Anti-Aging Pioneer Aubrey de Grey: “People in Middle Age Now Have a Fair Chance”
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

Aubrey de Grey at the World Stem Cell Summit in Miami on January 25, 2018.
Aging is not a mystery, says famed researcher Dr. Aubrey de Grey, perhaps the world's foremost advocate of the provocative view that medical technology will one day allow humans to control the aging process and live healthily into our hundreds—or even thousands.
"The cultural attitudes toward all of this are going to be completely turned upside down by sufficiently promising results in the lab, in mice."
He likens aging to a car wearing down over time; as the body operates normally, it accumulates damage which can be tolerated for a while, but eventually sends us into steep decline. The most promising way to escape this biological reality, he says, is to repair the damage as needed with precise scientific tools.
The bad news is that doing this groundbreaking research takes a long time and a lot of money, which has not always been readily available, in part due to a cultural phenomenon he terms "the pro-aging trance." Cultural attitudes have long been fatalistic about the inevitability of aging; many people balk at the seemingly implausible prospect of indefinite longevity.
But the good news for de Grey—and those who are cheering him on—is that his view is becoming less radical these days. Both the academic and private sectors are racing to tackle aging; his own SENS Research Foundation, for one, has spun out into five different companies. Defeating aging, he says, "is not just a future industry; it's an industry now that will be both profitable and extremely good for your health."
De Grey sat down with Editor-in-Chief Kira Peikoff at the World Stem Cell Summit in Miami to give LeapsMag the latest scoop on his work. Here is an edited and condensed version of our conversation.
Since your book Ending Aging was published a decade ago, scientific breakthroughs in stem cell research, genome editing, and other fields have taken the world by storm. Which of these have most affected your research?
They have all affected it a lot in one way, and hardly at all in another way. They have speeded it up--facilitated short cuts, ways to get where we're already trying to go. What they have not done is identified any fundamental changes to the overall strategy. In the book, we described the seven major types of damage, and particular ways of going about fixing each of them, and that hasn't changed.
"Repair at the microscopic level, one would be able to expect to do without surgery, just by injecting the right kind of stem cells."
Has any breakthrough specifically made the biggest impact?
It's not just the obvious things, like iPS (induced pluripotent stem cells) and CRISPR (a precise tool for editing genes). It's also the more esoteric things that applied specifically to certain of our areas, but most people don't really know about them. For example, the identification of how to control something called co-translational mitochondrial protein import.
How much of the future of anti-aging treatments will involve regeneration of old tissue, or wholesale growth of new organs?
The more large-scale ones, regenerating whole new organs, are probably only going to play a role in the short-term and will be phased out relatively rapidly, simply because, in order to be useful, one has to employ surgery, which is really invasive. We'll want to try to get around that, but it seems quite likely that in the very early stages, the techniques we have for repairing things at the molecular and cellular level in situ will be insufficiently comprehensive, and so we will need to do the more sledgehammer approach of building a whole new organ and sticking it in.
Every time you are in a position where you're replacing an organ, you have the option, in principle, of repairing the organ, without replacing it. And repair at the microscopic level, one would be able to expect to do without surgery, just by injecting the right kind of stem cells or whatever. That would be something one would expect to be able to apply to someone much closer to death's door and much more safely in general, and probably much more cheaply. One would expect that subsequent generations of these therapies would move in that direction.
Your foundation is working on an initiative requiring $50 million in funding—
Well, if we had $50 million per year in funding, we could go about three times faster than we are on $5 million per year.
And you're looking at a 2021 timeframe to start human trials?
That's approximate. Remember, because we accumulate in the body so many different types of damage, that means we have many different types of therapy to repair that damage. And of course, each of those types has to be developed independently. It's very much a divide and conquer therapy. The therapies interact with each other to some extent; the repair of one type of damage may slow down the creation of another type of damage, but still that's how it's going to be.
And some of these therapies are much easier to implement than others. The easier components of what we need to do are already in clinical trials—stem cell therapies especially, and immunotherapy against amyloid in the brain, for example. Even in phase III clinical trials in some cases. So when I talk about a timeframe like 2021, or early 20s shall we say, I'm really talking about the most difficult components.
What recent strides are you most excited about?
Looking back over the past couple of years, I'm particularly proud of the successes we've had in the very most difficult areas. If you go through the 7 components of SENS, there are two that have absolutely been stuck in a rut and have gotten nowhere for 15 to 20 years, and we basically fixed that in both cases. We published two years ago in Science magazine that essentially showed a way forward against the stiffening of the extracellular matrix, which is responsible for things like wrinkles and hypertension. And then a year ago, we published a real breakthrough paper with regard to placing copies of the mitochondria DNA in the nuclear DNA modified in such a way that they still work, which is an idea that had been around for 30 years; everyone had given up on it, some a long time ago, and we basically revived it.
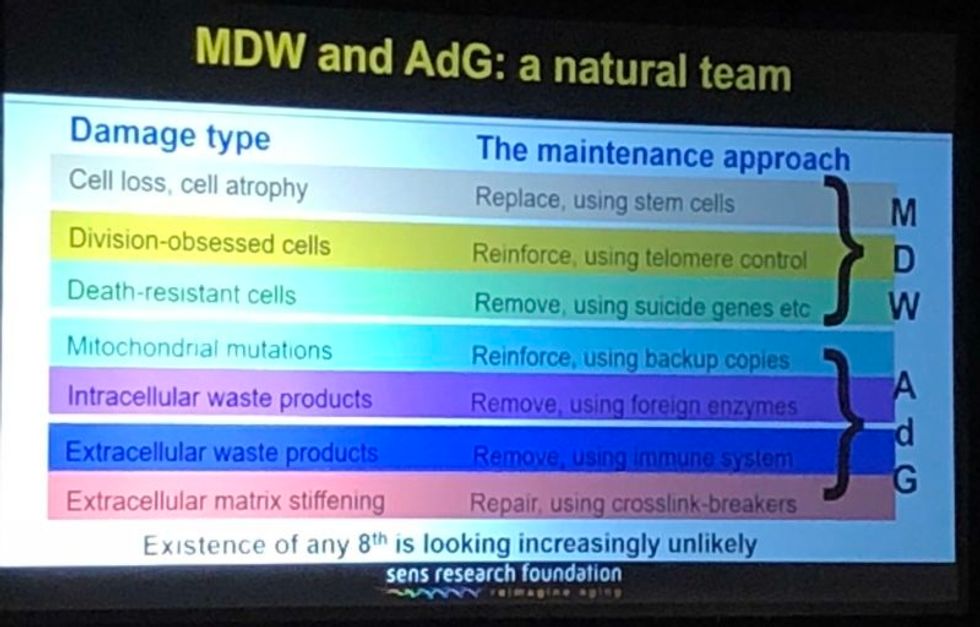
A slide presented by Aubrey de Grey, referencing his collaboration with Mike West at AgeX, showing the 7 types of damage that he believes must be repaired to end aging.
(Courtesy Kira Peikoff)
That's exciting. What do you think are the biggest barriers to defeating aging today: the technological challenges, the regulatory framework, the cost, or the cultural attitude of the "pro-aging" trance?
One can't really address those independently of each other. The technological side is one thing; it's hard, but we know where we're going, we've got a plan. The other ones are very intertwined with each other. A lot of people are inclined to say, the regulatory hurdle will be completely insurmountable, plus people don't recognize aging as a disease, so it's going to be a complete nonstarter. I think that's nonsense. And the reason is because the cultural attitudes toward all of this are going to be completely turned upside down before we have to worry about the regulatory hurdles. In other words, they're going to be turned upside down by sufficiently promising results in the lab, in mice. Once we get to be able to rejuvenate actually old mice really well so they live substantially longer than they otherwise would have done, in a healthy state, everyone's going to know about it and everyone's going to demand – it's not going to be possible to get re-elected unless you have a manifesto commitment to turn the FDA completely upside down and make sure this happens without any kind of regulatory obstacle.
I've been struggling away all these years trying to bring little bits of money in the door, and the reason I have is because of the skepticism as to regards whether this could actually work, combined with the pro-aging trance, which is a product of the skepticism – people not wanting to get their hopes up, so finding excuses about aging being a blessing in disguise, so they don't have to think about it. All of that will literally disintegrate pretty much overnight when we have the right kind of sufficiently impressive progress in the lab. Therefore, the availability of money will also [open up]. It's already cracking: we're already seeing the beginnings of the actual rejuvenation biotechnology industry that I've been talking about with a twinkle in my eye for some years.
"For humans, a 50-50 chance would be twenty years at this point, and there's a 10 percent chance that we won't get there for a hundred years."
Why do you think the culture is starting to shift?
There's no one thing yet. There will be that tipping point I mentioned, perhaps five years from now when we get a real breakthrough, decisive results in mice that make it simply impossible to carry on being fatalistic about all this. Prior to that, what we're already seeing is the impact of sheer old-school repeat advertising—me going out there, banging away and saying the same fucking thing again and again, and nobody saying anything that persuasively knocks me down. … And it's also the fact that we are making incremental amounts of progress, not just ourselves, but the scientific community generally. It has become incrementally more plausible that what I say might be true.
I'm sure you hate getting the timeline question, but if we're five years away from this breakthrough in mice, it's hard to resist asking—how far is that in terms of a human cure?
When I give any kind of timeframes, the only real care I have to take is to emphasize the variance. In this case I think we have got a 50-50 chance of getting to that tipping point in mice within five years from now, certainly it could be 10 or 15 years if we get unlucky. Similarly, for humans, a 50-50 chance would be twenty years at this point, and there's a 10 percent chance that we won't get there for a hundred years.
"I don't get people coming to me saying, well I don't think medicine for the elderly should be done because if it worked it would be a bad thing. People like to ignore this contradiction."
What would you tell skeptical people are the biggest benefits of a very long-lived population?
Any question about the longevity of people is the wrong question. Because the longevity that people fixate about so much will only ever occur as a side effect of health. However long ago you were born or however recently, if you're sick, you're likely to die fairly soon unless we can stop you being sick. Whereas if you're healthy, you're not. So if we do as well as we think we can do in terms of keeping people healthy and youthful however long ago they were born, then the side effect in terms of longevity and life expectancy is likely to be very large. But it's still a side effect, so the way that people actually ought to be—in fact have a requirement to be—thinking, is about whether they want people to be healthy.
Now I don't get people coming to me saying, well I don't think medicine for the elderly should be done because if it worked it would be a bad thing. People like to ignore this contradiction, they like to sweep it under the carpet and say, oh yeah, aging is totally a good thing.
People will never actually admit to the fact that what they are fundamentally saying is medicine for the elderly, if it actually works, would be bad, but still that is what they are saying.
Shifting gears a bit, I'm curious to find out which other radical visionaries in science and tech today you most admire?
Fair question. One is Mike West. I have the great privilege that I now work for him part-time with Age X. I have looked up to him very much for the past ten years, because what he did over the past 20 years starting with Geron is unimaginable today. He was working in an environment where I would not have dreamt of the possibility of getting any private money, any actual investment, in something that far out, that far ahead of its time, and he did it, again and again. It's insane what he managed to do.
What about someone like Elon Musk?
Sure, he's another one. He is totally impervious to the caution and criticism and conservatism that pervades humanity, and he's getting on making these bloody self-driving cars, space tourism, and so on, making them happen. He's thinking just the way I'm thinking really.
"You can just choose how frequently and how thoroughly you repair the damage. And you can make a different choice next time."
You famously said ten years ago that you think the first person to live to 1000 is already alive. Do you think that's still the case?
Definitely, yeah. I can't see how it could not be. Again, it's a probabilistic thing. I said there's at least a 10 percent chance that we won't get to what I call Longevity Escape Velocity for 100 years and if that's true, then the statement about 1000 years being alive already is not going to be the case. But for sure, I believe that the beneficiaries of what we may as well call SENS 1.0, the point where we get to LEV, those people are exceptionally unlikely ever to suffer from any kind of ill health correlated with their age. Because we will never fall below Longevity Escape Velocity once we attain it.
Could someone who was just born today expect—
I would say people in middle age now have a fair chance. Remember – a 50/50 chance of getting to LEV within 20 years, and when you get there, you don't just stay at biologically 70 or 80, you are rejuvenated back to biologically 30 or 40 and you stay there, so your risk of death each year is not related to how long ago you were born, it's the same as a young adult. Today, that's less than 1 in 1000 per year, and that number is going to go down as we get self-driving cars and all that, so actually 1000 is a very conservative number.
So you would be able to choose what age you wanted to go back to?
Oh sure, of course, it's just like a car. What you're doing is you're repairing damage, and the damage is still being created by the body's metabolism, so you can just choose how frequently and how thoroughly you repair the damage. And you can make a different choice next time.
What would be your perfect age?
I have no idea. That's something I don't have an opinion about, because I could change it whenever I like.
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Indigenous wisdom plus honeypot ants could provide new antibiotics
Indigenous people in Australia dig pits next to a honeypot colony. Scientists think the honey can be used to make new antimicrobial drugs.
For generations, the Indigenous Tjupan people of Australia enjoyed the sweet treat of honey made by honeypot ants. As a favorite pastime, entire families would go searching for the underground colonies, first spotting a worker ant and then tracing it to its home. The ants, which belong to the species called Camponotus inflatus, usually build their subterranean homes near the mulga trees, Acacia aneura. Having traced an ant to its tree, it would be the women who carefully dug a pit next to a colony, cautious not to destroy the entire structure. Once the ant chambers were exposed, the women would harvest a small amount to avoid devastating the colony’s stocks—and the family would share the treat.
The Tjupan people also knew that the honey had antimicrobial properties. “You could use it for a sore throat,” says Danny Ulrich, a member of the Tjupan nation. “You could also use it topically, on cuts and things like that.”
These hunts have become rarer, as many of the Tjupan people have moved away and, up until now, the exact antimicrobial properties of the ant honey remained unknown. But recently, scientists Andrew Dong and Kenya Fernandes from the University of Sydney, joined Ulrich, who runs the Honeypot Ants tours in Kalgoorlie, a city in Western Australia, on a honey-gathering expedition. Afterwards, they ran a series of experiments analyzing the honey’s antimicrobial activity—and confirmed that the Indigenous wisdom was true. The honey was effective against Staphylococcus aureus, a common pathogen responsible for sore throats, skin infections like boils and sores, and also sepsis, which can result in death. Moreover, the honey also worked against two species of fungi, Cryptococcus and Aspergillus, which can be pathogenic to humans, especially those with suppressed immune systems.
In the era of growing antibiotic resistance and the rising threat of pathogenic fungi, these findings may help scientists identify and make new antimicrobial compounds. “Natural products have been honed over thousands and millions of years by nature and evolution,” says Fernandes. “And some of them have complex and intricate properties that make them really important as potential new antibiotics. “

In an era of growing resistance to antibiotics and new threats of fungi infections, the latest findings about honeypot ants are helping scientists identify new antimicrobial drugs.
Danny Ulrich
Bee honey is also known for its antimicrobial properties, but bees produce it very differently than the ants. Bees collect nectar from flowers, which they regurgitate at the hive and pack into the hexagonal honeycombs they build for storage. As they do so, they also add into the mix an enzyme called glucose oxidase produced by their glands. The enzyme converts atmospheric oxygen into hydrogen peroxide, a reactive molecule that destroys bacteria and acts as a natural preservative. After the bees pack the honey into the honeycombs, they fan it with their wings to evaporate the water. Once a honeycomb is full, the bees put a beeswax cover on it, where it stays well-preserved thanks to the enzymatic action, until the bees need it.
Less is known about the chemistry of ants’ honey-making. Similarly to bees, they collect nectar. They also collect the sweet sap of the mulga tree. Additionally, they also “milk” the aphids—small sap-sucking insects that live on the tree. When ants tickle the aphids with their antennae, the latter release a sweet substance, which the former also transfer to their colonies. That’s where the honey management difference becomes really pronounced. The ants don’t build any kind of structures to store their honey. Instead, they store it in themselves.
The workers feed their harvest to their fellow ants called repletes, stuffing them up to the point that their swollen bellies outgrow the ants themselves, looking like amber-colored honeypots—hence the name. Because of their size, repletes don’t move, but hang down from the chamber’s ceiling, acting as living feedstocks. When food becomes scarce, they regurgitate their reserves to their colony’s brethren. It’s not clear whether the repletes die afterwards or can be restuffed again. “That's a good question,” Dong says. “After they've been stretched, they can't really return to exactly the same shape.”
These replete ants are the “treat” the Tjupan women dug for. Once they saw the round-belly ants inside the chambers, they would reach in carefully and get a few scoops of them. “You see a lot of honeypot ants just hanging on the roof of the little openings,” says Ulrich’s mother, Edie Ulrich. The women would share the ants with family members who would eat them one by one. “They're very delicate,” shares Edie Ulrich—you have to take them out carefully, so they don’t accidentally pop and become a wasted resource. “Because you’d lose all this precious honey.”
Dong stumbled upon the honeypot ants phenomenon because he was interested in Indigenous foods and went on Ulrich’s tour. He quickly became fascinated with the insects and their role in the Indigenous culture. “The honeypot ants are culturally revered by the Indigenous people,” he says. Eventually he decided to test out the honey’s medicinal qualities.
The researchers were surprised to see that even the smallest, eight percent concentration of honey was able to arrest the growth of S. aureus.
To do this, the two scientists first diluted the ant honey with water. “We used something called doubling dilutions, which means that we made 32 percent dilutions, and then we halve that to 16 percent and then we half that to eight percent,” explains Fernandes. The goal was to obtain as much results as possible with the meager honey they had. “We had very, very little of the honeypot ant honey so we wanted to maximize the spectrum of results we can get without wasting too much of the sample.”
After that, the researchers grew different microbes inside a nutrient rich broth. They added the broth to the different honey dilutions and incubated the mixes for a day or two at the temperature favorable to the germs’ growth. If the resulting solution turned turbid, it was a sign that the bugs proliferated. If it stayed clear, it meant that the honey destroyed them. The researchers were surprised to see that even the smallest, eight percent concentration of honey was able to arrest the growth of S. aureus. “It was really quite amazing,” Fernandes says. “Eight milliliters of honey in 92 milliliters of water is a really tiny amount of honey compared to the amount of water.”
Similar to bee honey, the ants’ honey exhibited some peroxide antimicrobial activity, researchers found, but given how little peroxide was in the solution, they think the honey also kills germs by a different mechanism. “When we measured, we found that [the solution] did have some hydrogen peroxide, but it didn't have as much of it as we would expect based on how active it was,” Fernandes says. “Whether this hydrogen peroxide also comes from glucose oxidase or whether it's produced by another source, we don't really know,” she adds. The research team does have some hypotheses about the identity of this other germ-killing agent. “We think it is most likely some kind of antimicrobial peptide that is actually coming from the ant itself.”
The honey also has a very strong activity against the two types of fungi, Cryptococcus and Aspergillus. Both fungi are associated with trees and decaying leaves, as well as in the soils where ants live, so the insects likely have evolved some natural defense compounds, which end up inside the honey.
It wouldn’t be the first time when modern medicines take their origin from the natural world or from the indigenous people’s knowledge. The bark of the cinchona tree native to South America contains quinine, a substance that treats malaria. The Indigenous people of the Andes used the bark to quell fever and chills for generations, and when Europeans began to fall ill with malaria in the Amazon rainforest, they learned to use that medicine from the Andean people.
The wonder drug aspirin similarly takes its origin from a bark of a tree—in this case a willow.
Even some anticancer compounds originated from nature. A chemotherapy drug called Paclitaxel, was originally extracted from the Pacific yew trees, Taxus brevifolia. The samples of the Pacific yew bark were first collected in 1962 by researchers from the United States Department of Agriculture who were looking for natural compounds that might have anti-tumor activity. In December 1992, the FDA approved Paclitaxel (brand name Taxol) for the treatment of ovarian cancer and two years later for breast cancer.
In the era when the world is struggling to find new medicines fast enough to subvert a fungal or bacterial pandemic, these discoveries can pave the way to new therapeutics. “I think it's really important to listen to indigenous cultures and to take their knowledge because they have been using these sources for a really, really long time,” Fernandes says. Now we know it works, so science can elucidate the molecular mechanisms behind it, she adds. “And maybe it can even provide a lead for us to develop some kind of new treatments in the future.”
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.
Blood Test Can Detect Lymphoma Cells Before a Tumor Grows Back
David Kurtz making DNA sequencing libraries in his lab.
When David M. Kurtz was doing his clinical fellowship at Stanford University Medical Center in 2009, specializing in lymphoma treatments, he found himself grappling with a question no one could answer. A typical regimen for these blood cancers prescribed six cycles of chemotherapy, but no one knew why. "The number seemed to be drawn out of a hat," Kurtz says. Some patients felt much better after just two doses, but had to endure the toxic effects of the entire course. For some elderly patients, the side effects of chemo are so harsh, they alone can kill. Others appeared to be cancer-free on the CT scans after the requisite six but then succumbed to it months later.
"Anecdotally, one patient decided to stop therapy after one dose because he felt it was so toxic that he opted for hospice instead," says Kurtz, now an oncologist at the center. "Five years down the road, he was alive and well. For him, just one dose was enough." Others would return for their one-year check up and find that their tumors grew back. Kurtz felt that while CT scans and MRIs were powerful tools, they weren't perfect ones. They couldn't tell him if there were any cancer cells left, stealthily waiting to germinate again. The scans only showed the tumor once it was back.
Blood cancers claim about 68,000 people a year, with a new diagnosis made about every three minutes, according to the Leukemia Research Foundation. For patients with B-cell lymphoma, which Kurtz focuses on, the survival chances are better than for some others. About 60 percent are cured, but the remaining 40 percent will relapse—possibly because they will have a negative CT scan, but still harbor malignant cells. "You can't see this on imaging," says Michael Green, who also treats blood cancers at University of Texas MD Anderson Medical Center.
The new blood test is sensitive enough to spot one cancerous perpetrator amongst one million other DNA molecules.
Kurtz wanted a better diagnostic tool, so he started working on a blood test that could capture the circulating tumor DNA or ctDNA. For that, he needed to identify the specific mutations typical for B-cell lymphomas. Working together with another fellow PhD student Jake Chabon, Kurtz finally zeroed-in on the tumor's genetic "appearance" in 2017—a pair of specific mutations sitting in close proximity to each other—a rare and telling sign. The human genome contains about 3 billion base pairs of nucleotides—molecules that compose genes—and in case of the B-cell lymphoma cells these two mutations were only a few base pairs apart. "That was the moment when the light bulb went on," Kurtz says.
The duo formed a company named Foresight Diagnostics, focusing on taking the blood test to the clinic. But knowing the tumor's mutational signature was only half the process. The other was fishing the tumor's DNA out of patients' bloodstream that contains millions of other DNA molecules, explains Chabon, now Foresight's CEO. It would be like looking for an escaped criminal in a large crowd. Kurtz and Chabon solved the problem by taking the tumor's "mug shot" first. Doctors would take the biopsy pre-treatment and sequence the tumor, as if taking the criminal's photo. After treatments, they would match the "mug shot" to all DNA molecules derived from the patient's blood sample to see if any molecular criminals managed to escape the chemo.
Foresight isn't the only company working on blood-based tumor detection tests, which are dubbed liquid biopsies—other companies such as Natera or ArcherDx developed their own. But in a recent study, the Foresight team showed that their method is significantly more sensitive in "fishing out" the cancer molecules than existing tests. Chabon says that this test can detect circulating tumor DNA in concentrations that are nearly 100 times lower than other methods. Put another way, it's sensitive enough to spot one cancerous perpetrator amongst one million other DNA molecules.
They also aim to extend their test to detect other malignancies such as lung, breast or colorectal cancers.
"It increases the sensitivity of detection and really catches most patients who are going to progress," says Green, the University of Texas oncologist who wasn't involved in the study, but is familiar with the method. It would also allow monitoring patients during treatment and making better-informed decisions about which therapy regimens would be most effective. "It's a minimally invasive test," Green says, and "it gives you a very high confidence about what's going on."
Having shown that the test works well, Kurtz and Chabon are planning a new trial in which oncologists would rely on their method to decide when to stop or continue chemo. They also aim to extend their test to detect other malignancies such as lung, breast or colorectal cancers. The latest genome sequencing technologies have sequenced and catalogued over 2,500 different tumor specimens and the Foresight team is analyzing this data, says Chabon, which gives the team the opportunity to create more molecular "mug shots."
The team hopes that that their blood cancer test will become available to patients within about five years, making doctors' job easier, and not only at the biological level. "When I tell patients, "good news, your cancer is in remission', they ask me, 'does it mean I'm cured?'" Kurtz says. "Right now I can't answer this question because I don't know—but I would like to." His company's test, he hopes, will enable him to reply with certainty. He'd very much like to have the power of that foresight.
This article is republished from our archives to coincide with Blood Cancer Awareness Month, which highlights progress in cancer diagnostics and treatment.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.