. Mindstrong, whose founders include former leaders of the National Institutes of Health, modeled the timing and order of these actions to make assessments that correlated closely with gold-standard tests of cognitive function.
National organizations of mental health professionals have been following the expanding number of available apps over the years with keen interest. App Advisor is an initiative of the American Psychiatric Association that helps psychiatrists and other mental health professionals navigate the issues raised by mobile health technology. App Advisor does not rate or recommend particular apps but rather provides guidance about why apps should be assessed and how health professionals can do this.
A website that does review mental health apps is One Mind Psyber Guide, an independent nonprofit that partners with several national organizations. One Mind users can select among numerous search terms for the condition and therapeutic approach of interest. Apps are rated on a five-point scale, with reviews written by professionals in the field.
Do mental health apps related to depression have the kind of safety and effectiveness data required for medications and other medical interventions? Not always — and not often. Yet the overall results have shown early promise, Wittenborn noted.
“Studies that have attempted to detect depression from smartphone and wearable sensors [during a single session] have ranged in accuracy from about 86 to 89 percent,” Wittenborn said. “Studies that tried to predict changes in depression over time have been less accurate, with accuracy ranging from 59 to 85 percent.”
The Food and Drug Administration encourages the development of apps and has approved a few of them—mostly ones used by health professionals—but it is generally “hands off,” according to the American Psychiatric Association. The FDA has published a list of examples of software (including programming of apps) that it does not plan to regulate because they pose low risk to the public. First on the list is software that helps patients with diagnosed psychiatric conditions, including depression, maintain their behavioral coping skills by providing a “Skill of the Day” technique or message.
On its App Advisor site, the American Psychiatric Association says mental health apps can be dangerous or cause harm in multiple ways, such as by providing false information, overstating the app’s therapeutic value, selling personal data without clearly notifying users, and collecting data that isn’t relevant to mental health.
Although there is currently reason for caution, patients may eventually come to expect mental health professionals to recommend apps, especially as their rating systems, features and capabilities expand. Through such apps, patients might experience more and higher quality interactions with their mental health professionals. “Apps will continue to be refined and become more effective through future research,” said Wittenborn. “They will become more integrated into practice over time.”