Scientists redesign bacteria to tackle the antibiotic resistance crisis
Probiotic bacteria can be engineered to fight antibiotic-resistant superbugs by releasing chemicals that kill them.
In 1945, almost two decades after Alexander Fleming discovered penicillin, he warned that as antibiotics use grows, they may lose their efficiency. He was prescient—the first case of penicillin resistance was reported two years later. Back then, not many people paid attention to Fleming’s warning. After all, the “golden era” of the antibiotics age had just began. By the 1950s, three new antibiotics derived from soil bacteria — streptomycin, chloramphenicol, and tetracycline — could cure infectious diseases like tuberculosis, cholera, meningitis and typhoid fever, among others.
Today, these antibiotics and many of their successors developed through the 1980s are gradually losing their effectiveness. The extensive overuse and misuse of antibiotics led to the rise of drug resistance. The livestock sector buys around 80 percent of all antibiotics sold in the U.S. every year. Farmers feed cows and chickens low doses of antibiotics to prevent infections and fatten up the animals, which eventually causes resistant bacterial strains to evolve. If manure from cattle is used on fields, the soil and vegetables can get contaminated with antibiotic-resistant bacteria. Another major factor is doctors overprescribing antibiotics to humans, particularly in low-income countries. Between 2000 to 2018, the global rates of human antibiotic consumption shot up by 46 percent.
In recent years, researchers have been exploring a promising avenue: the use of synthetic biology to engineer new bacteria that may work better than antibiotics. The need continues to grow, as a Lancet study linked antibiotic resistance to over 1.27 million deaths worldwide in 2019, surpassing HIV/AIDS and malaria. The western sub-Saharan Africa region had the highest death rate (27.3 people per 100,000).
Researchers warn that if nothing changes, by 2050, antibiotic resistance could kill 10 million people annually.
To make it worse, our remedy pipelines are drying up. Out of the 18 biggest pharmaceutical companies, 15 abandoned antibiotic development by 2013. According to the AMR Action Fund, venture capital has remained indifferent towards biotech start-ups developing new antibiotics. In 2019, at least two antibiotic start-ups filed for bankruptcy. As of December 2020, there were 43 new antibiotics in clinical development. But because they are based on previously known molecules, scientists say they are inadequate for treating multidrug-resistant bacteria. Researchers warn that if nothing changes, by 2050, antibiotic resistance could kill 10 million people annually.
The rise of synthetic biology
To circumvent this dire future, scientists have been working on alternative solutions using synthetic biology tools, meaning genetically modifying good bacteria to fight the bad ones.
From the time life evolved on earth around 3.8 billion years ago, bacteria have engaged in biological warfare. They constantly strategize new methods to combat each other by synthesizing toxic proteins that kill competition.
For example, Escherichia coli produces bacteriocins or toxins to kill other strains of E.coli that attempt to colonize the same habitat. Microbes like E.coli (which are not all pathogenic) are also naturally present in the human microbiome. The human microbiome harbors up to 100 trillion symbiotic microbial cells. The majority of them are beneficial organisms residing in the gut at different compositions.
The chemicals that these “good bacteria” produce do not pose any health risks to us, but can be toxic to other bacteria, particularly to human pathogens. For the last three decades, scientists have been manipulating bacteria’s biological warfare tactics to our collective advantage.
In the late 1990s, researchers drew inspiration from electrical and computing engineering principles that involve constructing digital circuits to control devices. In certain ways, every cell in living organisms works like a tiny computer. The cell receives messages in the form of biochemical molecules that cling on to its surface. Those messages get processed within the cells through a series of complex molecular interactions.
Synthetic biologists can harness these living cells’ information processing skills and use them to construct genetic circuits that perform specific instructions—for example, secrete a toxin that kills pathogenic bacteria. “Any synthetic genetic circuit is merely a piece of information that hangs around in the bacteria’s cytoplasm,” explains José Rubén Morones-Ramírez, a professor at the Autonomous University of Nuevo León, Mexico. Then the ribosome, which synthesizes proteins in the cell, processes that new information, making the compounds scientists want bacteria to make. “The genetic circuit remains separated from the living cell’s DNA,” Morones-Ramírez explains. When the engineered bacteria replicates, the genetic circuit doesn’t become part of its genome.
Highly intelligent by bacterial standards, some multidrug resistant V. cholerae strains can also “collaborate” with other intestinal bacterial species to gain advantage and take hold of the gut.
In 2000, Boston-based researchers constructed an E.coli with a genetic switch that toggled between turning genes on and off two. Later, they built some safety checks into their bacteria. “To prevent unintentional or deleterious consequences, in 2009, we built a safety switch in the engineered bacteria’s genetic circuit that gets triggered after it gets exposed to a pathogen," says James Collins, a professor of biological engineering at MIT and faculty member at Harvard University’s Wyss Institute. “After getting rid of the pathogen, the engineered bacteria is designed to switch off and leave the patient's body.”
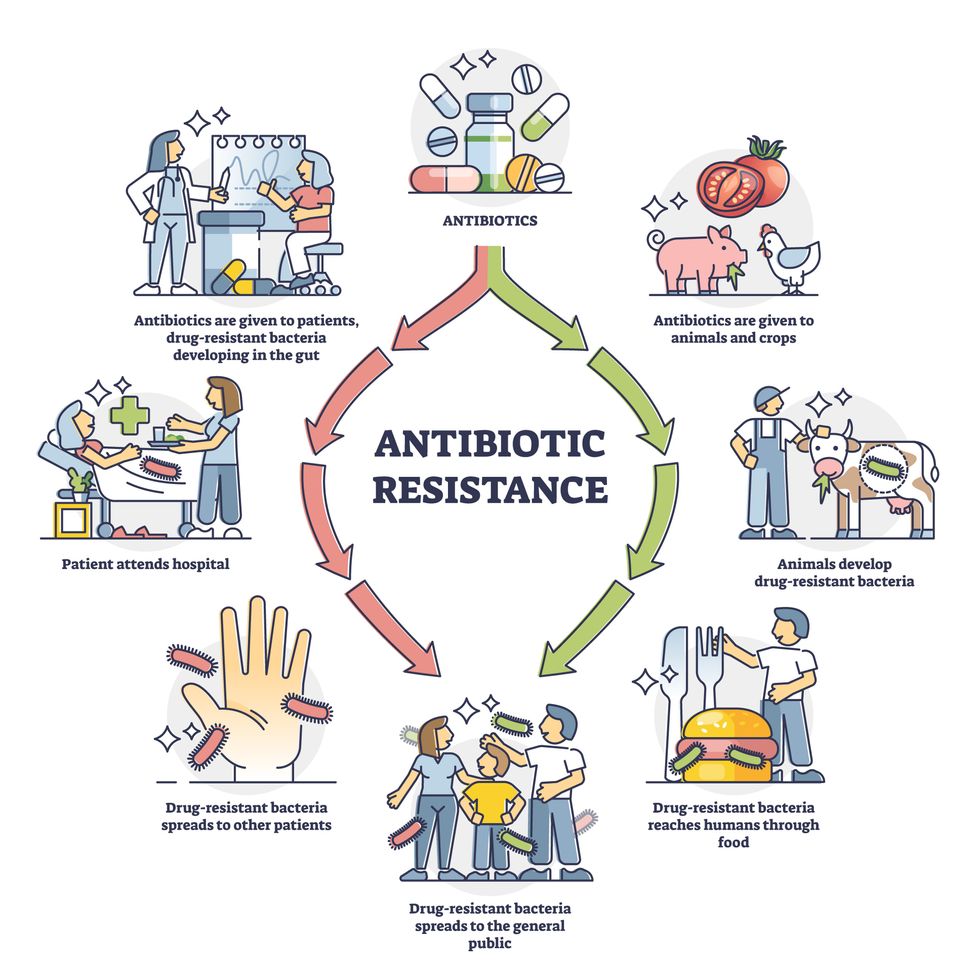
Overuse and misuse of antibiotics causes resistant strains to evolve
Adobe Stock
Seek and destroy
As the field of synthetic biology developed, scientists began using engineered bacteria to tackle superbugs. They first focused on Vibrio cholerae, which in the 19th and 20th century caused cholera pandemics in India, China, the Middle East, Europe, and Americas. Like many other bacteria, V. cholerae communicate with each other via quorum sensing, a process in which the microorganisms release different signaling molecules, to convey messages to its brethren. Highly intelligent by bacterial standards, some multidrug resistant V. cholerae strains can also “collaborate” with other intestinal bacterial species to gain advantage and take hold of the gut. When untreated, cholera has a mortality rate of 25 to 50 percent and outbreaks frequently occur in developing countries, especially during floods and droughts.
Sometimes, however, V. cholerae makes mistakes. In 2008, researchers at Cornell University observed that when quorum sensing V. cholerae accidentally released high concentrations of a signaling molecule called CAI-1, it had a counterproductive effect—the pathogen couldn’t colonize the gut.
So the group, led by John March, professor of biological and environmental engineering, developed a novel strategy to combat V. cholerae. They genetically engineered E.coli to eavesdrop on V. cholerae communication networks and equipped it with the ability to release the CAI-1 molecules. That interfered with V. cholerae progress. Two years later, the Cornell team showed that V. cholerae-infected mice treated with engineered E.coli had a 92 percent survival rate.
These findings inspired researchers to sic the good bacteria present in foods like yogurt and kimchi onto the drug-resistant ones.
Three years later in 2011, Singapore-based scientists engineered E.coli to detect and destroy Pseudomonas aeruginosa, an often drug-resistant pathogen that causes pneumonia, urinary tract infections, and sepsis. Once the genetically engineered E.coli found its target through its quorum sensing molecules, it then released a peptide, that could eradicate 99 percent of P. aeruginosa cells in a test-tube experiment. The team outlined their work in a Molecular Systems Biology study.
“At the time, we knew that we were entering new, uncharted territory,” says lead author Matthew Chang, an associate professor and synthetic biologist at the National University of Singapore and lead author of the study. “To date, we are still in the process of trying to understand how long these microbes stay in our bodies and how they might continue to evolve.”
More teams followed the same path. In a 2013 study, MIT researchers also genetically engineered E.coli to detect P. aeruginosa via the pathogen’s quorum-sensing molecules. It then destroyed the pathogen by secreting a lab-made toxin.
Probiotics that fight
A year later in 2014, a Nature study found that the abundance of Ruminococcus obeum, a probiotic bacteria naturally occurring in the human microbiome, interrupts and reduces V.cholerae’s colonization— by detecting the pathogen’s quorum sensing molecules. The natural accumulation of R. obeum in Bangladeshi adults helped them recover from cholera despite living in an area with frequent outbreaks.
The findings from 2008 to 2014 inspired Collins and his team to delve into how good bacteria present in foods like yogurt and kimchi can attack drug-resistant bacteria. In 2018, Collins and his team developed the engineered probiotic strategy. They tweaked a bacteria commonly found in yogurt called Lactococcus lactis to treat cholera.
Engineered bacteria can be trained to target pathogens when they are at their most vulnerable metabolic stage in the human gut. --José Rubén Morones-Ramírez.
More scientists followed with more experiments. So far, researchers have engineered various probiotic organisms to fight pathogenic bacteria like Staphylococcus aureus (leading cause of skin, tissue, bone, joint and blood infections) and Clostridium perfringens (which causes watery diarrhea) in test-tube and animal experiments. In 2020, Russian scientists engineered a probiotic called Pichia pastoris to produce an enzyme called lysostaphin that eradicated S. aureus in vitro. Another 2020 study from China used an engineered probiotic bacteria Lactobacilli casei as a vaccine to prevent C. perfringens infection in rabbits.
In a study last year, Ramírez’s group at the Autonomous University of Nuevo León, engineered E. coli to detect quorum-sensing molecules from Methicillin-resistant Staphylococcus aureus or MRSA, a notorious superbug. The E. coli then releases a bacteriocin that kills MRSA. “An antibiotic is just a molecule that is not intelligent,” says Ramírez. “On the other hand, engineered bacteria can be trained to target pathogens when they are at their most vulnerable metabolic stage in the human gut.”
Collins and Timothy Lu, an associate professor of biological engineering at MIT, found that engineered E. coli can help treat other conditions—such as phenylketonuria, a rare metabolic disorder, that causes the build-up of an amino acid phenylalanine. Their start-up Synlogic aims to commercialize the technology, and has completed a phase 2 clinical trial.
Circumventing the challenges
The bacteria-engineering technique is not without pitfalls. One major challenge is that beneficial gut bacteria produce their own quorum-sensing molecules that can be similar to those that pathogens secrete. If an engineered bacteria’s biosensor is not specific enough, it will be ineffective.
Another concern is whether engineered bacteria might mutate after entering the gut. “As with any technology, there are risks where bad actors could have the capability to engineer a microbe to act quite nastily,” says Collins of MIT. But Collins and Ramírez both insist that the chances of the engineered bacteria mutating on its own are virtually non-existent. “It is extremely unlikely for the engineered bacteria to mutate,” Ramírez says. “Coaxing a living cell to do anything on command is immensely challenging. Usually, the greater risk is that the engineered bacteria entirely lose its functionality.”
However, the biggest challenge is bringing the curative bacteria to consumers. Pharmaceutical companies aren’t interested in antibiotics or their alternatives because it’s less profitable than developing new medicines for non-infectious diseases. Unlike the more chronic conditions like diabetes or cancer that require long-term medications, infectious diseases are usually treated much quicker. Running clinical trials are expensive and antibiotic-alternatives aren’t lucrative enough.
“Unfortunately, new medications for antibiotic resistant infections have been pushed to the bottom of the field,” says Lu of MIT. “It's not because the technology does not work. This is more of a market issue. Because clinical trials cost hundreds of millions of dollars, the only solution is that governments will need to fund them.” Lu stresses that societies must lobby to change how the modern healthcare industry works. “The whole world needs better treatments for antibiotic resistance.”
An Investigational Drug Offers Hope to Patients with a Disabling Neuromuscular Disease
Robert Thomas was a devoted runner, gym goer, and crew member on a sailing team in San Diego when, in his 40s, he noticed that his range of movement was becoming more limited.
He thought he was just getting older, but when he was hiking an uphill trail in Lake Tahoe, he kept tripping over rocks. "I'd never had this happen before," Robert says. "I knew something was wrong but didn't know what it was."
It wasn't until age 50 when he was diagnosed with Charcot-Marie-Tooth disease. The genetic disorder damages the peripheral nerves, which connect the brain and spinal cord to the rest of the body. This network of nerves is responsible for relaying information and signals about sensation, movement, and motor coordination. Over time, the disease causes debilitating muscle weakness and the loss of limb control.
Charcot-Marie-Tooth usually presents itself in childhood or in a person's teens, but in some patients, like Robert, onset can be later in life. Symptoms may include muscle cramping, tingling, or burning. Many patients also have high foot arches or hammer toes — toes that curl from the middle joint instead of pointing forward. Those affected often have difficulty walking and may lose sensation in their lower legs, feet, hands, or forearms. One of the most common rare diseases, it affects around 130,000 people in the United States and 2.8 million worldwide.
Like many people with Charcot-Marie-Tooth, or CMT, Robert wears corrective braces on his legs to help with walking. Now 61, he can't run or sail anymore because of the disease, but he still works out regularly and can hike occasionally. CMT also affects his grip, so he has to use special straps while doing some exercises.
For the past few years, Robert has been participating in a clinical trial for an investigational CMT drug. He takes the liquid formulation every morning and evening using an oral syringe. Scientists are following patients like Robert to learn if their symptoms stabilize or improve while on the drug. Dubbed PXT300, the drug was designed by French biopharmaceutical company Pharnext and is the farthest along in development for CMT. If approved, it would be the first drug for the disease.
Currently, there's no cure for CMT, only supportive treatments like pain medication. Some individuals receive physical and occupational therapy. A drug for CMT could be a game-changer for patients whose quality of life is severely affected by the disease.
Genetic Underpinnings
CMT arises from mutations in genes that are responsible for creating and maintaining the myelin sheath — the insulating layer around nerves. Pharnext's drug is meant to treat patients with CMT1A, the most common form of the disease, which represents about half of CMT cases. Around 5% of those with CMT1A become severely disabled and end up in wheelchairs. People with CMT1A have an extra copy of the gene PMP22, which makes a protein that's needed to maintain the myelin sheath around peripheral nerves.
Typically, an individual inherits one copy of PMP22 from each parent. But a person with CMT1A receives a copy of PMP22 from one parent and two copies from a parent with the disease. This extra copy of the gene results in excess protein production, which damages the cells responsible for preserving and regenerating the myelin sheath, called Schwann cells.
The myelin sheath helps ensure that a signal from the brain gets carried to nerves in the muscles so that a part of the body can carry out a particular action or movement. This sheath is like the insulation on an electrical cord and the action is like a light bulb. If the insulation is fine, the light bulb turns on. But if the insulation is frayed, the light will flicker.
"The same happens to these patients," says David Horn Solomon, CEO of Pharnext. "The signal to their muscle is weak and flickers." Over time, their muscles become weaker and thinner.
The PMP22 gene has proven difficult to target with a drug because it's located in a protected space — the Schwann cells that make up the insulation around nerves. "There's not an easy way to tamp it down," Solomon says.
Another company, Acceleron Pharma of Cambridge, Massachusetts, was developing an injectable CMT drug meant to increase the strength of leg muscles. But the company halted development last year after the experimental drug failed in a mid-stage trial. While the drug led to a statistically significant increase in muscle volume, it didn't translate to improvements in muscle function or quality of life for trial participants.
Made by Design
Pharnext's drug, PXT3003, is a combination of three existing drugs — baclofen, a muscle relaxant; naltrexone, a drug that decreases the desire for alcohol and opioids; and sorbitol, a type of sugar alcohol.
The company designed the drug using its artificial intelligence platform, which screened 20,000 existing drugs to predict combinations that could inhibit the PMP22 gene and thereby lower protein production. The AI system narrowed the search to several hundreds of combinations and Pharnext tested around 75 of them in the lab before landing on baclofen, naltrexone, and sorbitol. Individually, the drugs don't have much effect on the PMP22 gene. But combined, they work to lower how much protein the gene makes.
"How the drug inside the cell reduces expression isn't quite clear yet," says Florian Thomas, director of the Hereditary Neuropathy Center, and founding chair and professor in the department of neurology at Hackensack University Medical Center and Hackensack Meridian School of Medicine in New Jersey (no relation to Robert Thomas, the CMT patient). "By reducing the amount of protein being produced, we hopefully can stabilize the nerves."
In rodents genetically engineered to have the PMP22 gene, the drug reduced protein levels and delayed onset of muscle weakness when given to rats. In another animal study, the drug increased the size of the myelin sheath around nerves in rats.
"Like humans with CMT, one of the problems the animals have is they can't grip things, their grip strength is poor," Solomon says. But when treated with Pharnext's drug, "the grip strength of these animals improves dramatically even over 12 weeks."
Human trials look encouraging, too. But the company ran into a manufacturing issue during a late-stage trial. The drug requires refrigeration, and as a result of temperature changes, crystals formed inside vials containing the high dose of the drug. The study was a double-blind trial, meaning neither the trial participants nor investigators were supposed to know who received the high dose of the drug, who received the low dose, and who received a placebo. In these types of studies, the placebo and experimental drug should look the same so that investigators can't tell them apart. But because only the high dose contained crystals, not the low dose or placebo, regulators said the trial data could be biased.
Pharnext is now conducting a new randomized, double-blind trial to prove that its drug works. The study is recruiting individuals aged 16 through 65 years old with mild to moderate CMT. The company hopes to show that the drug can stop patients' symptoms from worsening, or in the best case scenario, possibly even improve them. The company doesn't think the drug will be able to help people with severe forms of the disease.
"In neurologic disease, you're looking for plasticity, where there's still the possibility of stabilization or reversal," Solomon says. Plasticity refers to the ability of the nervous system to change and adapt in response to stimuli.
Preventing Disability
Allison Moore, a CMT patient and founder and CEO of the Hereditary Neuropathy Foundation, has been following drug development for CMT since she founded the organization in 2001. She says many investigational drugs haven't moved forward because they've shown little success in animals. The fact that Pharnext's drug has made it to a late-stage human trial is promising, she says.
"It's really exciting," Moore says. "There's a chance that if you take the drug early before you're very severe, you'll end up not developing the disease to a level that's super disabling."
CMT has damaged Moore's peroneal nerve, a main nerve in the foot. As a result, she has foot drop, the inability to lift the front part of her foot, and needs to wear leg braces to help her walk. "The idea that you could take this early on and that it could stop progression, that's the hope that we have."
Thomas, the neurologist, says a drug doesn't have to be a cure to have a significant impact on patients. "If I have a CMT patient who's 50 years old, that patient will be more disabled by age 60," he says. "If I can treat that person with a drug, and that person is just as disabled at age 60 as they were at age 50, that's transformative in my mind."
While Robert Thomas says he hasn't noticed a dramatic improvement since he's been on the drug, he does think it's helping. Robert is now in an open-label study, which means he and his health provider are aware that he's receiving the drug.
When the COVID-19 pandemic hit, manufacturing and supply chain disruptions meant that Robert was without the trial drug for two months. When his medication ran out, his legs felt unstable again and walking was harder. "There was a clear distinction between being on and off that medication," he says.
Pharnext's current trial will take about a year and a half to complete. After that, the FDA will decide on whether to approve the drug for CMT patients.
As scientists learn more about the PMP22 gene and the more than 100 other genes that when mutated cause CMT, more precise treatments could be possible. For instance, scientists have used the gene-editing tool CRISPR to correct a CMT-causing mutation in human cells in the lab. The results were published August 16 in the journal Frontiers in Cell and Developmental Biology.
Pharnext is also interested in pursuing genetic treatments for CMT, but in the meantime, repurposed drugs may be the best shot at helping patients until more advanced treatments are available.
"Making Sense of Science" is a monthly podcast that features interviews with leading medical and scientific experts about the latest developments and the big ethical and societal questions they raise. This episode is hosted by science and biotech journalist Emily Mullin, summer editor of the award-winning science outlet Leaps.org.

