Scientists redesign bacteria to tackle the antibiotic resistance crisis

Probiotic bacteria can be engineered to fight antibiotic-resistant superbugs by releasing chemicals that kill them.
In 1945, almost two decades after Alexander Fleming discovered penicillin, he warned that as antibiotics use grows, they may lose their efficiency. He was prescient—the first case of penicillin resistance was reported two years later. Back then, not many people paid attention to Fleming’s warning. After all, the “golden era” of the antibiotics age had just began. By the 1950s, three new antibiotics derived from soil bacteria — streptomycin, chloramphenicol, and tetracycline — could cure infectious diseases like tuberculosis, cholera, meningitis and typhoid fever, among others.
Today, these antibiotics and many of their successors developed through the 1980s are gradually losing their effectiveness. The extensive overuse and misuse of antibiotics led to the rise of drug resistance. The livestock sector buys around 80 percent of all antibiotics sold in the U.S. every year. Farmers feed cows and chickens low doses of antibiotics to prevent infections and fatten up the animals, which eventually causes resistant bacterial strains to evolve. If manure from cattle is used on fields, the soil and vegetables can get contaminated with antibiotic-resistant bacteria. Another major factor is doctors overprescribing antibiotics to humans, particularly in low-income countries. Between 2000 to 2018, the global rates of human antibiotic consumption shot up by 46 percent.
In recent years, researchers have been exploring a promising avenue: the use of synthetic biology to engineer new bacteria that may work better than antibiotics. The need continues to grow, as a Lancet study linked antibiotic resistance to over 1.27 million deaths worldwide in 2019, surpassing HIV/AIDS and malaria. The western sub-Saharan Africa region had the highest death rate (27.3 people per 100,000).
Researchers warn that if nothing changes, by 2050, antibiotic resistance could kill 10 million people annually.
To make it worse, our remedy pipelines are drying up. Out of the 18 biggest pharmaceutical companies, 15 abandoned antibiotic development by 2013. According to the AMR Action Fund, venture capital has remained indifferent towards biotech start-ups developing new antibiotics. In 2019, at least two antibiotic start-ups filed for bankruptcy. As of December 2020, there were 43 new antibiotics in clinical development. But because they are based on previously known molecules, scientists say they are inadequate for treating multidrug-resistant bacteria. Researchers warn that if nothing changes, by 2050, antibiotic resistance could kill 10 million people annually.
The rise of synthetic biology
To circumvent this dire future, scientists have been working on alternative solutions using synthetic biology tools, meaning genetically modifying good bacteria to fight the bad ones.
From the time life evolved on earth around 3.8 billion years ago, bacteria have engaged in biological warfare. They constantly strategize new methods to combat each other by synthesizing toxic proteins that kill competition.
For example, Escherichia coli produces bacteriocins or toxins to kill other strains of E.coli that attempt to colonize the same habitat. Microbes like E.coli (which are not all pathogenic) are also naturally present in the human microbiome. The human microbiome harbors up to 100 trillion symbiotic microbial cells. The majority of them are beneficial organisms residing in the gut at different compositions.
The chemicals that these “good bacteria” produce do not pose any health risks to us, but can be toxic to other bacteria, particularly to human pathogens. For the last three decades, scientists have been manipulating bacteria’s biological warfare tactics to our collective advantage.
In the late 1990s, researchers drew inspiration from electrical and computing engineering principles that involve constructing digital circuits to control devices. In certain ways, every cell in living organisms works like a tiny computer. The cell receives messages in the form of biochemical molecules that cling on to its surface. Those messages get processed within the cells through a series of complex molecular interactions.
Synthetic biologists can harness these living cells’ information processing skills and use them to construct genetic circuits that perform specific instructions—for example, secrete a toxin that kills pathogenic bacteria. “Any synthetic genetic circuit is merely a piece of information that hangs around in the bacteria’s cytoplasm,” explains José Rubén Morones-Ramírez, a professor at the Autonomous University of Nuevo León, Mexico. Then the ribosome, which synthesizes proteins in the cell, processes that new information, making the compounds scientists want bacteria to make. “The genetic circuit remains separated from the living cell’s DNA,” Morones-Ramírez explains. When the engineered bacteria replicates, the genetic circuit doesn’t become part of its genome.
Highly intelligent by bacterial standards, some multidrug resistant V. cholerae strains can also “collaborate” with other intestinal bacterial species to gain advantage and take hold of the gut.
In 2000, Boston-based researchers constructed an E.coli with a genetic switch that toggled between turning genes on and off two. Later, they built some safety checks into their bacteria. “To prevent unintentional or deleterious consequences, in 2009, we built a safety switch in the engineered bacteria’s genetic circuit that gets triggered after it gets exposed to a pathogen," says James Collins, a professor of biological engineering at MIT and faculty member at Harvard University’s Wyss Institute. “After getting rid of the pathogen, the engineered bacteria is designed to switch off and leave the patient's body.”
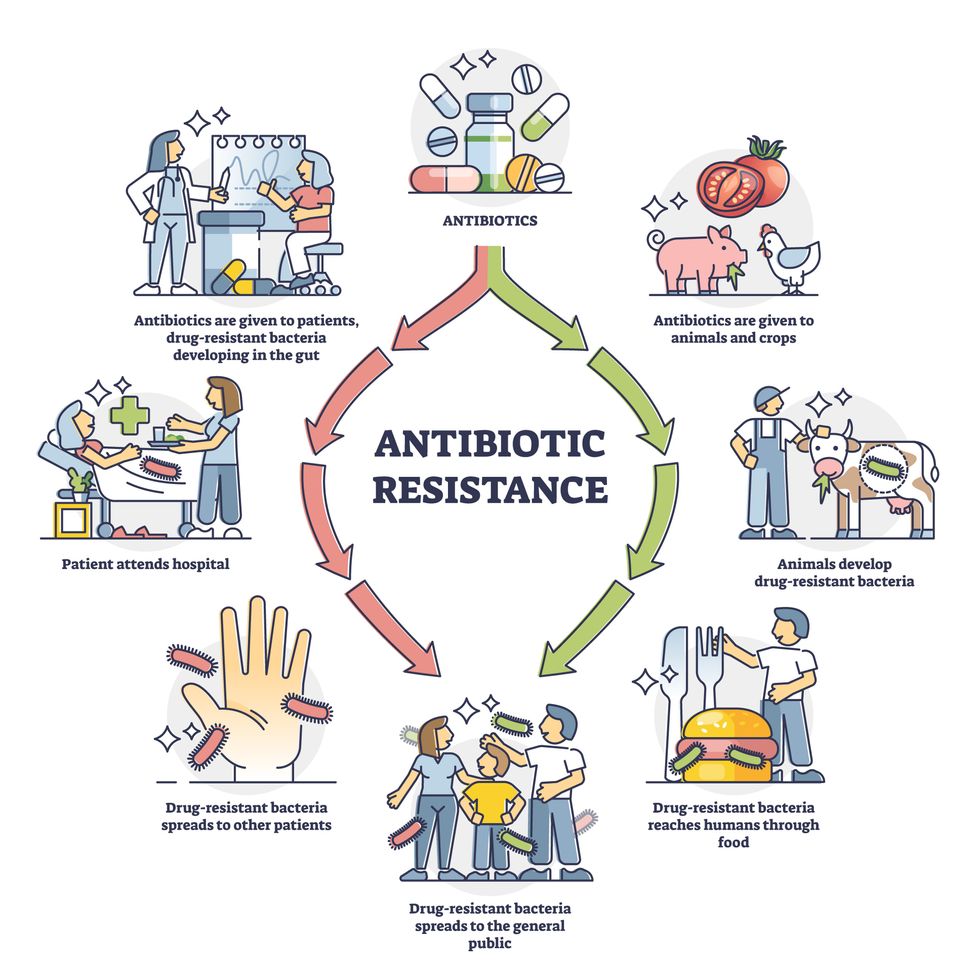
Overuse and misuse of antibiotics causes resistant strains to evolve
Adobe Stock
Seek and destroy
As the field of synthetic biology developed, scientists began using engineered bacteria to tackle superbugs. They first focused on Vibrio cholerae, which in the 19th and 20th century caused cholera pandemics in India, China, the Middle East, Europe, and Americas. Like many other bacteria, V. cholerae communicate with each other via quorum sensing, a process in which the microorganisms release different signaling molecules, to convey messages to its brethren. Highly intelligent by bacterial standards, some multidrug resistant V. cholerae strains can also “collaborate” with other intestinal bacterial species to gain advantage and take hold of the gut. When untreated, cholera has a mortality rate of 25 to 50 percent and outbreaks frequently occur in developing countries, especially during floods and droughts.
Sometimes, however, V. cholerae makes mistakes. In 2008, researchers at Cornell University observed that when quorum sensing V. cholerae accidentally released high concentrations of a signaling molecule called CAI-1, it had a counterproductive effect—the pathogen couldn’t colonize the gut.
So the group, led by John March, professor of biological and environmental engineering, developed a novel strategy to combat V. cholerae. They genetically engineered E.coli to eavesdrop on V. cholerae communication networks and equipped it with the ability to release the CAI-1 molecules. That interfered with V. cholerae progress. Two years later, the Cornell team showed that V. cholerae-infected mice treated with engineered E.coli had a 92 percent survival rate.
These findings inspired researchers to sic the good bacteria present in foods like yogurt and kimchi onto the drug-resistant ones.
Three years later in 2011, Singapore-based scientists engineered E.coli to detect and destroy Pseudomonas aeruginosa, an often drug-resistant pathogen that causes pneumonia, urinary tract infections, and sepsis. Once the genetically engineered E.coli found its target through its quorum sensing molecules, it then released a peptide, that could eradicate 99 percent of P. aeruginosa cells in a test-tube experiment. The team outlined their work in a Molecular Systems Biology study.
“At the time, we knew that we were entering new, uncharted territory,” says lead author Matthew Chang, an associate professor and synthetic biologist at the National University of Singapore and lead author of the study. “To date, we are still in the process of trying to understand how long these microbes stay in our bodies and how they might continue to evolve.”
More teams followed the same path. In a 2013 study, MIT researchers also genetically engineered E.coli to detect P. aeruginosa via the pathogen’s quorum-sensing molecules. It then destroyed the pathogen by secreting a lab-made toxin.
Probiotics that fight
A year later in 2014, a Nature study found that the abundance of Ruminococcus obeum, a probiotic bacteria naturally occurring in the human microbiome, interrupts and reduces V.cholerae’s colonization— by detecting the pathogen’s quorum sensing molecules. The natural accumulation of R. obeum in Bangladeshi adults helped them recover from cholera despite living in an area with frequent outbreaks.
The findings from 2008 to 2014 inspired Collins and his team to delve into how good bacteria present in foods like yogurt and kimchi can attack drug-resistant bacteria. In 2018, Collins and his team developed the engineered probiotic strategy. They tweaked a bacteria commonly found in yogurt called Lactococcus lactis to treat cholera.
Engineered bacteria can be trained to target pathogens when they are at their most vulnerable metabolic stage in the human gut. --José Rubén Morones-Ramírez.
More scientists followed with more experiments. So far, researchers have engineered various probiotic organisms to fight pathogenic bacteria like Staphylococcus aureus (leading cause of skin, tissue, bone, joint and blood infections) and Clostridium perfringens (which causes watery diarrhea) in test-tube and animal experiments. In 2020, Russian scientists engineered a probiotic called Pichia pastoris to produce an enzyme called lysostaphin that eradicated S. aureus in vitro. Another 2020 study from China used an engineered probiotic bacteria Lactobacilli casei as a vaccine to prevent C. perfringens infection in rabbits.
In a study last year, Ramírez’s group at the Autonomous University of Nuevo León, engineered E. coli to detect quorum-sensing molecules from Methicillin-resistant Staphylococcus aureus or MRSA, a notorious superbug. The E. coli then releases a bacteriocin that kills MRSA. “An antibiotic is just a molecule that is not intelligent,” says Ramírez. “On the other hand, engineered bacteria can be trained to target pathogens when they are at their most vulnerable metabolic stage in the human gut.”
Collins and Timothy Lu, an associate professor of biological engineering at MIT, found that engineered E. coli can help treat other conditions—such as phenylketonuria, a rare metabolic disorder, that causes the build-up of an amino acid phenylalanine. Their start-up Synlogic aims to commercialize the technology, and has completed a phase 2 clinical trial.
Circumventing the challenges
The bacteria-engineering technique is not without pitfalls. One major challenge is that beneficial gut bacteria produce their own quorum-sensing molecules that can be similar to those that pathogens secrete. If an engineered bacteria’s biosensor is not specific enough, it will be ineffective.
Another concern is whether engineered bacteria might mutate after entering the gut. “As with any technology, there are risks where bad actors could have the capability to engineer a microbe to act quite nastily,” says Collins of MIT. But Collins and Ramírez both insist that the chances of the engineered bacteria mutating on its own are virtually non-existent. “It is extremely unlikely for the engineered bacteria to mutate,” Ramírez says. “Coaxing a living cell to do anything on command is immensely challenging. Usually, the greater risk is that the engineered bacteria entirely lose its functionality.”
However, the biggest challenge is bringing the curative bacteria to consumers. Pharmaceutical companies aren’t interested in antibiotics or their alternatives because it’s less profitable than developing new medicines for non-infectious diseases. Unlike the more chronic conditions like diabetes or cancer that require long-term medications, infectious diseases are usually treated much quicker. Running clinical trials are expensive and antibiotic-alternatives aren’t lucrative enough.
“Unfortunately, new medications for antibiotic resistant infections have been pushed to the bottom of the field,” says Lu of MIT. “It's not because the technology does not work. This is more of a market issue. Because clinical trials cost hundreds of millions of dollars, the only solution is that governments will need to fund them.” Lu stresses that societies must lobby to change how the modern healthcare industry works. “The whole world needs better treatments for antibiotic resistance.”
Podcast: Should Scientific Controversies Be Silenced?
The recent Joe Rogan/Spotify controversy prompts the consideration of tough questions about expertise, trust, gatekeepers, and dissent.
The "Making Sense of Science" podcast features interviews with leading medical and scientific experts about the latest developments and the big ethical and societal questions they raise. This monthly podcast is hosted by journalist Kira Peikoff, founding editor of the award-winning science outlet Leaps.org.
The recent Joe Rogan/Spotify backlash over the misinformation presented in his recent episode on the Covid-19 vaccines raises some difficult and important bioethical questions for society: How can people know which experts to trust? What should big tech gatekeepers do about false claims promoted on their platforms? How should the scientific establishment respond to heterodox viewpoints from experts who disagree with the consensus? When is silencing of dissent merited, and when is it problematic? Journalist Kira Peikoff asks infectious disease physician and pandemic scholar Dr. Amesh Adalja to weigh in.

Dr. Amesh Adalja, Senior Scholar, Johns Hopkins Center for Health Security and an infectious disease physician
Listen to the Episode
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Scientists Are Studying How to Help Dogs Have Longer Lives, in a Bid to Further Our Own
Feeding dogs only once a day is showing health benefits in a large study, scientists report.
The sad eyes. The wagging tail. The frustrated whine. The excited bark. Dogs know how to get their owners to fork over the food more often.
The extra calories dogs get from feeding patterns now used by many Americans may not be good for them from a health and longevity viewpoint. In research from a large study called the Dog Aging Project, canines fed once a day had better scores on cognition tests and lower odds of developing diseases of organs throughout the body: intestinal tract, mouth and teeth, bones and joints, kidneys and bladder, and liver and pancreas.
Fewer than 1 in 10 dog owners fed their furry friends once daily, while nearly three fourths provided two daily meals.
“Most veterinarians have been led to believe that feeding dogs twice a day is optimal, but this is a relatively new idea that has developed over the past few decades with little supportive evidence from a health standpoint,” said Matt Kaeberlein, PhD, Co-Director of the Dog Aging Project, a professor of pathology and Director of the Healthy Aging and Longevity Research Institute at the University of Washington. Kaeberlein studies basic mechanisms of aging to find ways of extending the healthspan, the number of years of life lived free of disease. It’s not enough to extend the lifespan unless declines in biological function and risks of age-related diseases are also studied, he believes, hence the healthspan.
The Dog Aging Project is studying tens of thousands of dogs living with their owners in the real world, not a biology laboratory. The feeding study is the first of several reports now coming from the project based on owners’ annual reports of demographics, physical activity, environment, dog behavior, diet, medications and supplements, and health status. It has been posted on bioRxiv as it goes through peer review.
“All available evidence suggests that most biological mechanisms of aging in dogs will be conserved in humans. It just happens much faster in dogs.”
“The Dog Aging Project is one of the most exciting in the longevity space,” said David A. Sinclair, professor in the Department of Genetics and co-director of the Paul F. Glenn Center for Biology of Aging Research at Harvard Medical School. “Not only is it important to help our companions live longer and healthier, but because they are like people and share the same environment and many of the lifestyles as their owners, they are the perfect model for human longevity interventions.”
The epigenetic clock — and specifically changes in gene expression resulting from methylation of cytosine and guanine in the DNA — provides the critical connection between aging in dogs and people. “All available evidence suggests that most biological mechanisms of aging in dogs will be conserved in humans,” Kaeberlein said. “It just happens much faster in dogs.” These methylation changes, called the “methylomes,” have been associated with rates of aging in dogs, humans, and also mice.
In a 2020 study young dogs matched with young adults and aged dogs matched with older adults showed the greatest similarities in methylomes. In the Cell Systems report, Tina Wang of the University of California, San Diego, and colleagues wrote that the methylome “can be used to quantitatively translate the age-related physiology experienced by one organism (i.e., a model species like dog) to the age at which physiology in a second organism is most similar (i.e., a second model or humans).” This allows rates of aging in one species to be mapped onto aging in another species, providing “a compelling tool in the quest to understand aging and identify interventions for maximizing healthy lifespan.”
In the Dog Aging Project study, 8% of 24,238 owners fed their dogs once daily, the same as the percentage of owners serving three daily meals. Twice-daily feedings were most common (73%), and just over 1 in 10 owners (11%) “free fed” their dogs by just filling up the bowl whenever it was empty — most likely Rover’s favorite option.
“The notion of breakfast, lunch, and dinner for people in the United States is not based on large studies that compared three meals a day to two meals a day, or to four, “ said Kate E. Creevy, chief veterinary officer with the Dog Aging Project and associate professor at Texas A&M University. “It’s more about what we are accustomed to. Similarly, there are not large population studies comparing outcomes of dogs fed once, twice, or three times a day.”
“We do not recommend that people change their dogs’ diets based on this report,” Creevy emphasized. “It’s important to understand the difference between research that finds associations versus research that finds cause and effect.”
To establish cause and effect, the Dog Aging Project will follow their cohort over many years. Then, Creevy said, “We will be able to determine whether the associations we have found with feeding frequency are causes, or effects, or neither.”
While not yet actionable, the feeding findings fit with biology across a variety of animals, Kaeberlein said, including indicators that better health translates into longer healthspans. He said that caloric restriction and perhaps time-restricted eating or intermittent fasting — all ways that some human diets are structured — can have a positive impact on the biology of aging by allowing the gastrointestinal tract to have time each day to rest and repair itself, just as sleep benefits the brain through rest.
Timing of meals is also related to the concept of ketogenesis, Kaeberlein explained. Without access to glucose, animals switch over to a ketogenic state in which back-up systems produce energy through metabolic pathways that generate ketones. Mice go into this state very quickly, after a few hours or an overnight fast, while people shift to ketogenesis more slowly, from a few hours to up to 36 hours for people on typical Western diets, Kaeberlein said.
Dogs are different. They take at least two days to shift to ketogenesis, suggesting they have evolved to need fewer meals that are spaced out rather than the multiple daily meals plus snacks that people prefer.
As this relates to longevity, Kaeberlein said that a couple of studies show that mice who are fed a ketogenic diet have longer lifespans (years of life regardless of health). “For us, the next step is to analyze the composition of the dogs’ diets or the relationship of multiple daily feedings with obesity,” he said. “Maybe not being obese is related to better health.”
To learn more, the Dog Aging Project needs dogs — lots of dogs! Kaeberlein wants at least 100,000 dogs, including small dogs, large dogs, dogs of all ages. Puppies are needed for the researchers to follow across their lifespan. The project has an excellent website where owners can volunteer to participate.
Nutritional strategies are often not built around sound scientific principles, Kaeberlein said. In human nutrition, people have tried all kinds of diets over the years, including some that were completely wrong. Kaeberlein and his colleagues in the Dog Aging Project want to change that, at least for people’s canine companions, and hopefully, as a result, give dogs added years of healthy life and provide clues for human nutrition.
After that, maybe they can do something about those sad eyes and the frustrated whine.

