An Astounding Treatment at an Astounding Price: Who Gets to Benefit?

Tony and Kelly Mantoan, with their boys Teddy and Fulton, who both suffer from SMA, a genetic disorder that makes walking, swallowing, and breathing progressively difficult.
Kelly Mantoan was nursing her newborn son, Teddy, in the NICU in a Philadelphia hospital when her doctor came in and silently laid a hand on her shoulder. Immediately, Kelly knew what the gesture meant and started to sob: Teddy, like his one-year-old brother, Fulton, had just tested positive for a neuromuscular condition called spinal muscular atrophy (SMA).
The boys were 8 and 10 when Kelly heard about an experimental new treatment, still being tested in clinical trials, called Spinraza.
"We knew that [SMA] was a genetic disorder, and we knew that we had a 1 in 4 chance of Teddy having SMA," Mantoan recalls. But the idea of having two children with the same severe disability seemed too unfair for Kelly and her husband, Tony, to imagine. "We had lots of well-meaning friends tell us, well, God won't do this to you twice," she says. Except that He, or a cruel trick of nature, had.
In part, the boys' diagnoses were so devastating because there was little that could be done at the time, back in 2009 and 2010, when the boys were diagnosed. Affecting an estimated 1 in 11,000 babies, SMA is a degenerative disease in which the body is deficient in survival motor neuron (SMN) protein, thanks to a genetic mutation or absence of the body's SNM1 gene. So muscles that control voluntary movement – such as walking, breathing, and swallowing – weaken and eventually cease to function altogether.
Babies diagnosed with SMA Type 1 rarely live past toddlerhood, while people diagnosed with SMA Types 2, 3, and 4 can live into adulthood, usually with assistance like ventilators and feeding tubes. Shortly after birth, both Teddy Mantoan and his brother, Fulton, were diagnosed with SMA Type 2.
The boys were 8 and 10 when Kelly heard about an experimental new treatment, still being tested in clinical trials, called Spinraza. Up until then, physical therapy was the only sanctioned treatment for SMA, and Kelly enrolled both her boys in weekly sessions to preserve some of their muscle strength as the disease marched forward. But Spinraza – a grueling regimen of lumbar punctures and injections designed to stimulate a backup survival motor neuron gene to produce more SMN protein – offered new hope.
In clinical trials, after just a few doses of Spinraza, babies with SMA Type 1 began meeting normal developmental milestones – holding up their heads, rolling over, and sitting up. In other trials, Spinraza treatment delayed the need for permanent ventilation, while patients on the placebo arm continued to lose function, and several died. Spinraza was such a success, and so well tolerated among patients, that clinical trials ended early and the drug was fast-tracked for FDA approval in 2016. In January 2017, when Kelly got the call that Fulton and Teddy had been approved by the hospital to start Spinraza infusions, Kelly dropped to her knees in the middle of the kitchen and screamed.
Spinraza, manufactured by Biogen, has been hailed as revolutionary, but it's also not without drawbacks: Priced per injection, just one dose of Spinraza costs $125,000, making it one of the most expensive drugs on the global market. What's worse, treatment requires a "loading dose" of four injections over a four-week period, and then periodic injections every four months, indefinitely. For the first year of treatment, Spinraza treatment costs $750,000 – and then $375,000 for every year thereafter.
Last week, a competitive treatment for SMA Type 1 manufactured by Novartis burst onto the market. The new treatment, called Zolgensma, is a one-time gene therapy intended to be given to infants and is currently priced at $2.125 million, or $425,000 annually for five years, making it the most expensive drug in the world. Like Spinraza, Zolgensma is currently raising challenging questions about how insurers and government payers like Medicaid will be able to afford these treatments without bankrupting an already-strained health care system.
To Biogen's credit, the company provides financial aid for Spinraza patients with private insurance who pay co-pays for treatment, as well as for those who have been denied by Medicaid and Medicare. But getting insurance companies to agree to pay for Spinraza can often be an ordeal in itself. Although Fulton and Teddy Mantoan were approved for treatment over two years ago, a lengthy insurance battle delayed treatment for another eight months – time that, for some SMA patients, can mean a significant loss of muscular function.
Kelly didn't notice anything in either boy – positive or negative – for the first few months of Spinraza injections. But one day in November 2017, as Teddy was lowered off his school bus in his wheelchair, he turned to say goodbye to his friends and "dab," – a dance move where one's arms are extended briefly across the chest and in the air. Normally, Teddy would dab by throwing his arms up in the air with momentum, striking a pose quickly before they fell down limp at his sides. But that day, Teddy held his arms rigid in the air. His classmates, along with Kelly, were stunned. "Teddy, look at your arms!" Kelly remembers shrieking. "You're holding them up – you're dabbing!"

Teddy and Fulton Mantoan, who both suffer from spinal muscular atrophy, have seen life-changing results from Spinraza.
(Courtesy of Kelly Mantoan)
Not long after Teddy's dab, the Mantoans started seeing changes in Fulton as well. "With Fulton, we realized suddenly that he was no longer choking on his food during meals," Kelly said. "Almost every meal we'd have to stop and have him take a sip of water and make him slow down and take small bites so he wouldn't choke. But then we realized we hadn't had to do that in a long time. The nurses at school were like, 'it's not an issue anymore.'"
For the Mantoans, this was an enormous relief: Less choking meant less chance of aspiration pneumonia, a leading cause of death for people with SMA Types 1 and 2.
While Spinraza has been life-changing for the Mantoans, it remains painfully out of reach for many others. Thanks to Spinraza's enormous price tag, the threshold for who gets to use it is incredibly high: Adult and pediatric patients, particularly those with state-sponsored insurance, have reported multiple insurance denials, lengthy appeals processes, and endless bureaucracy from insurance and hospitals alike that stand in the way of treatment.
Kate Saldana, a 21-year-old woman with Type 2 SMA, is one of the many adult patients who have been lobbying for the drug. Saldana, who uses a ventilator 20 hours each day, says that Medicaid denied her Spinraza treatments because they mistakenly believed that she used a ventilator full-time. Saldana is currently in the process of appealing their decision, but knows she is fighting an uphill battle.

Kate Saldana, who suffers from Type 2 SMA, has been fighting unsuccessfully for Medicaid to cover Spinraza.
(Courtesy of Saldana)
"Originally, the treatments were studied and created for infants and children," Saldana said in an e-mail. "There is a plethora of data to support the effectiveness of Spinraza in those groups, but in adults it has not been studied as much. That makes it more difficult for insurance to approve it, because they are not sure if it will be as beneficial."
Saldana has been pursuing treatment unsuccessfully since last August – but others, like Kimberly Hill, a 32-year-old with SMA Type 2, have been waiting even longer. Hill, who lives in Oklahoma, has been fighting for treatment since Spinraza went on the U.S. market in December 2016. Because her mobility is limited to the use of her left thumb, Hill is eager to try anything that will enable her to keep working and finish a Master's degree in Fire and Emergency Management.
"Obviously, my family and I were elated with the approval of Spinraza," Hill said in an e-mail. "We thought I would finally have the chance to get a little stronger and healthier." But with Medicare and Medicaid, coverage and eligibility varies wildly by state. Earlier this year, Medicaid approved Spinraza for adult patients only if a clawback clause was attached to the approval, meaning that under certain conditions the Medicaid funds would need to be paid back. Because of the clawback clause, hospitals have been reluctant to take on Spinraza treatments, effectively barring adult Medicaid patients from accessing the drug altogether.
Hill's hospital is currently in negotiations with Medicaid to move forward with Spinraza treatment, but in the meantime, Hill is in limbo. "We keep being told there is nothing we can do, and we are devastated," Hill said.
"I felt extremely sad and honestly a bit forgotten, like adults [with SMA] don't matter."
Between Spinraza and its new competitor, Zolgensma, some are speculating that insurers will start to favor Zolgensma coverage instead, since the treatment is shorter and ultimately cheaper than Spinraza in the long term. But for some adults with SMA who can't access Spinraza and who don't qualify for Zolgensma treatment, the issue of what insurers will cover is moot.
"I was so excited when I heard that Zolgensma was approved by the FDA," said Annie Wilson, an adult SMA patient from Alameda, Calif. who has been fighting for Spinraza since 2017. "When I became aware that it was only being offered to children, I felt extremely sad and honestly a bit forgotten, like adults [with SMA] don't matter."
According to information from a Biogen representative, more than 7500 people worldwide have been treated with Spinraza to date, one third of whom are adults.
While Spinraza has been revolutionary for thousands of patients, it's unclear how many more lives state agencies and insurance companies will allow it to save.
Thanks to safety cautions from the COVID-19 pandemic, a strain of influenza has been completely eliminated.
If you were one of the millions who masked up, washed your hands thoroughly and socially distanced, pat yourself on the back—you may have helped change the course of human history.
Scientists say that thanks to these safety precautions, which were introduced in early 2020 as a way to stop transmission of the novel COVID-19 virus, a strain of influenza has been completely eliminated. This marks the first time in human history that a virus has been wiped out through non-pharmaceutical interventions, such as vaccines.
The flu shot, explained
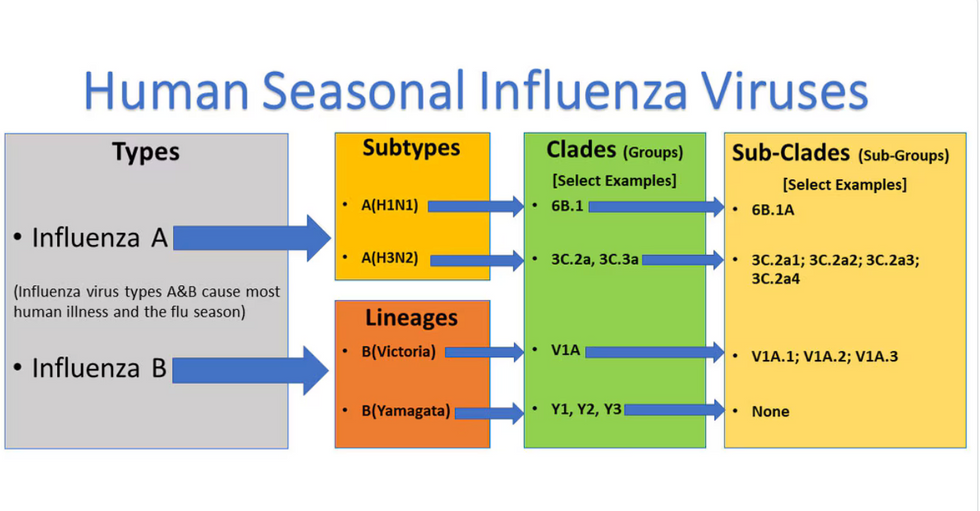
Influenza viruses type A and B are responsible for the majority of human illnesses and the flu season.
Centers for Disease Control
For more than a decade, flu shots have protected against two types of the influenza virus–type A and type B. While there are four different strains of influenza in existence (A, B, C, and D), only strains A, B, and C are capable of infecting humans, and only A and B cause pandemics. In other words, if you catch the flu during flu season, you’re most likely sick with flu type A or B.
Flu vaccines contain inactivated—or dead—influenza virus. These inactivated viruses can’t cause sickness in humans, but when administered as part of a vaccine, they teach a person’s immune system to recognize and kill those viruses when they’re encountered in the wild.
Each spring, a panel of experts gives a recommendation to the US Food and Drug Administration on which strains of each flu type to include in that year’s flu vaccine, depending on what surveillance data says is circulating and what they believe is likely to cause the most illness during the upcoming flu season. For the past decade, Americans have had access to vaccines that provide protection against two strains of influenza A and two lineages of influenza B, known as the Victoria lineage and the Yamagata lineage. But this year, the seasonal flu shot won’t include the Yamagata strain, because the Yamagata strain is no longer circulating among humans.
How Yamagata Disappeared

Flu surveillance data from the Global Initiative on Sharing All Influenza Data (GISAID) shows that the Yamagata lineage of flu type B has not been sequenced since April 2020.
Nature
Experts believe that the Yamagata lineage had already been in decline before the pandemic hit, likely because the strain was naturally less capable of infecting large numbers of people compared to the other strains. When the COVID-19 pandemic hit, the resulting safety precautions such as social distancing, isolating, hand-washing, and masking were enough to drive the virus into extinction completely.
Because the strain hasn’t been circulating since 2020, the FDA elected to remove the Yamagata strain from the seasonal flu vaccine. This will mark the first time since 2012 that the annual flu shot will be trivalent (three-component) rather than quadrivalent (four-component).
Should I still get the flu shot?
The flu shot will protect against fewer strains this year—but that doesn’t mean we should skip it. Influenza places a substantial health burden on the United States every year, responsible for hundreds of thousands of hospitalizations and tens of thousands of deaths. The flu shot has been shown to prevent millions of illnesses each year (more than six million during the 2022-2023 season). And while it’s still possible to catch the flu after getting the flu shot, studies show that people are far less likely to be hospitalized or die when they’re vaccinated.
Another unexpected benefit of dropping the Yamagata strain from the seasonal vaccine? This will possibly make production of the flu vaccine faster, and enable manufacturers to make more vaccines, helping countries who have a flu vaccine shortage and potentially saving millions more lives.
After his grandmother’s dementia diagnosis, one man invented a snack to keep her healthy and hydrated.
Founder Lewis Hornby and his grandmother Pat, sampling Jelly Drops—an edible gummy containing water and life-saving electrolytes.
On a visit to his grandmother’s nursing home in 2016, college student Lewis Hornby made a shocking discovery: Dehydration is a common (and dangerous) problem among seniors—especially those that are diagnosed with dementia.
Hornby’s grandmother, Pat, had always had difficulty keeping up her water intake as she got older, a common issue with seniors. As we age, our body composition changes, and we naturally hold less water than younger adults or children, so it’s easier to become dehydrated quickly if those fluids aren’t replenished. What’s more, our thirst signals diminish naturally as we age as well—meaning our body is not as good as it once was in letting us know that we need to rehydrate. This often creates a perfect storm that commonly leads to dehydration. In Pat’s case, her dehydration was so severe she nearly died.
When Lewis Hornby visited his grandmother at her nursing home afterward, he learned that dehydration especially affects people with dementia, as they often don’t feel thirst cues at all, or may not recognize how to use cups correctly. But while dementia patients often don’t remember to drink water, it seemed to Hornby that they had less problem remembering to eat, particularly candy.

Hornby wanted to create a solution for elderly people who struggled keeping their fluid intake up. He spent the next eighteen months researching and designing a solution and securing funding for his project. In 2019, Hornby won a sizable grant from the Alzheimer’s Society, a UK-based care and research charity for people with dementia and their caregivers. Together, through the charity’s Accelerator Program, they created a bite-sized, sugar-free, edible jelly drop that looked and tasted like candy. The candy, called Jelly Drops, contained 95% water and electrolytes—important minerals that are often lost during dehydration. The final product launched in 2020—and was an immediate success. The drops were able to provide extra hydration to the elderly, as well as help keep dementia patients safe, since dehydration commonly leads to confusion, hospitalization, and sometimes even death.
Not only did Jelly Drops quickly become a favorite snack among dementia patients in the UK, but they were able to provide an additional boost of hydration to hospital workers during the pandemic. In NHS coronavirus hospital wards, patients infected with the virus were regularly given Jelly Drops to keep their fluid levels normal—and staff members snacked on them as well, since long shifts and personal protective equipment (PPE) they were required to wear often left them feeling parched.
In April 2022, Jelly Drops launched in the United States. The company continues to donate 1% of its profits to help fund Alzheimer’s research.

