Antibody Testing Alone is Not the Key to Re-Opening Society
Immunity tests have too many unknowns right now to make them very useful in determining protective antibody status.
[Editor's Note: We asked experts from different specialties to weigh in on a timely Big Question: "How should immunity testing play a role in re-opening society?" Below, a virologist offers her perspective.]
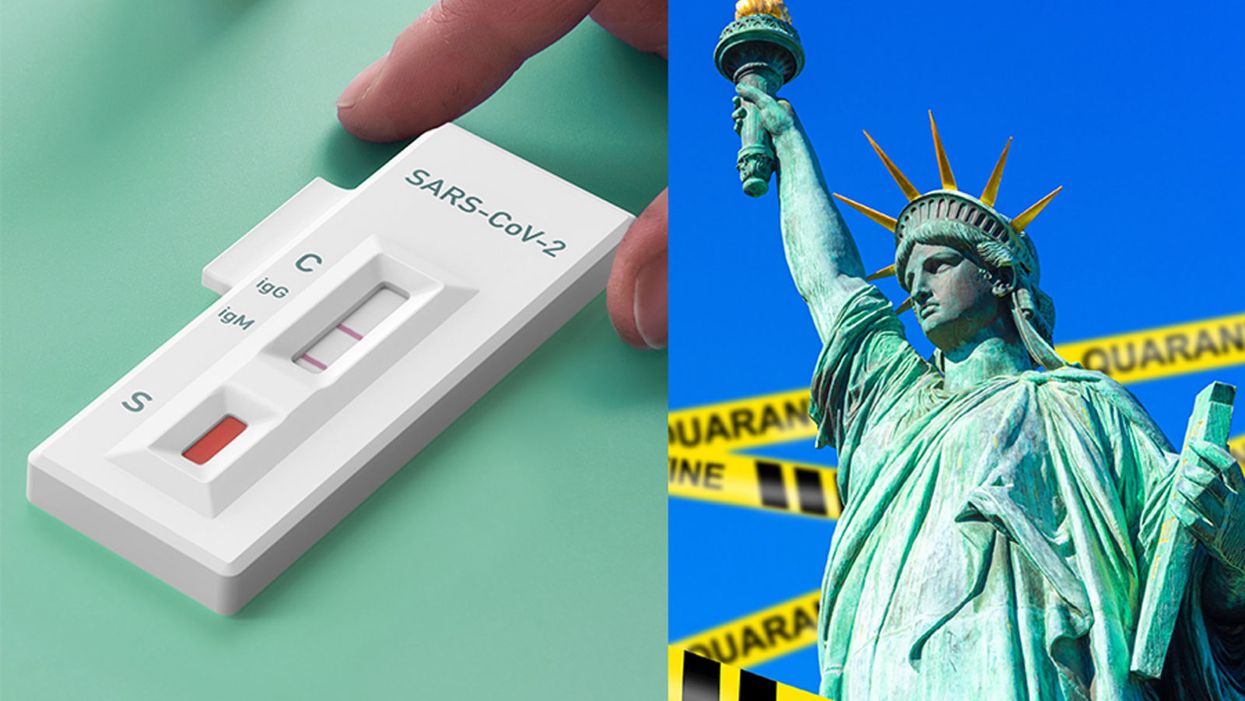
With the advent of serology testing and increased emphasis on "re-opening" America, public health officials have begun considering whether or not people who have recovered from COVID-19 can safely re-enter the workplace.
"Immunity certificates cannot certify what is not known."
Conventional wisdom holds that people who have developed antibodies in response to infection with SARS-CoV-2, the coronavirus that causes COVID-19, are likely to be immune to reinfection.
For most acute viral infections, this is generally true. However, SARS-CoV-2 is a new pathogen, and there are currently many unanswered questions about immunity. Can recovered patients be reinfected or transmit the virus? Does symptom severity determine how protective responses will be after recovery? How long will protection last? Understanding these basic features is essential to phased re-opening of the government and economy for people who have recovered from COVID-19.
One mechanism that has been considered is issuing "immunity certificates" to individuals with antibodies against SARS-CoV-2. These certificates would verify that individuals have already recovered from COVID-19, and thus have antibodies in their blood that will protect them against reinfection, enabling them to safely return to work and participate in society. Although this sounds reasonable in theory, there are many practical reasons why this is not a wise policy decision to ease off restrictive stay-home orders and distancing practices.
Too Many Scientific Unknowns
Serology tests measure antibodies in the serum—the liquid component of blood, which is where the antibodies are located. In this case, serology tests measure antibodies that specifically bind to SARS-CoV-2 virus particles. Usually when a person is infected with a virus, they develop antibodies that can "recognize" that virus, so the presence of SARS-CoV-2 antibodies indicates that a person has been previously exposed to the virus. Broad serology testing is critical to knowing how many people have been infected with SARS-CoV-2, since testing capacity for the virus itself has been so low.
Tests for the virus measure amounts of SARS-CoV-2 RNA—the virus's genetic material—directly, and thus will not detect the virus once a person has recovered. Thus, the majority of people who were not severely ill and did not require hospitalization, or did not have direct contact with a confirmed case, will not test positive for the virus weeks after they have recovered and can only determine if they had COVID-19 by testing for antibodies.
In most cases, for most pathogens, antibodies are also neutralizing, meaning they bind to the virus and render it incapable of infecting cells, and this protects against future infections. Immunity certificates are based on the assumption that people with antibodies specific for SARS-CoV-2 will be protected against reinfection. The problem is that we've only known that SARS-CoV-2 existed for a little over four months. Although studies so far indicate that most (but not all) patients with confirmed COVID-19 cases develop antibodies, we don't know the extent to which antibodies are protective against reinfection, or how long that protection will last. Immunity certificates cannot certify what is not known.
The limited data so far is encouraging with regard to protective immunity. Most of the patient sera tested for antibodies show reasonable titers of IgG, the type of antibodies most likely to be neutralizing. Furthermore, studies have shown that these IgG antibodies are capable of neutralizing surrogate viruses as well as infectious SARS-CoV-2 in laboratory tests. In addition, rhesus monkeys that were experimentally infected with SARS-CoV-2 and allowed to recover were protected from reinfection after a subsequent experimental challenge. These data tentatively suggest that most people are likely to develop neutralizing IgG, and protective immunity, after being infected by SARS-CoV-2.
However, not all COVID-19 patients do produce high levels of antibodies specific for SARS-CoV-2. A small number of patients in one study had no detectable neutralizing IgG. There have also been reports of patients in South Korea testing PCR positive after a prior negative test, indicating reinfection or reactivation. These cases may be explained by the sensitivity of the PCR test, and no data have been produced to indicate that these cases are genuine reinfection or recurrence of viral infection.
Complicating matters further, not all serology tests measure antibody titers. Some rapid serology tests are designed to be binary—the test can either detect antibodies or not, but does not give information about the amount of antibodies circulating. Based on our current knowledge, we cannot be certain that merely having any level of detectable antibodies alone guarantees protection from reinfection, or from a subclinical reinfection that might not cause a second case of COVID-19, but could still result in transmission to others. These unknowns remain problematic even with tests that accurately detect the presence of antibodies—which is not a given today, as many of the newly available tests are reportedly unreliable.
A Logistical and Ethical Quagmire
While most people are eager to cast off the isolation of physical distancing and resume their normal lives, mere desire to return to normality is not an indicator of whether those antibodies actually work, and no certificate can confer immune protection. Furthermore, immunity certificates could lead to some complicated logistical and ethical issues. If antibodies do not guarantee protective immunity, certifying that they do could give antibody-positive people a false sense of security, causing them to relax infection control practices such as distancing and hand hygiene.
"We should not, however, place our faith in assumptions and make return to normality contingent on an arbitrary and uninformative piece of paper."
Certificates could be forged, putting susceptible people at higher exposure risk. It's not clear who would issue them, what they would entitle the bearer to do or not do, or how certification would be verified or enforced. There are many ways in which such certificates could be used as a pretext to discriminate against people based on health status, in addition to disability, race, and socioeconomic status. Tracking people based on immune status raises further concerns about privacy and civil rights.
Rather than issuing documents confirming immune status, we should instead "re-open" society cautiously, with widespread virus and serology testing to accurately identify and isolate infected cases rapidly, with immediate contact tracing to safely quarantine and monitor those at exposure risk. Broad serosurveillance must be coupled with functional assays for neutralization activity to begin assessing how protective antibodies might actually be against SARS-CoV-2 infection. To understand how long immunity lasts, we should study antibodies, as well as the functional capabilities of other components of the larger immune system, such as T cells, in recovered COVID-19 patients over time.
We should not, however, place our faith in assumptions and make return to normality contingent on an arbitrary and uninformative piece of paper. Re-opening society, the government, and the economy depends not only on accurately determining how many people have antibodies to SARS-CoV-2, but on a deeper understanding of how those antibodies work to provide protection.
A new type of cancer therapy is shrinking deadly brain tumors with just one treatment
MRI scans after a new kind of immunotherapy for brain cancer show remarkable progress in one patient just days after the first treatment.
Few cancers are deadlier than glioblastomas—aggressive and lethal tumors that originate in the brain or spinal cord. Five years after diagnosis, less than five percent of glioblastoma patients are still alive—and more often, glioblastoma patients live just 14 months on average after receiving a diagnosis.
But an ongoing clinical trial at Mass General Cancer Center is giving new hope to glioblastoma patients and their families. The trial, called INCIPIENT, is meant to evaluate the effects of a special type of immune cell, called CAR-T cells, on patients with recurrent glioblastoma.
How CAR-T cell therapy works
CAR-T cell therapy is a type of cancer treatment called immunotherapy, where doctors modify a patient’s own immune system specifically to find and destroy cancer cells. In CAR-T cell therapy, doctors extract the patient’s T-cells, which are immune system cells that help fight off disease—particularly cancer. These T-cells are harvested from the patient and then genetically modified in a lab to produce proteins on their surface called chimeric antigen receptors (thus becoming CAR-T cells), which makes them able to bind to a specific protein on the patient’s cancer cells. Once modified, these CAR-T cells are grown in the lab for several weeks so that they can multiply into an army of millions. When enough cells have been grown, these super-charged T-cells are infused back into the patient where they can then seek out cancer cells, bind to them, and destroy them. CAR-T cell therapies have been approved by the US Food and Drug Administration (FDA) to treat certain types of lymphomas and leukemias, as well as multiple myeloma, but haven’t been approved to treat glioblastomas—yet.
CAR-T cell therapies don’t always work against solid tumors, such as glioblastomas. Because solid tumors contain different kinds of cancer cells, some cells can evade the immune system’s detection even after CAR-T cell therapy, according to a press release from Massachusetts General Hospital. For the INCIPIENT trial, researchers modified the CAR-T cells even further in hopes of making them more effective against solid tumors. These second-generation CAR-T cells (called CARv3-TEAM-E T cells) contain special antibodies that attack EFGR, a protein expressed in the majority of glioblastoma tumors. Unlike other CAR-T cell therapies, these particular CAR-T cells were designed to be directly injected into the patient’s brain.
The INCIPIENT trial results
The INCIPIENT trial involved three patients who were enrolled in the study between March and July 2023. All three patients—a 72-year-old man, a 74-year-old man, and a 57-year-old woman—were treated with chemo and radiation and enrolled in the trial with CAR-T cells after their glioblastoma tumors came back.
The results, which were published earlier this year in the New England Journal of Medicine (NEJM), were called “rapid” and “dramatic” by doctors involved in the trial. After just a single infusion of the CAR-T cells, each patient experienced a significant reduction in their tumor sizes. Just two days after receiving the infusion, the glioblastoma tumor of the 72-year-old man decreased by nearly twenty percent. Just two months later the tumor had shrunk by an astonishing 60 percent, and the change was maintained for more than six months. The most dramatic result was in the 57-year-old female patient, whose tumor shrank nearly completely after just one infusion of the CAR-T cells.
The results of the INCIPIENT trial were unexpected and astonishing—but unfortunately, they were also temporary. For all three patients, the tumors eventually began to grow back regardless of the CAR-T cell infusions. According to the press release from MGH, the medical team is now considering treating each patient with multiple infusions or prefacing each treatment with chemotherapy to prolong the response.
While there is still “more to do,” says co-author of the study neuro-oncologist Dr. Elizabeth Gerstner, the results are still promising. If nothing else, these second-generation CAR-T cell infusions may someday be able to give patients more time than traditional treatments would allow.
“These results are exciting but they are also just the beginning,” says Dr. Marcela Maus, a doctor and professor of medicine at Mass General who was involved in the clinical trial. “They tell us that we are on the right track in pursuing a therapy that has the potential to change the outlook for this intractable disease.”
A recent study in The Lancet Oncology showed that AI found 20 percent more cancers on mammogram screens than radiologists alone.
Since the early 2000s, AI systems have eliminated more than 1.7 million jobs, and that number will only increase as AI improves. Some research estimates that by 2025, AI will eliminate more than 85 million jobs.
But for all the talk about job security, AI is also proving to be a powerful tool in healthcare—specifically, cancer detection. One recently published study has shown that, remarkably, artificial intelligence was able to detect 20 percent more cancers in imaging scans than radiologists alone.
Published in The Lancet Oncology, the study analyzed the scans of 80,000 Swedish women with a moderate hereditary risk of breast cancer who had undergone a mammogram between April 2021 and July 2022. Half of these scans were read by AI and then a radiologist to double-check the findings. The second group of scans was read by two researchers without the help of AI. (Currently, the standard of care across Europe is to have two radiologists analyze a scan before diagnosing a patient with breast cancer.)
The study showed that the AI group detected cancer in 6 out of every 1,000 scans, while the radiologists detected cancer in 5 per 1,000 scans. In other words, AI found 20 percent more cancers than the highly-trained radiologists.

But even though the AI was better able to pinpoint cancer on an image, it doesn’t mean radiologists will soon be out of a job. Dr. Laura Heacock, a breast radiologist at NYU, said in an interview with CNN that radiologists do much more than simply screening mammograms, and that even well-trained technology can make errors. “These tools work best when paired with highly-trained radiologists who make the final call on your mammogram. Think of it as a tool like a stethoscope for a cardiologist.”
AI is still an emerging technology, but more and more doctors are using them to detect different cancers. For example, researchers at MIT have developed a program called MIRAI, which looks at patterns in patient mammograms across a series of scans and uses an algorithm to model a patient's risk of developing breast cancer over time. The program was "trained" with more than 200,000 breast imaging scans from Massachusetts General Hospital and has been tested on over 100,000 women in different hospitals across the world. According to MIT, MIRAI "has been shown to be more accurate in predicting the risk for developing breast cancer in the short term (over a 3-year period) compared to traditional tools." It has also been able to detect breast cancer up to five years before a patient receives a diagnosis.
The challenges for cancer-detecting AI tools now is not just accuracy. AI tools are also being challenged to perform consistently well across different ages, races, and breast density profiles, particularly given the increased risks that different women face. For example, Black women are 42 percent more likely than white women to die from breast cancer, despite having nearly the same rates of breast cancer as white women. Recently, an FDA-approved AI device for screening breast cancer has come under fire for wrongly detecting cancer in Black patients significantly more often than white patients.
As AI technology improves, radiologists will be able to accurately scan a more diverse set of patients at a larger volume than ever before, potentially saving more lives than ever.

